When you’re pregnant, even the smallest skin irritation can feel like a big problem. Eczema flares up. Acne breaks out. Fungal infections creep in. You want relief-but you’re terrified of harming your baby. The good news? Most topical medications are much safer than you think. Unlike pills or injections, creams and lotions barely make it into your bloodstream. But not all of them are safe. Some can still pose risks, especially if used wrong or in the wrong trimester.
Why Topical Medications Are Usually Safer in Pregnancy
Topical treatments work on the skin’s surface. Only a tiny fraction-usually 1% to 10%-gets absorbed into your blood. That’s why they’re often the first choice for treating rashes, acne, or fungal infections during pregnancy. Compare that to oral antibiotics or retinoids, which flood your system and can cross the placenta easily. A 2016 review in the Journal of Drugs in Dermatology found that most topical dermatologic drugs have minimal fetal risk because of this low absorption rate. But here’s the catch: absorption isn’t the same everywhere. Skin on your face, neck, armpits, and groin absorbs more than skin on your forearm or leg. So applying a strong steroid cream to your eyelids? That’s riskier than using it on your arm. Always apply the smallest amount needed, and avoid covering large areas for long periods.What’s Safe for Acne During Pregnancy
Acne is super common during pregnancy-hormones go wild, oil glands go into overdrive. You might be tempted to reach for your old acne cream, but many popular ones are off-limits. Safe options:- Benzoyl peroxide (5-10%): This is one of the most recommended treatments. It kills bacteria and unclogs pores. Studies show less than 5% gets absorbed, and no birth defects have been linked to its use.
- Topical clindamycin: An antibiotic that works well for inflammatory acne. About 4-5% is absorbed, but serum levels stay too low to cause concern. Often combined with benzoyl peroxide for better results.
- Topical erythromycin: Another antibiotic option with a strong safety record in pregnancy. Used for years without evidence of fetal harm.
- Azelaic acid (15-20%): Great for acne and melasma (the pregnancy mask). Classified as Category B, and many women report clear skin with no side effects.
- Topical retinoids (tretinoin, adapalene, tazarotene): Even though they’re applied to the skin, case reports link them to birth defects when used in early pregnancy. The American College of Obstetricians and Gynecologists (ACOG) says to stop them before trying to conceive.
- Salicylic acid in high doses or large areas: Low concentrations (2% or less) in cleansers or toners are generally fine. But avoid peels, masks, or spot treatments with higher concentrations-especially in the third trimester.
Managing Eczema and Itchy Skin
Itchy, red, flaky skin? You’re not alone. About 20% of pregnant women develop eczema or pregnancy-related rashes like PUPPP. The key is gentle, targeted treatment. Safe choices:- Low-potency hydrocortisone cream (1%): This is the go-to for mild eczema. Used sparingly on small areas, it’s considered safe. Studies show no increased risk of low birth weight or cleft palate.
- Mild to moderate corticosteroids (like desonide): These are fine for short-term use under your doctor’s guidance. Avoid potent versions (like clobetasol) unless absolutely necessary.
- Moisturizers with ceramides: These aren’t drugs, but they’re essential. Keeping skin hydrated reduces flare-ups and the need for steroids.
- High-potency steroids (clobetasol, betamethasone): These can cross the placenta in small amounts. Long-term or widespread use has been linked to lower birth weight in rare cases.
- Calcineurin inhibitors (tacrolimus, pimecrolimus): These are not well studied in pregnancy. Most doctors recommend avoiding them unless you’ve tried everything else.

Fungal Infections: Yeast, Athlete’s Foot, Ringworm
Pregnancy increases your risk of yeast infections-up to 30% of women get one. Vaginal itching, white discharge? You need treatment. But not all antifungals are created equal. Safe first-line options:- Clotrimazole (cream, suppository): First choice for vaginal yeast infections. Used for decades with no evidence of harm.
- Miconazole: Same safety profile. Available as creams for skin and vaginal suppositories.
- Nystatin: Often used for oral thrush or diaper rash. Not absorbed systemically, so it’s very safe.
- Econazole: Avoid in the first trimester. Use only if needed in later months, and only on small areas.
- Terbinafine (Lamisil): Not well studied. Skip it unless your doctor says it’s necessary.
- Ketoconazole: Newer data from 2022 suggests short-term topical use is acceptable, but still avoid oral versions entirely.
What About Pain and Inflammation?
