Pharmacy Management: How Pharmacies Operate, Substitute Drugs, and Serve Patients
When you walk into a pharmacy, you’re not just getting pills—you’re interacting with a system built on pharmacy management, the organized process of dispensing medications, ensuring safety, and complying with legal rules. Also known as pharmaceutical operations, it’s what keeps your prescriptions accurate, affordable, and available when you need them. This isn’t just about counting tablets. It’s about knowing when a pharmacist can swap your brand-name drug for a generic, how regulators in the EU or U.S. control those swaps, and why your pill might look different even though it does the same thing.
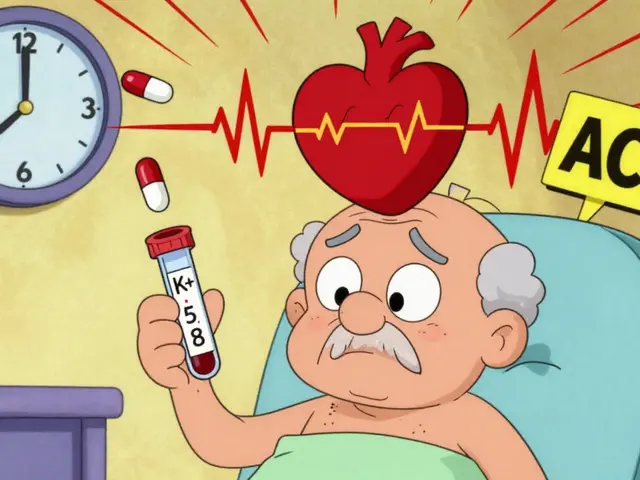
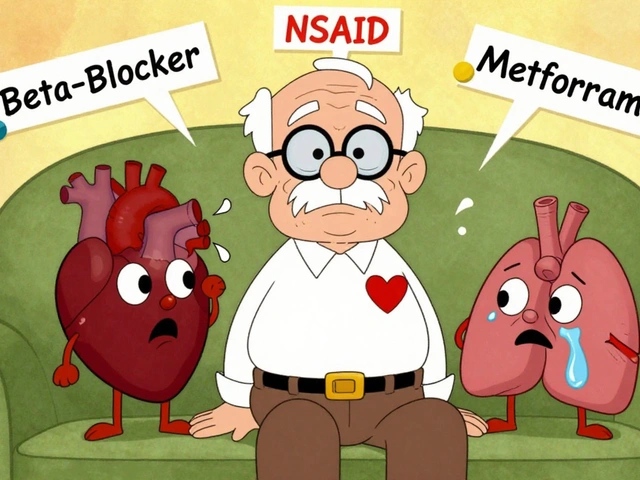
At the heart of pharmacy management is pharmacist substitution authority, the legal power pharmacists have to switch medications under state or national rules. In the U.S., this means a pharmacist can often replace your brand-name drug with a generic version unless your doctor says no. But it’s not always that simple. Some drugs, like those with a narrow therapeutic index, need extra care because even small changes in formulation can affect how they work. In the EU, drug regulation, the set of rules that govern how medicines are approved and sold across countries. Also known as pharmaceutical regulation, it’s shaped by agencies like the EMA, which enforce strict bioequivalence standards before generics hit the shelves. These rules exist because patients need to trust that a $10 generic pill works just like the $100 brand-name version—and sometimes, it does. Other times, differences in fillers, coatings, or release mechanisms cause side effects or reduced effectiveness, especially with extended-release tablets or capsules.
Pharmacy management also ties into how patients access meds today. With apps like Amazon RxPass and Hims & Hers, you can now get generic drugs delivered in 24 hours—no trip to the pharmacy needed. But that shift changes the role of the pharmacist. Instead of just filling scripts, they’re now part of telehealth systems, verifying doses, checking interactions, and guiding patients through substitutions. Meanwhile, regulators are updating rules in 2025 to speed up generic approvals, especially in Europe, where four different pathways exist for bringing cheaper drugs to market. All of this matters because pharmacy management isn’t a back-office function—it’s a frontline health service that affects your safety, your wallet, and your daily routine.
What you’ll find below is a collection of real-world insights into how these systems actually work. From how pharmacists decide which drugs to swap, to why some generics cause more side effects than others, to how international rules differ—you’ll see the hidden mechanics behind every prescription you fill.