Levothyroxine is one of the most commonly prescribed medications in the world. In the U.S. alone, over 127 million prescriptions were filled in 2022. In the UK, nearly 260 million packs were dispensed between 2016 and 2020. It’s not a miracle drug. It’s not a cure. It’s a replacement. For people with an underactive thyroid, levothyroxine restores the hormone their body no longer makes in enough quantity. But taking it isn’t as simple as popping a pill every morning. Get the dose wrong, switch brands without warning, or skip monitoring, and you could end up feeling worse than before you started.
Why Levothyroxine Works - and Why It Can Go Wrong
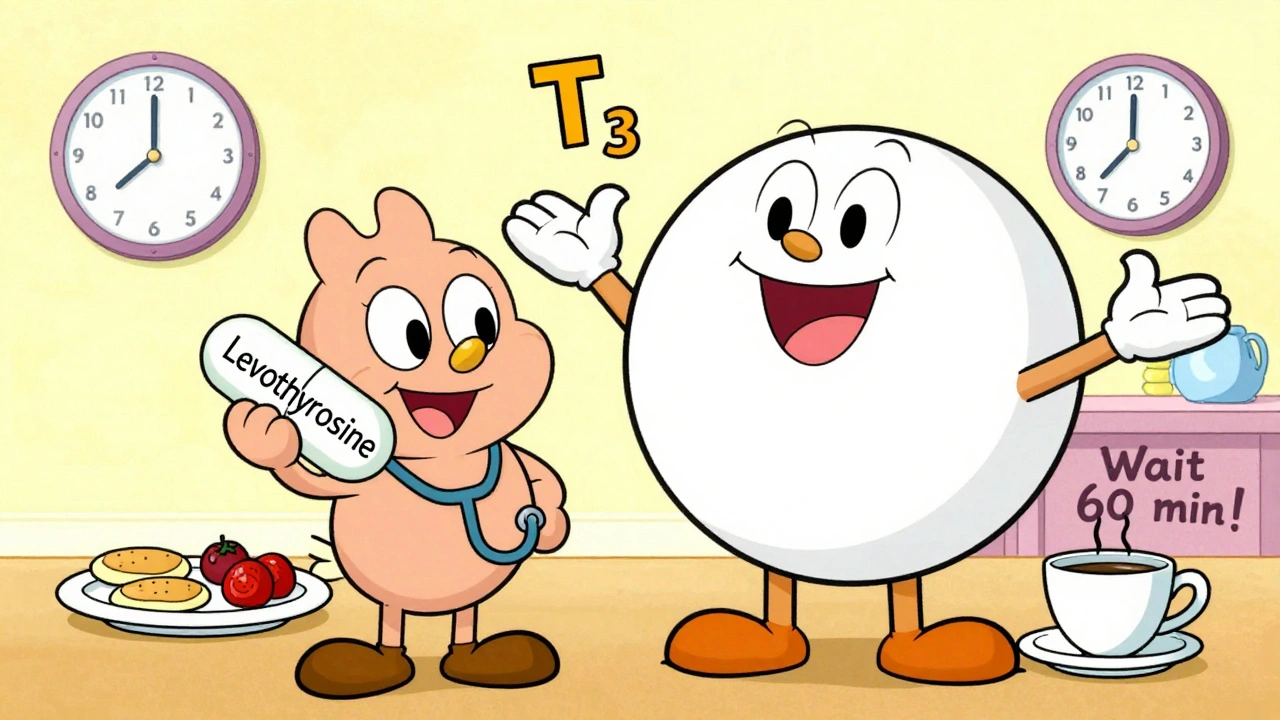
Levothyroxine is a synthetic version of T4, the main hormone your thyroid makes. Your body converts T4 into T3, the active form that powers your metabolism, brain function, heart rate, and body temperature. When your thyroid fails - whether from Hashimoto’s, surgery, radiation, or just aging - levothyroxine steps in. Done right, it fixes fatigue, weight gain, brain fog, and cold intolerance. Most people feel better within 3 to 6 months.
But here’s the catch: thyroid hormones have a narrow therapeutic window. That means the difference between the right dose and a harmful one is small. Too little, and you stay hypothyroid. Too much, and you risk heart palpitations, bone loss, anxiety, and even atrial fibrillation - especially in older adults.
