Massage Therapy Technique Selector
Find Your Best Massage Technique
Based on your condition and symptoms, we'll recommend the most appropriate massage therapy for edema relief.
Your Recommended Technique
Quick Takeaways
- Edema is fluid buildup that can be eased with specific massage techniques.
- Massage therapy improves blood and lymph flow, helping the body re‑absorb excess fluid.
- Lymphatic drainage, deep tissue massage, and myofascial release are the most effective styles for swelling relief.
- Professional guidance is essential when you have medical conditions like heart failure or venous insufficiency.
- Simple home‑hand techniques can complement professional sessions and keep circulation humming.
What Is Edema and Why Does It Matter?
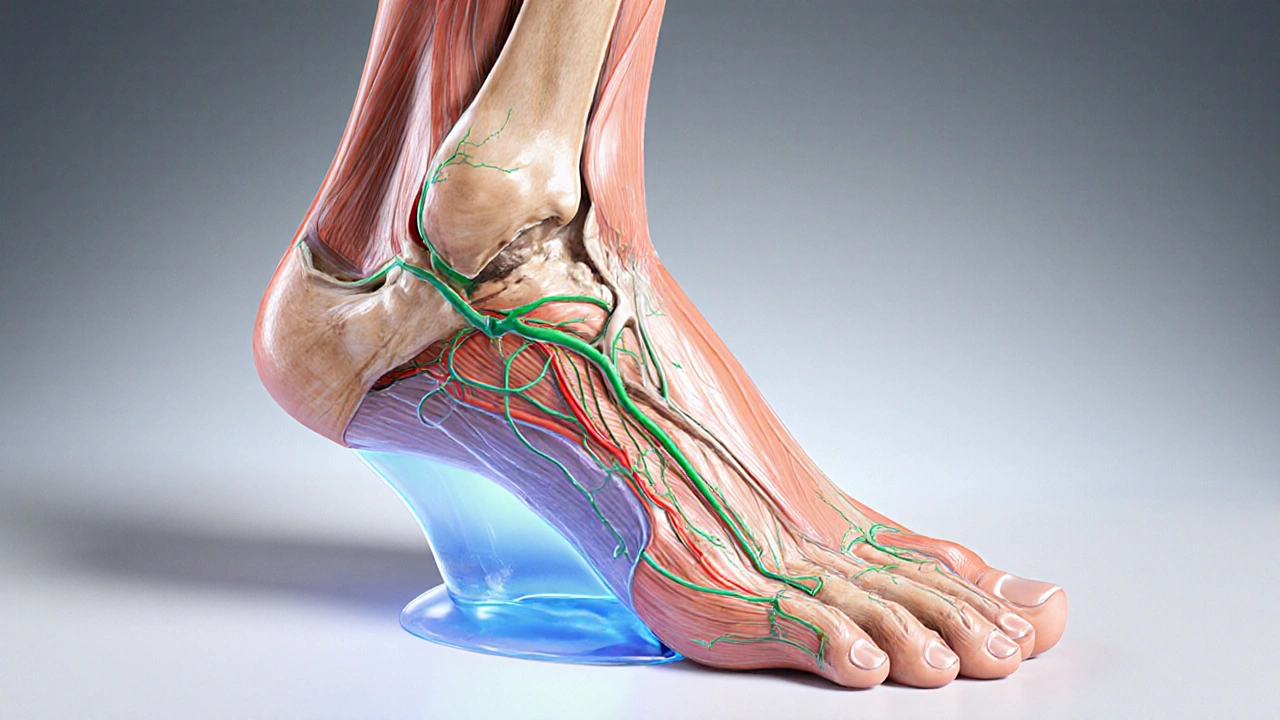
When fluid leaks out of blood vessels and settles in the tissues, you get edema is the medical term for swelling caused by excess interstitial fluid. The condition shows up in the ankles, feet, hands, or even the abdomen, and it can make everyday tasks feel heavy.
Common triggers include prolonged standing, a salty diet, pregnancy, and underlying health issues such as heart, kidney, or liver disease. The lymphatic system a network of vessels and nodes that moves lymph fluid back into circulation plays a starring role - when it stalls, fluid builds up.
How Massage Therapy Improves Circulation
Massage isn’t just a feel‑good indulgence; it creates mechanical pressure that pushes fluid through veins and lymph channels. This action does three things:
- Increases circulation the flow of blood through vessels delivering oxygen and nutrients, which helps re‑absorb the leaked fluid.
- Stimulates the lymphatic system enhancing the transport of lymphatic fluid toward the thoracic duct.
- Reduces the viscosity of interstitial fluid, making it easier for the body’s natural pumps to move it away.
Research from the Australian College of Sports Physicians (2023) showed that a 30‑minute lymphatic massage lowered ankle circumference by an average of 1.2cm in people with chronic venous insufficiency.

