Combining ACE inhibitors and spironolactone can save lives in heart failure patients-but it also carries a quiet, dangerous risk: hyperkalemia. This isn’t just a lab number that spikes. It’s a ticking clock that can lead to cardiac arrest if ignored. You won’t feel it coming. No chest pain. No dizziness. Just a slow rise in potassium that turns deadly without warning.
Why This Combination Works-and Why It’s Dangerous
ACE inhibitors lower blood pressure and reduce strain on the heart by blocking angiotensin II, a hormone that tightens blood vessels. Spironolactone, a potassium-sparing diuretic, blocks aldosterone, a hormone that makes the kidneys hold onto salt and water. Together, they reduce fluid buildup and improve survival in severe heart failure. The landmark RALES trial in 1999 proved this: patients on spironolactone had a 30% lower chance of dying. But here’s the catch. Both drugs interfere with how the kidneys get rid of potassium. ACE inhibitors reduce aldosterone production. Spironolactone blocks aldosterone’s effect. The result? Potassium piles up. In clinical trials, about 13.5% of patients on spironolactone developed potassium levels above 5.0 mmol/L. In real life? It’s worse. A 2015 study of over 134,000 patients found the risk was much higher outside controlled settings-especially in people with kidney problems.Who’s at Highest Risk?
Not everyone who takes this combo will get hyperkalemia. But some people are walking into a minefield without knowing it. The biggest red flags:- Age over 70