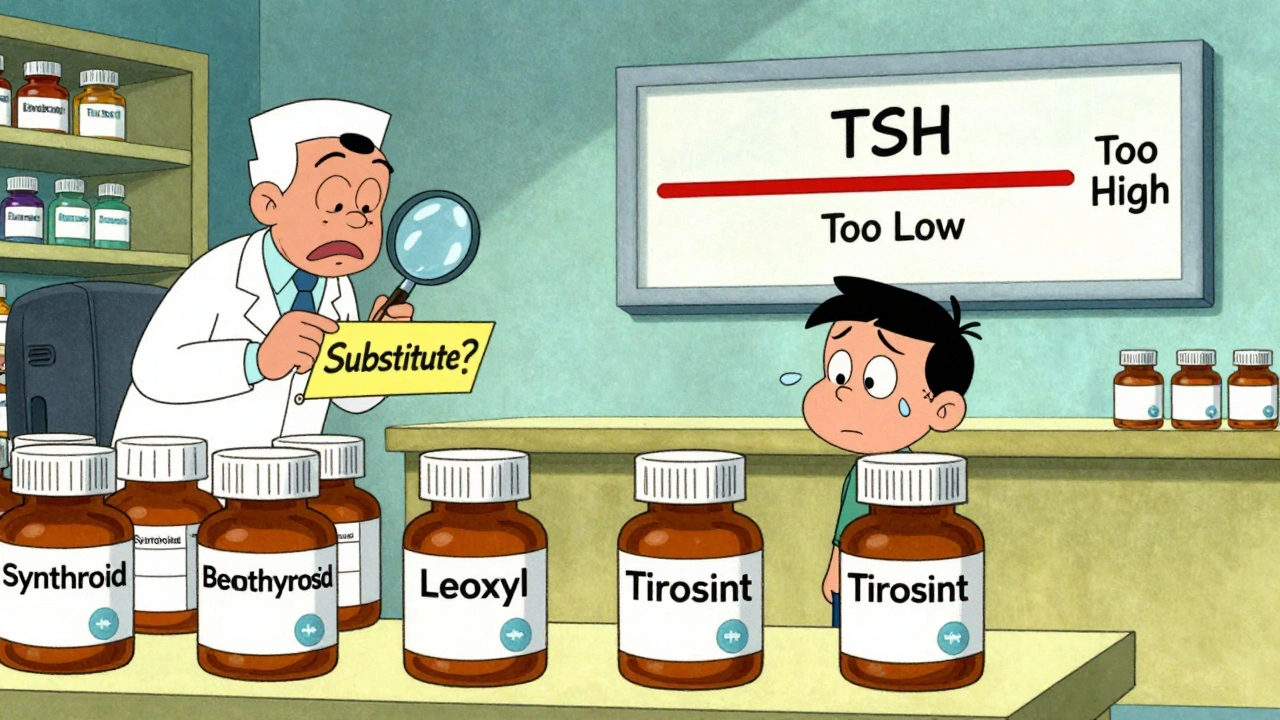
And it’s not just about the dose. The brand matters. A lot. In 2021, the UK’s MHRA reviewed 335 reports of problems after switching levothyroxine brands. Patients reported fatigue, headaches, weight gain, and palpitations - classic signs of thyroid imbalance. Yet only 27 of those cases had thyroid blood tests done. That’s like adjusting your car’s fuel injection without checking the engine light.
How Often Should You Get Tested?
There’s no one-size-fits-all schedule. But there are clear guidelines backed by the American Thyroid Association and the UK’s Specialist Pharmacy Service.
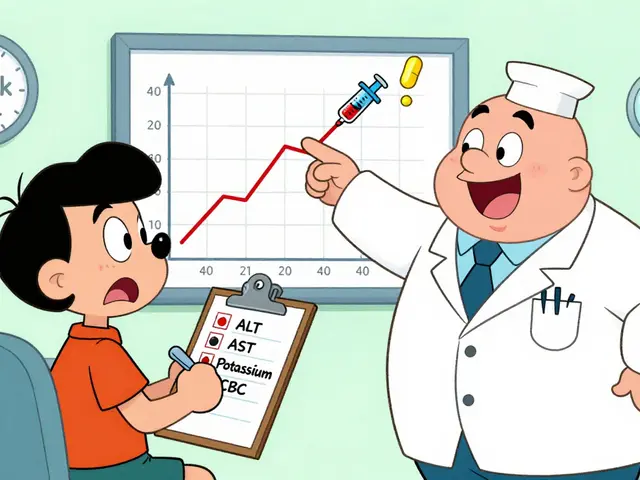
When you start levothyroxine, or after a dose change, your TSH (thyroid-stimulating hormone) should be checked in 6 weeks. That’s not a suggestion - it’s the minimum. TSH is the most sensitive marker of thyroid hormone levels in your blood. Free T4 is also useful if symptoms persist.