Top Massage Techniques for Edema Relief
Not all massages are created equal. Below is a quick comparison of the three most evidence‑based approaches.
| Technique | Pressure Level | Primary Goal | Best For |
|---|---|---|---|
| Lymphatic Drainage Massage | Very light, rhythmic strokes | Stimulate lymph flow | Post‑surgical swelling, lymphedema |
| Deep Tissue Massage | Medium‑to‑high, focused on muscle layers | Break up fibrotic tissue, improve venous return | Chronic edema from muscle tightness, athletes |
| Myofascial Release | Gentle sustained pressure | Release fascia restrictions, enhance fluid movement | Edema linked to scar tissue or post‑trauma |
When to Seek a Professional Massage Therapist
If you have any of the following, book a qualified practitioner before trying self‑massage:
- Heart failure, uncontrolled hypertension, or recent cardiac events.
- Severe varicose veins or diagnosed venous insufficiency.
- Lymphedema after cancer treatment.
- Painful or rapidly expanding swelling.
A professional massage therapist a certified practitioner trained in therapeutic techniques and contraindications will assess your medical history, choose the appropriate pressure, and integrate other modalities like compression garments if needed.
DIY Home Techniques to Boost Circulation
Even without a therapist, you can keep fluid moving with these simple moves. Perform them once or twice daily, especially after long periods of sitting or standing.
- Gentle pumping strokes. Using the flat of your hand, start at the foot and glide upward toward the heart in smooth, overlapping motions. Spend about 5minutes per leg.
- Self‑myofascial release with a foam roller. Lie on a foam roller under the calf, slowly roll up and down to loosen tight fascia. 1-2minutes per calf.
- Ankle circles. Rotate each ankle clockwise for 30seconds, then counter‑clockwise. This mobilises the peroneal veins and improves venous return.
- Leg elevation. Prop your legs on a pillow for 15-20minutes after a massage or a long day. Gravity helps fluid drain back toward the heart.
Pair these moves with a low‑sodium diet, regular walking, and proper hydration for best results.

Common Questions About Massage and Edema
Frequently Asked Questions
Can massage cause more swelling?
If the therapist uses too much pressure or works on an area with an active infection, swelling can temporarily increase. That’s why a qualified practitioner evaluates pressure levels and avoids inflamed zones.
How often should I get a lymphatic drainage session?
For chronic conditions, 2-3 sessions per week for the first month, then taper to weekly maintenance, works well. Adjust frequency based on your practitioner’s assessment.
Is massage safe during pregnancy?
Yes, as long as the therapist is trained in prenatal massage and avoids deep pressure on the abdomen and lower back. Light lymphatic techniques can help relieve the swelling many pregnant people experience.
What’s the difference between deep tissue massage and myofascial release?
Deep tissue targets the muscle fibers with focused, deeper strokes, whereas myofascial release works on the surrounding connective tissue using slower, sustained pressure. Both can improve fluid movement, but myofascial release is gentler on fragile lymphatics.
Can I combine compression stockings with massage?
Absolutely. Wearing graduated compression after a session helps lock in the fluid‑moving benefits, especially for people with venous insufficiency.
Putting It All Together
Massage therapy offers a practical, low‑cost way to fight edema and keep blood flowing smoothly. By choosing the right technique, working with a qualified massage therapist, and adding a few daily self‑care moves, you can shrink swelling, reduce discomfort, and boost overall mobility. Always check with your doctor if you have serious health conditions, and treat massage as part of a broader lifestyle plan that includes movement, diet, and proper hydration.
 Lower GI Bleeding: Diverticula, Angiodysplasia, and How to Diagnose It
Lower GI Bleeding: Diverticula, Angiodysplasia, and How to Diagnose It
 Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
 Hyaluronic Acid Injections for Knee Osteoarthritis: What Really Works
Hyaluronic Acid Injections for Knee Osteoarthritis: What Really Works
 Buy Cheap Generic Tylenol Online - 2025 Guide
Buy Cheap Generic Tylenol Online - 2025 Guide
 Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Richard Wieland
October 12, 2025 AT 06:18Massage can truly ease that ankle puff.
rachel mamuad
October 13, 2025 AT 08:33Yo, the lymphatic drainage is like the circulatory system's best buddy, u know? It's low‑press, rhythmic, and it helps move interstitial fluid out‑the‑door fast, especially post‑op. TL;DR: keep it light and consistent.
Maricia Harris
October 14, 2025 AT 10:48OMG, did anyone actually try the deep‑tissue on their swollen calves? It felt like fireworks on my shins – drama city!
Tara Timlin
October 15, 2025 AT 13:03Really solid info here! If you're dealing with post‑surgical edema, start with gentle lymphatic strokes for 5‑10 minutes twice a day. Pair that with leg elevation for 15 minutes after each session and you’ll notice a measurable reduction in circumference within a week. Don’t forget to stay hydrated and keep sodium low.
benjamin malizu
October 16, 2025 AT 15:18While the article glorifies massage, it neglects the ethical responsibility of ensuring patients understand the risks. Promoting self‑massage for heart‑failure patients without a physician’s clearance borders on negligence, and the jargon‑laden prose obscures this vital warning.