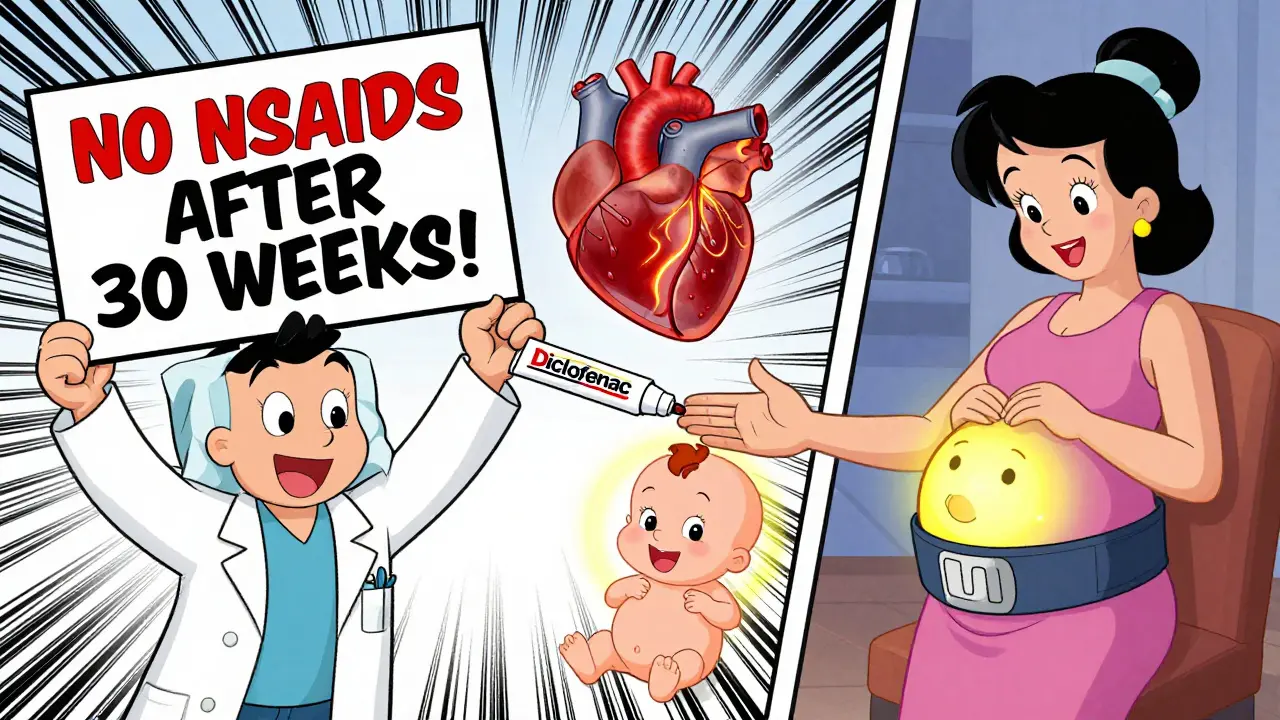
Back pain? Swollen ankles? You might reach for a topical NSAID like diclofenac gel. It sounds harmless-just rub it on. But it’s not risk-free. Safe? Sort of. Topical NSAIDs absorb less than pills, but they still enter your bloodstream. The American Academy of Family Physicians warns: avoid them after 30 weeks. Why? They can cause the ductus arteriosus-a vital blood vessel in the baby’s heart-to close too early. This can lead to serious heart problems. Best alternative: Use acetaminophen (Tylenol) for pain. It’s the safest oral option in pregnancy. For localized pain, try cold packs, gentle massage, or pregnancy support belts.Antiviral Creams for Cold Sores and Herpes
If you have a history of cold sores, pregnancy can trigger outbreaks. The good news? Topical antivirals are mostly safe. Safe options:- Acyclovir cream: Used for herpes simplex (cold sores). Minimal absorption. Studies show no increased risk of birth defects.
- Trichloroacetic acid: Used for warts. Safe in pregnancy when applied by a professional.
- Podofilox and podophyllin resin: These are used for genital warts but can be toxic to the fetus. Never use them during pregnancy.
What About OTC Products and Natural Remedies?
Just because something’s “natural” doesn’t mean it’s safe. Tea tree oil? Aloe vera? Witch hazel?- Aloe vera gel: Safe for minor burns or rashes. Avoid oral aloe.