Once your levels are stable - meaning two TSH tests 3 months apart are both in range - you can drop to testing every 6 to 12 months. But if you’re over 65, have heart disease, are pregnant, or take drugs like amiodarone or lithium, you need more frequent checks. Some patients need testing every 3 months, even when stable.
Here’s the problem: NHS data from 2022 showed only 58% of primary care practices follow these guidelines. Over a third of patients go more than 18 months without a TSH test. That’s dangerous. Your needs change. Weight gain? Medication changes? Aging? All of these affect how much levothyroxine you need. Skipping tests means you’re flying blind.
When to Worry About Side Effects
Levothyroxine itself isn’t toxic. But getting the dose wrong can be. Symptoms of under-treatment (too little) include:
- Constant tiredness
- Weight gain despite eating less
- Depression or brain fog
- Dry skin and hair loss
- Feeling cold when others are fine
Symptoms of over-treatment (too much) include:
- Heart palpitations or racing heartbeat
- Anxiety, irritability, or insomnia
- Unexplained weight loss
- Sweating more than usual
- Shaky hands or muscle weakness
These aren’t just "feeling off" moments. They’re signals your body is out of balance. If you’re on levothyroxine and notice any of these, don’t wait for your next appointment. Call your doctor. Get tested.
And here’s something few people know: if you’ve switched brands and suddenly feel worse - even if the label says the same dose - it’s not in your head. A 2022 survey of 1,245 members of Thyroid UK found 68% had adverse reactions after switching manufacturers. The FDA and EMA require all brands to be bioequivalent, but absorption can still vary slightly between fillings. For some people, that’s enough to trigger symptoms.
How to Take Levothyroxine Correctly
It’s not just about the dose. It’s about how you take it.
Levothyroxine must be taken on an empty stomach. Wait 30 to 60 minutes before eating. Take it at the same time every day - ideally in the morning, before breakfast. If you can’t do that, take it at bedtime, but only if you haven’t eaten for at least 3 hours.
Now, here’s the kicker: many common supplements and medications interfere with absorption. If you take calcium, iron, or antacids - even one a day - they can block levothyroxine from entering your bloodstream. The same goes for cholesterol drugs like cholestyramine and soy products. The solution? Space them out by at least 4 hours.
And don’t take it with coffee. Studies show caffeine reduces absorption by up to 30%. Wait an hour after your pill before your morning brew.
Who Needs Special Care?
Not everyone on levothyroxine is the same. Some groups need extra attention:
- Pregnant women: Thyroid needs jump by 30-50% during pregnancy. TSH should be checked every 4 weeks in the first half, then at least once in the third trimester. Untreated hypothyroidism increases risks of miscarriage, preterm birth, and developmental delays.
- People over 65: Older adults are more sensitive to excess thyroid hormone. Higher TSH targets (up to 7.5 mIU/L) are often safer than forcing levels into the young adult range.
- Those with heart disease: Starting or increasing levothyroxine too fast can trigger angina or arrhythmias. Dose increases should be slow - 12.5 to 25 mcg at a time.
- Patients on lithium or amiodarone: These drugs directly affect thyroid function. Monitoring every 3 months is non-negotiable.
- Children and teens: Growth and development depend on stable thyroid levels. Regular testing and endocrinology follow-up are essential.
If you fall into any of these groups, ask your doctor if you should be referred to an endocrinologist. Primary care doctors are great, but thyroid management gets complex fast.

The Bigger Picture: Why Monitoring Is Broken
Levothyroxine is cheap. It’s generic. It’s been around for 70 years. That’s why so many systems treat it like a simple fix. But it’s not. It’s a precision tool.
The reality? Most patients are left to manage this on their own. They get a prescription, a leaflet, and a vague "come back in a year." They don’t know how to track symptoms. They don’t know to ask for tests. They don’t know to demand the same brand.
And pharmacists? They’re trained to substitute generics to save money. But with levothyroxine, that can backfire. The MHRA now advises doctors to specify brand names on prescriptions for patients who’ve had bad reactions to switches. That’s a small step - but it’s progress.
What’s missing? A system that treats thyroid patients as chronic care cases, not afterthoughts. Regular blood tests. Clear communication. Consistent brands. Patient education. All of it.