Maureen Hoffmann
October 17, 2025 AT 17:33Hey team, great job breaking down the techniques! Remember, consistency is key – a daily 5‑minute pump routine combined with a short foam‑roller session can dramatically improve lymphatic return. Keep the tone upbeat and encourage readers to celebrate even small drops in swelling!
Alexi Welsch
October 18, 2025 AT 19:48One must inquire whether the presented data truly substantiates the proclaimed efficacy of deep‑tissue massage in venous insufficiency. The citation to the Australian College of Sports Physicians, while credible, lacks a comprehensive meta‑analysis, thereby rendering the conclusion somewhat premature.
Ryan Hlavaty
October 19, 2025 AT 22:03It is morally indefensible to endorse any swelling‑reduction technique without first emphasizing the primacy of medical supervision, especially for those with cardiac comorbidities. The public must be reminded that unqualified hands can cause more harm than good.
Chris Faber
October 21, 2025 AT 00:18Dude, just try the simple ankle circles and a quick leg raise – works like a charm and doesn't cost a dime.
aura green
October 22, 2025 AT 02:33Alright, let’s unpack this whole "massage cures edema" saga, because apparently we’ve all been waiting for a miracle‑rub to replace actual medical care. First, the notion that a gentle hand‑over‑the‑skin can magically siphon off fluid is as whimsical as believing a fairy will sprinkle salt on your fries. Second, the article correctly notes that lymphatic drainage uses very light, rhythmic strokes, but then it glosses over the fact that the lymphatic system is a one‑way highway; you can’t just push fluid uphill without proper valves functioning. Third, the citation from the Australian College of Sports Physicians is real, yet the sample size was modest – a 30‑minute session lowered ankle circumference by merely 1.2 cm, which, while statistically significant, is clinically modest. Fourth, the piece wisely warns about heart conditions, infection, and rapid swelling, but it could have stressed that self‑massage in these scenarios is outright dangerous, not just "consult a professional" as a vague afterthought. Fifth, the DIY tips – pumping strokes, foam‑roller calf work, ankle circles, leg elevation – are solid, but they need context: they supplement, not replace, compression therapy or diuretics when indicated. Sixth, the mention of compression stockings after sessions is spot‑on; compression provides the necessary gradient to keep fluid moving once the lymphatic pump has been kick‑started. Seventh, I love the inclusion of prenatal safety notes, yet many pregnant readers might overlook the advice to avoid deep pressure on the abdomen and lower back, which could be catastrophic. Eighth, the article’s language oscillates between clinical and casual, which can confuse lay readers trying to gauge seriousness. Ninth, the humor about “fluid‑moving benefits” feels forced and detracts from the gravitas of dealing with chronic edema. Tenth, any suggestion that massage is low‑cost is relative; professional lymphatic therapists can be pricey, and insurance often won’t cover them. Eleventh, the piece could have mentioned that regular low‑intensity aerobic activity, like walking, synergizes with massage to improve venous return. Twelfth, hydration and a low‑sodium diet, while listed, deserve stronger emphasis; they are foundational. Thirteenth, the article omits discussion of adjunctive modalities like intermittent pneumatic compression, which can be a game‑changer for severe cases. Fourteenth, the safety disclaimer, while present, should be front‑and‑center, perhaps in a bold banner. Fifteenth, overall, the article does a decent job of summarizing techniques but needs sharper focus on contraindications, realistic outcome expectations, and integration with broader treatment plans. 😊
Sriram K
October 23, 2025 AT 04:48I think the balanced approach here is key – massage can be a useful adjunct, but only when paired with proper medical oversight. For patients with mild edema, the gentle pumping strokes described are safe and inexpensive. However, for anyone with cardiac or renal issues, a physician’s sign‑off is non‑negotiable. Integrating compression stockings and low‑salt diets will amplify any gains from manual therapy. Overall, the article does a good job of highlighting both benefits and red flags.
Deborah Summerfelt
October 24, 2025 AT 07:03Isn’t it fascinating how we treat the body like a leaky faucet? Massage is just a temporary patch; the real solution lies in questioning why the system is clogged in the first place.
Maud Pauwels
October 25, 2025 AT 09:18Clear info good but watch commas and periods next time
Scott Richardson
October 26, 2025 AT 10:33Our country has the best therapists, everyone should try them.
Laurie Princiotto
October 27, 2025 AT 12:48Wow, really? 🙄 This sounds like a sales pitch.
Justin Atkins
October 28, 2025 AT 15:03While the prose exudes enthusiasm, a more nuanced discussion of the physiological mechanisms-namely the Starling forces governing fluid exchange, the role of interstitial oncotic pressure, and the active contractility of lymphangions-would enrich the narrative. Incorporating such details would not only satisfy the intellectually curious but also ground the practical advice in solid biophysical theory.