- Tea tree oil: Diluted topical use (1-5%) is generally fine for acne or fungal spots. Don’t use undiluted or near the eyes.
- Witch hazel: Safe for hemorrhoids or irritated skin. No systemic absorption.
- Essential oils: Skip them unless approved by your OB. Many (like rosemary, basil, cinnamon) can stimulate contractions or affect hormones.
When to Call Your Doctor
You don’t need to panic over every little rash. But call your OB or dermatologist if:- A rash spreads quickly or looks infected (red, warm, oozing)
- You used a cream you weren’t supposed to-especially retinoids or strong steroids
- You’re using any topical medication for more than two weeks without improvement
- You have severe itching all over your body, especially at night (could be cholestasis of pregnancy)
Key Takeaways: What to Remember
- Topical meds are usually safer than pills-but not all are safe.
- Avoid topical retinoids (tretinoin, adapalene) completely during pregnancy.
- Benzoyl peroxide, clindamycin, azelaic acid, and low-dose hydrocortisone are safe for acne and eczema.
- Clotrimazole and miconazole are best for yeast infections.
- Avoid topical NSAIDs after 30 weeks.
- Read labels. Many OTC products contain hidden risky ingredients.
- When in doubt, ask your doctor or pharmacist. Don’t guess.
Most women who use approved topical treatments during pregnancy have healthy babies. The goal isn’t to avoid all medications-it’s to use the right ones, the right way, at the right time.
Is hydrocortisone cream safe during pregnancy?
Yes, low-potency hydrocortisone cream (1%) is considered safe for short-term use on small areas during pregnancy. It’s commonly used for eczema, bug bites, and mild rashes. Avoid using it on large areas or for long periods, and never apply it to the breasts before nursing. Stronger steroids (like clobetasol) should only be used under medical supervision.
Can I use acne cream with benzoyl peroxide while pregnant?
Yes, benzoyl peroxide is one of the safest acne treatments during pregnancy. Only a small amount (under 5%) is absorbed into the bloodstream, and no birth defects have been linked to its use. It’s often recommended as a first-line treatment for pregnancy acne. Use it as directed-usually once or twice daily-and avoid combining it with other harsh products.
Are topical retinoids dangerous during pregnancy?
Yes. Topical retinoids like tretinoin, adapalene, and tazarotene should be avoided during pregnancy. Even though they’re applied to the skin, case reports link them to rare birth defects when used in early pregnancy. The American College of Obstetricians and Gynecologists recommends stopping them before trying to conceive. If you used one before realizing you were pregnant, don’t panic-most women in these cases have healthy babies-but tell your doctor right away.
Can I use antifungal cream for a yeast infection while pregnant?
Yes, clotrimazole and miconazole are the preferred antifungal treatments for vaginal yeast infections during pregnancy. They’re available as creams, suppositories, or tablets and have been used safely for decades. Nystatin is also safe and often used for oral thrush. Avoid econazole in the first trimester and use it only if needed later in pregnancy.
Is it safe to use topical NSAIDs like diclofenac gel when pregnant?
Use with caution. Topical NSAIDs like diclofenac gel are absorbed in small amounts and may be safe before 30 weeks. But after 30 weeks, they can cause the baby’s ductus arteriosus (a heart blood vessel) to close too early, leading to serious complications. The American Academy of Family Physicians advises avoiding them in the third trimester. For pain, acetaminophen and physical therapies are safer choices.
What should I do if I accidentally used a risky cream during early pregnancy?
Don’t panic. Most topical medications have very low absorption, and many women who accidentally use a risky cream still have healthy babies. Stop using the product immediately and contact your doctor or midwife. They can assess the specific medication, how much you used, and when you used it. In most cases, no further action is needed, but your provider may recommend extra monitoring. The InfantRisk Center (1-800-822-2336) also offers free expert advice for pregnancy medication concerns.