Here’s what you can do: Keep a symptom journal. Note energy levels, mood, weight, and sleep. Bring it to every appointment. Ask for your TSH and Free T4 results - don’t wait for your doctor to offer them. If you switch pharmacies or brands, tell your doctor. If you feel off, get tested - don’t assume it’s "just stress."
Thyroid disease doesn’t discriminate. It affects women more than men. It gets worse with age. It hides in plain sight. But with proper monitoring, it’s manageable. Not perfect. Not easy. But manageable.
What’s Next for Levothyroxine?
Research is moving fast. Mayo Clinic is studying genetic markers that predict how fast someone metabolizes thyroid hormone. Early results suggest 23% of dose differences between people might be genetic. That could mean personalized dosing in the next 5 to 10 years.
Some patients still feel tired even with normal TSH. That’s led to interest in adding T3 (liothyronine) to treatment. But current evidence doesn’t support it for most people. It’s not a magic fix. And it comes with its own risks.
For now, levothyroxine remains the gold standard. But it’s only as good as the care around it. The pill doesn’t fail. The system does.
Don’t let yours.
Can I switch levothyroxine brands without telling my doctor?
No. Even if the dosage is the same, different brands can have slight variations in how your body absorbs the hormone. Many patients report symptoms like fatigue, weight changes, or anxiety after switching. If you notice new or worsening symptoms after a pharmacy substitution, contact your doctor and ask for a thyroid function test. Some doctors now write "dispense as written" on prescriptions to prevent automatic substitutions.
How long does it take for levothyroxine to start working?
You might notice small improvements in energy or mood within 2 to 3 weeks, but full symptom relief usually takes 3 to 6 months. That’s because your body needs time to adjust hormone levels and for tissues to respond. Don’t rush dose changes - wait at least 6 weeks after any adjustment before retesting TSH. Patience is key.
Is it safe to take levothyroxine for life?
Yes, when monitored properly. Levothyroxine is designed for long-term use. Many people take it for decades without issues. The risks come from incorrect dosing, not the medication itself. Regular blood tests and consistent dosing habits are what keep you safe. Stopping without medical advice can lead to a dangerous return of hypothyroid symptoms.
What should I do if I miss a dose?
If you miss a dose in the morning, take it as soon as you remember - as long as it’s still on an empty stomach. If it’s already time for your next dose, skip the missed one. Don’t double up. Occasional missed doses won’t harm you, but consistency matters. Set a phone alarm or use a pill organizer to stay on track.
Why do some people still feel tired even with normal TSH levels?
It’s not uncommon. TSH reflects what your pituitary gland sees, but not necessarily how your tissues are using the hormone. Some people have trouble converting T4 to T3, or have cellular resistance. Others have coexisting conditions like vitamin D deficiency, iron deficiency, or adrenal fatigue. If you’re still symptomatic, ask your doctor to check Free T3, ferritin, vitamin D, and cortisol. Sometimes, the answer isn’t just a higher dose.
Final Thoughts: Your Thyroid, Your Responsibility
Levothyroxine isn’t a quick fix. It’s a lifelong partnership between you and your body. You can’t outsource your care. You need to know your numbers. You need to track your symptoms. You need to speak up when something feels off.
Most people on levothyroxine do fine. But the ones who struggle? They’re usually the ones who didn’t ask the right questions. Who didn’t get tested often enough. Who switched brands without thinking. Who trusted the system - instead of their own body.
Don’t be one of them. Know your TSH. Know your brand. Know your symptoms. And never, ever assume it’s "just aging." Your thyroid is working for you. Make sure you’re working for it too.
 Where and How to Buy Calan Online Safely: Everything You Need to Know
Where and How to Buy Calan Online Safely: Everything You Need to Know
 How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
 Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
 Formulation Differences and Side Effects: Tablets, Capsules, and Extended-Release Medications
Formulation Differences and Side Effects: Tablets, Capsules, and Extended-Release Medications
Jennifer Blandford
December 10, 2025 AT 05:10Okay but can we talk about how wild it is that we treat thyroid meds like aspirin? I switched brands last year and went from feeling like a superhero to a zombie in two weeks. My doctor laughed when I brought it up. Like, nope, same number on the pill, you're fine. I had to demand bloodwork. Turns out my TSH was through the roof. Now I only take the one brand and I’m alive again. Seriously, if you feel off after a switch - don’t brush it off. Your body isn’t lying.