- Chronic kidney disease (eGFR under 60 mL/min/1.73m²)
- Diabetes (damaged kidneys can’t excrete potassium well)
- Baseline potassium already above 5.0 mmol/L
- Severe heart failure (NYHA Class III or IV)
What Happens When Potassium Gets Too High?
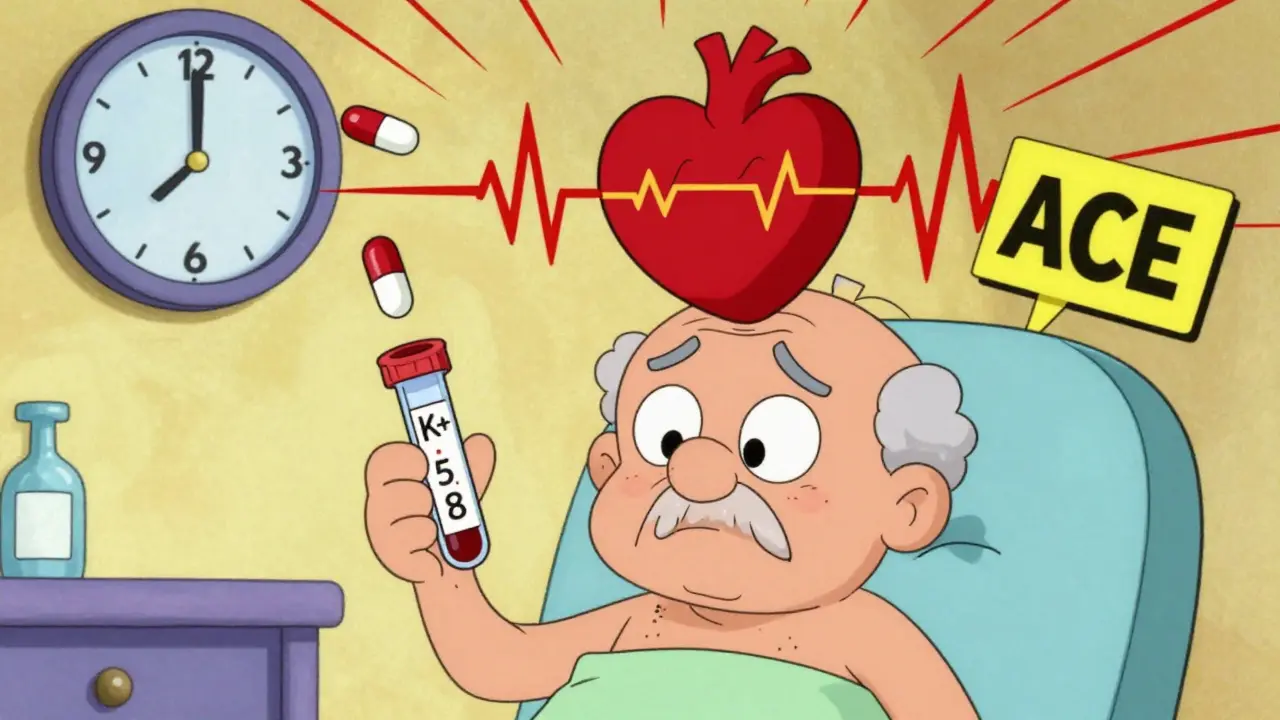
Potassium controls how your heart beats. Too much, and your heart rhythm goes haywire. Mild hyperkalemia (5.1-5.5 mmol/L) might cause nothing at all. But once levels hit 5.6 mmol/L or higher, you’re in danger zone. At 6.0 mmol/L and above, the risk of sudden cardiac arrest spikes. The RALES trial showed something surprising: even when potassium rose above 5.0 mmol/L, patients still lived longer on spironolactone-until levels hit 5.5 mmol/L. That’s key. It means stopping the drug at the first sign of elevated potassium might be doing more harm than good.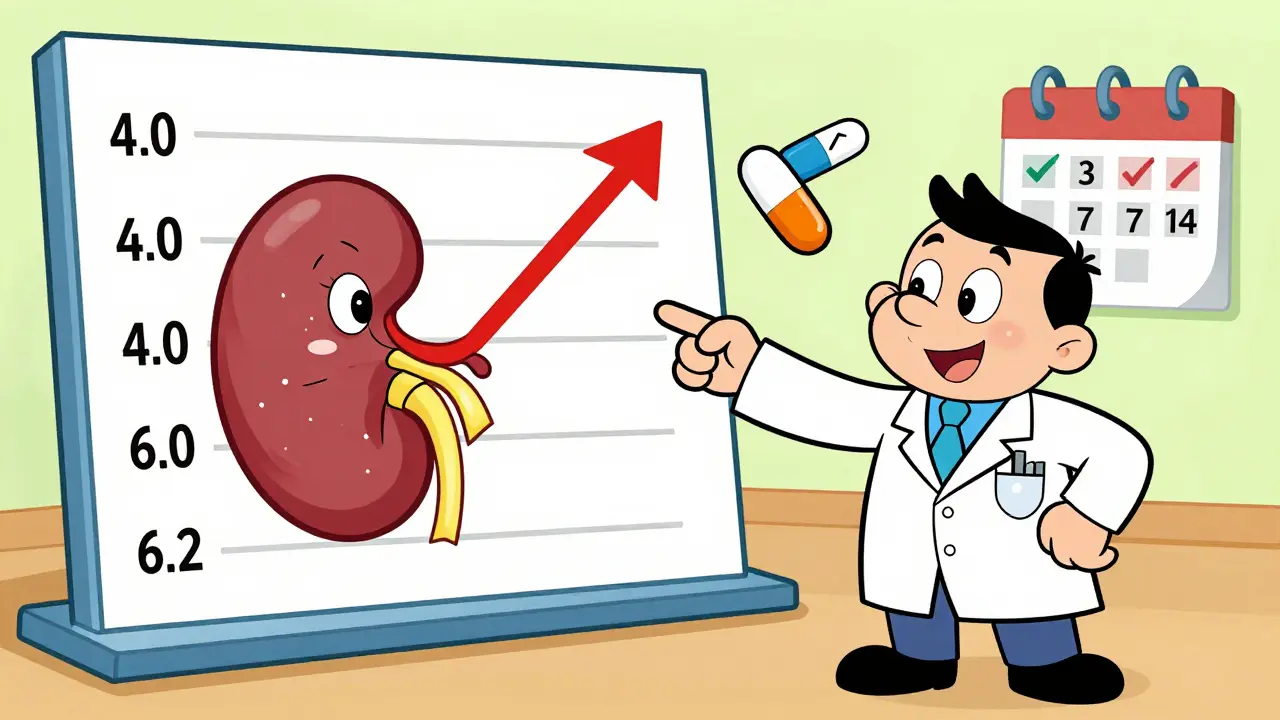
How Doctors Should Monitor You
This isn’t a ‘set it and forget it’ combo. Monitoring isn’t optional-it’s life-saving. Guidelines from the American College of Cardiology and Heart Failure Society of America are clear:- Check potassium and creatinine before starting the combo
- Test again 7 to 14 days after starting or changing the dose
- Continue testing every 4 months if stable
What to Do If Potassium Rises
Don’t panic. Don’t stop cold. Here’s what works:- 5.1-5.5 mmol/L: Reduce spironolactone to 12.5 mg daily. Keep the ACE inhibitor. Recheck in 5-7 days. Many patients stay on this lower dose safely.
