Levothyroxine Safety: What You Need to Know About Dosage, Interactions, and Side Effects
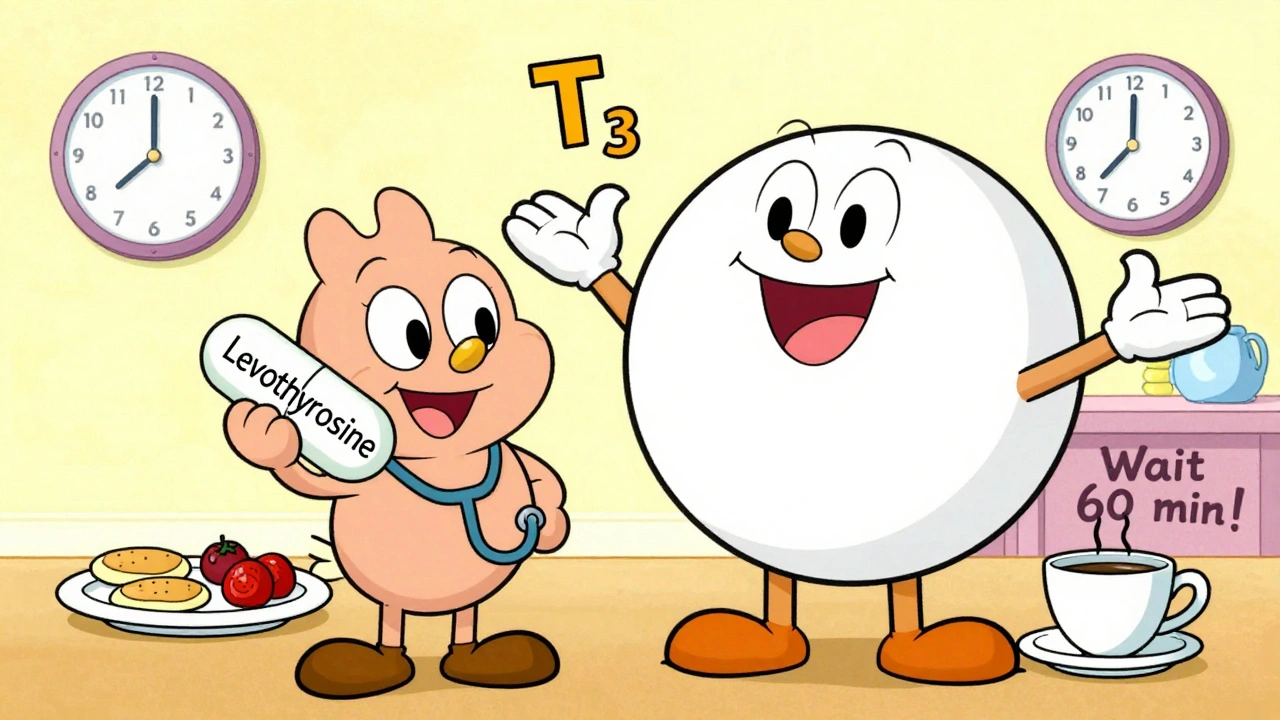
When you're taking levothyroxine, a synthetic form of the thyroid hormone T4 used to treat hypothyroidism. Also known as thyroid hormone replacement, it's one of the most commonly prescribed medications in the U.S.—but that doesn't mean it's simple to get right. Millions take it daily, yet many don’t realize how easily food, other drugs, or even timing can mess with its absorption. A pill taken with coffee or calcium can become nearly useless. A dose too high can cause heart palpitations, bone loss, or anxiety. Too low, and you’re still tired, gaining weight, and feeling foggy. Levothyroxine safety isn’t about just filling the prescription—it’s about understanding how your body actually uses it.
Drug interactions, how other medications interfere with levothyroxine’s effectiveness are one of the biggest hidden risks. Iron supplements, antacids, proton pump inhibitors, and even soy products can block absorption if taken at the same time. Even some heart meds like cholestyramine or sevelamer can do the same. And don’t forget about thyroid hormone replacement, the broader category levothyroxine belongs to—switching brands or generics without checking with your doctor can lead to dose shifts, because not all formulations are absorbed the same way. The FDA says generics are bioequivalent, but real-world reports show some patients feel worse after switching. That’s why consistency matters: stick to the same brand or generic if it’s working.
Levothyroxine side effects, the symptoms that signal your dose might be off are often mistaken for other problems. Heart racing? Could be too much. Hair loss or constipation returning? Could be too little. Weight changes, insomnia, or muscle weakness aren’t just random—they’re clues. Your doctor should check your TSH levels every 6–8 weeks after a dose change, then at least once a year once stable. But many people never get retested. If you’re on levothyroxine and haven’t had a blood test in over a year, you’re flying blind.
Levothyroxine isn’t a one-size-fits-all pill. Age, weight, other health conditions like heart disease or kidney problems, and even pregnancy all change what your body needs. Women over 65 often need lower doses. People with adrenal insufficiency can crash if given levothyroxine without steroids first. And if you’re pregnant, your dose will likely need to go up—sometimes by 30% or more. Ignoring those factors isn’t just risky—it’s dangerous.
What you’ll find below are real stories and practical advice from people who’ve been there: how to time your pill correctly, what to do when you miss a dose, how to talk to your pharmacist about substitutions, and which supplements to avoid. No fluff. No guesswork. Just what actually keeps people safe on this medication.