Scope of Practice: What Healthcare Providers Can and Can't Do
When you see a doctor, nurse, or pharmacist for medication advice, you assume they know what they’re allowed to do—but not everyone has the same scope of practice, the legal boundaries that define what healthcare professionals are permitted to do based on their training and license. Also known as practice boundaries, it’s what keeps your care safe, legal, and properly supervised. A pharmacist can refill your prescription, but they can’t diagnose a new condition. A nurse practitioner might prescribe antibiotics, but only if their state allows it. These rules vary by location, profession, and even the setting you’re in—hospital, clinic, or pharmacy.
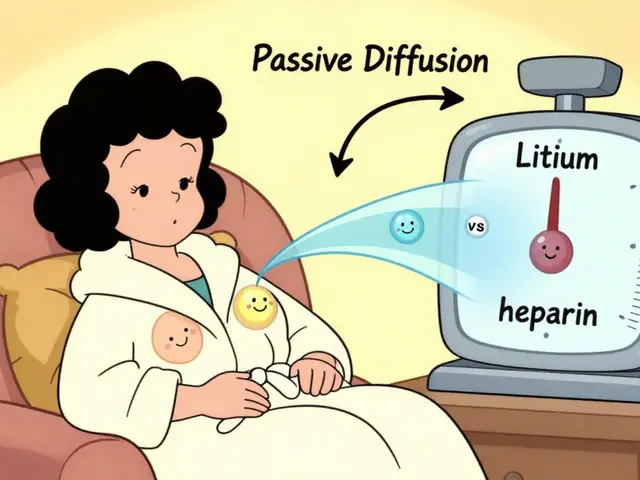
That’s why you might get different answers depending on who you ask. For example, prescribing rights, the legal authority to write prescriptions for medications aren’t the same across the board. In some places, physician assistants can prescribe almost anything a doctor can. In others, they need direct supervision. Even medication management, the process of tracking, adjusting, and monitoring drugs for safety and effectiveness has limits. A pharmacist might help you set up auto-refills or spot dangerous interactions, but they can’t change your dose without approval from your prescriber. These aren’t just paperwork rules—they directly affect how quickly you get help, what treatments you’re offered, and even whether you can get a generic version of your drug without another appointment.
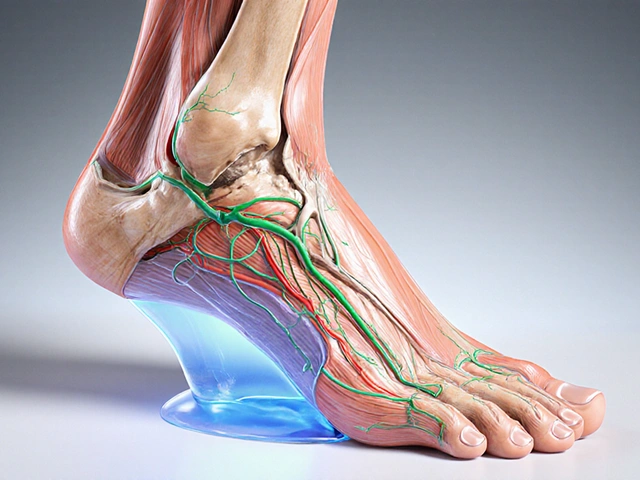
Look at the posts below. You’ll find real examples of how these boundaries play out. One article explains how app-based prescribing lets you get generic meds faster—but only if the platform is licensed to prescribe in your state. Another breaks down why some drugs like tacrolimus or verapamil require strict monitoring, and who’s allowed to adjust those doses. There’s even a piece on fall risk meds for seniors, where deprescribing isn’t just a suggestion—it’s a legal decision only certain providers can make. The differences between authorized generics and brand-name drugs? That’s a pharmacy question. But whether you can switch them without a new prescription? That’s a scope of practice issue.
Understanding scope of practice doesn’t mean you need to memorize state laws. It means knowing who to ask, when to push back, and why your care might look different from someone else’s—even if you have the same condition. The posts here show you how these rules shape your access to treatment, your ability to save money on meds, and how safely your drugs are managed. You’ll see what’s possible, what’s restricted, and why the person handing you your pills might not be the one who decided you needed them in the first place.