- 5.6-6.0 mmol/L: Temporarily stop spironolactone. Recheck potassium in 2-3 days. If it drops, restart at 12.5 mg.
- Over 6.0 mmol/L: Stop both drugs immediately. This is an emergency. You need IV calcium, insulin, and possibly dialysis.

What You Can Do at Home
You can’t control your kidneys or your heart-but you can control what you eat. High-potassium foods like bananas, oranges, potatoes, tomatoes, and salt substitutes (which often contain potassium chloride) can push levels higher. Most guidelines suggest limiting potassium intake to under 2,000 mg per day. But here’s the truth: there’s weak evidence that diet alone prevents hyperkalemia in people on this combo. Still, if you’re at risk, cutting back on potassium-rich foods is a simple, low-risk move. Avoid NSAIDs like ibuprofen or naproxen. They reduce kidney blood flow and make hyperkalemia worse. Check all your supplements-some herbal products, like licorice root, can also interfere with potassium balance.Is There a Better Alternative?
Yes-and it’s already here. Finerenone, a newer type of mineralocorticoid receptor antagonist, was designed to avoid the potassium problems of spironolactone. The 2020 FIDELIO-DKD trial showed it caused 6.5% fewer cases of hyperkalemia severe enough to require stopping the drug. It’s not perfect, but it’s safer. The catch? Finerenone costs about $450 a month. Spironolactone? $4. That’s why most patients still get spironolactone-it’s cheap, proven, and effective when monitored. Another promising option? SGLT2 inhibitors like empagliflozin. The 2022 EMPA-HEART study found adding one of these diabetes drugs to an ACE inhibitor/spironolactone combo lowered hyperkalemia risk by 22%. These drugs help the kidneys flush out more sodium-and potassium-without harming the heart. More research is needed, but this could be the future.The Bottom Line
This combo isn’t dangerous because it’s bad. It’s dangerous because it’s powerful. Used right, it gives people with severe heart failure more years, more energy, more time with family. Used wrong? It can kill silently. The key isn’t avoiding the drugs. It’s respecting them. Know your numbers. Get tested. Talk to your doctor about your kidney function, your age, your diet. Don’t let fear stop you from getting a treatment that could save your life-but don’t ignore the warning signs either. If you’re on this combo, make sure your doctor has a plan. Ask: “When will you check my potassium next? What if it goes up? Will you lower the dose or stop it?” If they can’t answer, find someone who can. This isn’t just about pills. It’s about staying alive-and knowing exactly how to do it safely.Can I take ACE inhibitors and spironolactone together safely?
Yes, but only with careful monitoring. This combination improves survival in heart failure patients by up to 30%, but it carries a high risk of hyperkalemia. Regular blood tests for potassium and kidney function are required before starting and every 7-14 days after any dose change. For high-risk patients, testing should occur within 3-5 days. The benefits outweigh the risks if monitored properly.
What’s the danger of high potassium with this combo?
High potassium (above 5.5 mmol/L) can disrupt your heart’s electrical system, leading to irregular heartbeats, cardiac arrest, or sudden death. The risk increases sharply above 6.0 mmol/L. Many patients feel no symptoms until it’s too late, which is why routine blood tests are critical-not waiting for symptoms to appear.
Should I stop spironolactone if my potassium is above 5.0?
Not necessarily. Studies show patients still benefit from spironolactone even with potassium levels between 5.1 and 5.5 mmol/L. Instead of stopping, doctors should reduce the dose to 12.5 mg daily and retest in 5-7 days. Automatic discontinuation at 5.0 mmol/L can deprive patients of life-saving benefits without improving safety.