Ronald Ezamaru
December 10, 2025 AT 22:14There's a reason the American Thyroid Association recommends TSH checks every 6 weeks after a dose change. It's not arbitrary. TSH is the most sensitive indicator we have. Many primary care providers skip this because it's inconvenient - but that’s not patient care, that’s triage. If you're stable, biannual testing is fine. But if you're pregnant, elderly, or on other meds? Quarterly is the baseline. Don’t let cost-cutting replace clinical judgment.
Ryan Brady
December 11, 2025 AT 04:37Ugh, another hypochondriac post. You people act like levothyroxine is rocket science. It's a pill. Take it. Stop complaining. If you're tired, maybe you're just lazy. Also, why are we letting pharmacists even think about switching brands? We should ban generics for this stuff. America needs to stop being so cheap with health. #BuyAmerican
Raja Herbal
December 11, 2025 AT 09:28So in India, we get levothyroxine from five different manufacturers and no one checks TSH for a year. And yet, somehow, people live. Maybe the problem isn’t the drug - it’s the obsession with numbers. I’ve seen patients on 100mcg who feel fine, and others on 50mcg crying because their TSH is 5.2. Your body knows more than your lab report. Maybe we should stop treating thyroid like a math problem.
Rich Paul
December 12, 2025 AT 18:06bro i took mine with coffee for 3 years and never felt anything. now i read this and i’m like… wait. did i just waste 3 years being tired because i was a dumbass? also i take iron at night and levothyroxine in the am - does that count? or do i need to like… wait 4 hours? this is wild. also why does my doc just give me a script and say ‘see ya’?
Delaine Kiara
December 13, 2025 AT 15:17Let me tell you about my cousin Linda. She was on levothyroxine for 12 years. Switched brands. Got a new pharmacist. Suddenly she couldn’t sleep, lost 20 pounds, and started crying in Target. She went to three doctors. One told her it was menopause. Another said she was ‘overreacting.’ Finally, her endo ordered a full panel - Free T3 was low, ferritin was 8, vitamin D was 12. She was literally falling apart. They upped her dose, added T3, started iron and D3. Now she’s hiking in Colorado. Don’t let your doctor treat you like a number. You’re a whole person. And your thyroid? It’s not just a widget.
Gilbert Lacasandile
December 14, 2025 AT 10:51I’ve been on this med for 15 years. I take it at 5 a.m., no food, no coffee, no supplements. I get tested every 6 months. I know my numbers. I know my brand. I don’t need a lecture. I just need the system to stop being lazy. If you’re going to prescribe this, own it. Don’t hand me a script and disappear. I’m not your afterthought.
Darcie Streeter-Oxland
December 16, 2025 AT 07:30It is, regrettably, a matter of considerable concern that the prevailing clinical paradigm for levothyroxine management remains inadequately aligned with evidence-based guidelines. The substitution of pharmaceutical brands without biochemical verification constitutes a significant deviation from the standard of care, particularly in elderly and cardiovascular-compromised populations. The data cited from the MHRA is both compelling and alarming. It is imperative that prescribers adopt a more rigorous and individualized approach to thyroid hormone replacement therapy.
Mona Schmidt
December 17, 2025 AT 13:21Thank you for writing this. I’ve been managing Hashimoto’s for 18 years and the lack of education around this is staggering. I keep a symptom journal - energy, mood, sleep, weight. I bring it to every appointment. I ask for my labs. I refuse to be passed off as ‘just stressed.’ If you’re on levothyroxine, you deserve to feel like yourself again. And you’re not being dramatic if you do. Your symptoms are real. Your needs matter. Keep asking. Keep tracking. You’re not alone.
Guylaine Lapointe
December 18, 2025 AT 06:00It’s not just the system - it’s the patients. I’ve seen people on levothyroxine for years who refuse to get tested because they’re ‘afraid of the numbers.’ You can’t outsource your health to a doctor. You have to show up. You have to read the damn leaflet. You have to know that coffee blocks absorption. You have to ask for your brand. You have to be the advocate for your own body. If you’re not willing to do that, don’t complain when you feel like garbage.
Sarah Gray
December 18, 2025 AT 16:05It’s tragic how little medical training exists on thyroid function. I’m a nurse practitioner and I’ve had patients come in with TSH levels over 20, asymptomatic, because their PCP ‘didn’t think it was necessary to test.’ Levothyroxine isn’t just a pill - it’s a hormonal lever that affects every system in the body. If you’re not monitoring it like you would insulin or warfarin, you’re not practicing medicine. You’re guessing. And people are suffering because of it.