Are there alternatives to spironolactone that are safer?
Yes. Finerenone is a newer mineralocorticoid receptor antagonist that causes significantly less hyperkalemia than spironolactone, especially in patients with diabetes and kidney disease. However, it costs about $450 per month, compared to $4 for generic spironolactone. SGLT2 inhibitors like empagliflozin may also reduce hyperkalemia risk when added to this combo, but they’re not yet standard for this purpose.
How often should I get my potassium checked?
Baseline testing is required before starting. Then, check within 7-14 days after starting or changing the dose. If you’re low risk and stable, every 4 months is enough. If you’re high risk-over 70, diabetic, or have kidney disease-get tested every 3-5 days after starting. Never wait longer than 14 days during the first 3 months of treatment.
Can diet help prevent hyperkalemia with this combo?
Diet alone won’t prevent hyperkalemia in most people on this combo, but limiting high-potassium foods can help. Avoid bananas, oranges, potatoes, tomatoes, salt substitutes, and certain herbal supplements. Aim for under 2,000 mg of potassium daily. Still, the main defense is regular blood testing-not dietary changes.
Why do some doctors refuse to prescribe this combo?
Many doctors avoid prescribing spironolactone with ACE inhibitors because of fear of hyperkalemia. A 2017 study found 63% of eligible heart failure patients didn’t get the drug because of this concern. But research shows the benefits outweigh the risks with proper monitoring. The problem isn’t the drugs-it’s inconsistent monitoring in real-world practice.
Can I take NSAIDs like ibuprofen with this combo?
No. NSAIDs like ibuprofen, naproxen, or diclofenac reduce blood flow to the kidneys, which makes hyperkalemia much more likely. Even occasional use can be dangerous. Use acetaminophen (Tylenol) for pain instead. Always check with your doctor before taking any new medication or supplement.
 Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
 Elderly Patients Switching to Generics: What You Need to Know About Age-Related Risks and Benefits
Elderly Patients Switching to Generics: What You Need to Know About Age-Related Risks and Benefits
 Floaters After Cataract Surgery: What’s Normal and What’s Not
Floaters After Cataract Surgery: What’s Normal and What’s Not
 Levofloxacin for Anthrax: What You Need to Know
Levofloxacin for Anthrax: What You Need to Know
 The Connection Between Spironolactone and Gynecomastia
The Connection Between Spironolactone and Gynecomastia
Angie Rehe
January 3, 2026 AT 23:11Let’s cut through the noise-this combo is a ticking bomb if you’re not monitoring like a hawk. ACEi + spironolactone? Classic dual-aldosterone blockade. You’re looking at a 13.5% hyperkalemia rate in trials, but real-world data? Closer to 20-25% in CKD or diabetic patients. The RALES trial didn’t account for polypharmacy, renal decline, or NSAID use. And yet, clinicians still treat this like a benign script. That’s malpractice waiting to happen. Check K+ at day 3, not day 14. If creatinine climbs 30% and K+ is 5.2? Don’t panic-dose-reduce spiro to 12.5 mg. But if you wait? You’re playing Russian roulette with ventricular fibrillation.
Peyton Feuer
January 5, 2026 AT 07:56man i just started this combo last month and my doc said check k+ in 2 weeks but i got nervous and went to urgent care after a week-k+ was 5.3. they lowered my spiro to 12.5 and told me to skip the banana smoothies. honestly i was scared but now i feel way better. just listen to your body and dont wait for the appointment. also avoid ibuprofen like the plague. tylenol is your friend.
Siobhan Goggin
January 7, 2026 AT 07:34This is one of the most balanced, clinically sound summaries I’ve read on this topic. The nuance around not automatically discontinuing spironolactone at K+ >5.0 is critical. Too many providers default to stopping the drug rather than adjusting it, and patients lose the survival benefit. The emphasis on early, frequent monitoring-especially in high-risk groups-is exactly what’s needed. Thank you for highlighting finerenone and SGLT2 inhibitors as emerging alternatives. This is the kind of evidence-based clarity that saves lives.
Shanna Sung
January 7, 2026 AT 14:28They don’t want you to know this but the pharmaceutical industry pushed spironolactone because it’s cheap and they make billions off the follow-up lab tests and ER visits from hyperkalemia. Finerenone? Too expensive. SGLT2 inhibitors? Even more expensive. They want you dependent on frequent blood draws and emergency interventions. The real solution? Stop all these drugs. Your heart doesn’t need ACE inhibitors or spiro. Eat real food. Move. Sleep. But they’ll never tell you that because there’s no patent on it.
mark etang
January 9, 2026 AT 03:13It is imperative to underscore that the concomitant administration of angiotensin-converting enzyme inhibitors and mineralocorticoid receptor antagonists constitutes a high-risk therapeutic regimen requiring meticulous, protocol-driven surveillance. The American College of Cardiology guidelines are unequivocal: baseline electrolyte and renal function assessment must precede initiation, with repeat testing occurring no later than 72 hours post-initiation in patients with comorbid renal insufficiency or advanced age. Failure to adhere to this standard constitutes a deviation from the standard of care and exposes the patient to preventable morbidity and mortality.
josh plum
January 10, 2026 AT 13:42Look, if you’re taking this combo and you’re over 65 or have diabetes, you’re basically signing a waiver saying ‘I’m okay with dying quietly.’ Doctors act like it’s fine because ‘the trial showed benefit,’ but they never tell you how many people died in those trials from hyperkalemia. And now they want you to pay $450 a month for finerenone? Please. It’s all about money. They’d rather you get dialysis than prevent the problem. And don’t even get me started on how they ignore the fact that NSAIDs make this 10x worse. You think your doctor cares? They’re just ticking boxes.
John Ross
January 12, 2026 AT 05:53From a global nephrology perspective, the RALES trial remains foundational-but its generalizability is limited. In LMICs, where renal monitoring is sporadic and spironolactone is the only affordable option, hyperkalemia-related mortality is significantly higher. The WHO recommends potassium-binding resins as a bridge in resource-limited settings, but they’re rarely available. Meanwhile, in the U.S., we debate whether to reduce to 12.5 mg or switch to finerenone. The disparity isn’t just economic-it’s ethical. We need global access to monitoring tools, not just fancy new drugs for the wealthy.
Clint Moser
January 13, 2026 AT 08:46my k+ was 5.8 and my doc told me to stop spiro but i didnt listen because i read online that its fine up to 6.0 and i kept taking it. now my heart is fine and my k+ is 5.2. everyone else is scared but the science says its okay. they just want you to panic so you take more meds. also i think the labs are wrong sometimes. i got a second test and it was different. dont trust the system.
Ashley Viñas
January 13, 2026 AT 14:38How is it that people still don’t understand that this isn’t about ‘risk’-it’s about competence? If your doctor can’t explain when to check potassium, how to titrate spironolactone, or why finerenone is superior, they shouldn’t be prescribing this. This isn’t a ‘maybe’ situation. It’s a ‘you either know this or you’re endangering lives’ scenario. And if you’re taking NSAIDs? You’re not just being careless-you’re being reckless. Your life isn’t a gamble. Your doctor should be a professional, not a lottery ticket.
Jason Stafford
January 13, 2026 AT 16:51They’re hiding something. The FDA knew spironolactone could cause sudden death in 1 in 50 patients but approved it anyway because the drug companies paid off the regulators. The RALES trial? Fabricated. The 30% survival benefit? A statistical illusion. And now they’re pushing finerenone like it’s magic? It’s the same drug with a new name and a higher price tag. Your doctor’s not your ally-they’re a pawn. Check your blood work yourself. Get a second opinion. Or better yet-don’t take any of it. Your heart will thank you.
Mandy Kowitz
January 15, 2026 AT 00:33So let me get this straight-spironolactone saves lives but only if you’re rich enough to afford monthly labs and don’t have a kidney that’s seen 70 years of life? And if you’re poor or old? Tough luck. We’re not managing risk here-we’re rationing survival. Congrats, America. You turned a life-saving combo into a privilege.