 Tadalista Professional vs Other ED Drugs: Full Comparison
Tadalista Professional vs Other ED Drugs: Full Comparison
 Cerebral Aneurysm: Understanding Rupture Risk and Modern Treatment Options
Cerebral Aneurysm: Understanding Rupture Risk and Modern Treatment Options
 Methimazole Allergy: Symptoms and Management
Methimazole Allergy: Symptoms and Management
 Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
 How Disulfiram Helps Treat Alcohol-Induced Liver Disease
How Disulfiram Helps Treat Alcohol-Induced Liver Disease
BETH VON KAUFFMANN
December 16, 2025 AT 14:26Let’s be real-most of this is just rehashing what OB-GYNs have been saying for decades. Benzoyl peroxide? Safe. Retinoids? Avoid. NSAIDs after 30 weeks? Yeah, we know. But nobody mentions the elephant in the room: the FDA’s pregnancy categories are obsolete. The real risk stratification is based on pharmacokinetics, not outdated letter grades. And yet, clinics still use Category B like it’s gospel. The 2016 JDD review cited? Solid, but it’s not the final word. We need more longitudinal data on azelaic acid and clindamycin in the third trimester. Also, why is nystatin listed as safe for oral thrush but not for vaginal use? That’s inconsistent.
And don’t get me started on ‘natural’ remedies. Tea tree oil at 1-5%? That’s a 10% dilution. You’re not applying it to your forearm-you’re putting it near your vulva. No data on mucosal absorption? Still calling it ‘safe’? That’s lazy.
Also, why no mention of the 2021 Lancet study on transdermal absorption through compromised skin? Eczema patients absorb 3x more. This whole guide feels like it was written for women with mild acne, not those with full-body dermatitis.
Bottom line: If you’re using anything topically for more than 14 days, you’re already in the danger zone. Stop self-diagnosing. Call your dermatologist. Or better yet, the InfantRisk Center. They’ve seen it all.
Donna Packard
December 18, 2025 AT 00:30This was so helpful. I was terrified to use anything for my pregnancy acne, but now I feel like I can breathe again. Thank you for breaking it down so clearly. I’ve been using the 5% benzoyl peroxide for two weeks and my skin is actually calming down. No more hiding behind makeup every day.
Also, the part about moisturizers with ceramides? I started using one last week and my eczema hasn’t flared once. Small wins, you know?
Patrick A. Ck. Trip
December 19, 2025 AT 19:37Thank you for this post. I am a first time father and i read this to my wife before bed. She was very stressed about her rash and i didn’t know what to say. This helped me understand what is safe and what to avoid. I think the part about topical NSAIDs was the most important-i had no idea diclofenac gel could affect the baby’s heart. We will be using the cold pack now instead. Also, the InfantRisk number is saved in my phone. Thank you for being so thorough.
ps. i think you meant ‘ductus arteriosus’ not ‘ductus arterioles’-but i’m no doctor, just a guy trying to help.
Peter Ronai
December 20, 2025 AT 08:59Oh, here we go again-the ‘safe topical’ myth. Let me guess, you’re also going to tell me that ‘it’s just a cream’ so it’s fine to use retinoids if you’re ‘careful’? Please. The data is clear: transdermal absorption isn’t linear. It’s exponential when you have broken skin, heat, occlusion, or a placenta that’s been hijacked by progesterone. You think 1% absorption is safe? That’s the same percentage that caused the first documented case of fetal hydantoin syndrome in the 70s. And now you’re waving around azelaic acid like it’s organic kale?
And don’t even get me started on ‘natural’ remedies. Tea tree oil is a hormone disruptor. It’s been shown in vitro to bind to estrogen receptors. You think your 1% dilution is safe? Try telling that to the fetal liver enzymes trying to metabolize it. This isn’t skincare-it’s fetal roulette.
And who wrote this? Someone who’s never held a newborn with a cardiac defect? Because if you’re not terrified of every single topical, you’re not paying attention.
Also, why no mention of the 2023 meta-analysis on clotrimazole and preterm birth? Oh right-because it’s inconvenient. This post is a placebo dressed in citations.
Michael Whitaker
December 22, 2025 AT 01:07As someone who has spent over a decade in maternal-fetal pharmacology, I must say this post is both commendable and dangerously incomplete. You cite the JDD review, yet omit the 2020 Cochrane meta-analysis on topical corticosteroid use and fetal growth restriction, which showed a dose-response relationship even with low-potency agents when applied to >10% body surface area over >3 weeks. You mention ceramides as ‘essential’-correct-but fail to note that many commercial ceramide creams contain parabens and phthalates, which are endocrine disruptors. You recommend benzoyl peroxide, yet ignore the fact that its degradation product, benzoic acid, crosses the placenta and can alter fetal acid-base balance in late gestation.
And while you correctly flag retinoids, you do not address the legal liability of dermatologists who prescribe them ‘off-label’ during pregnancy, nor the fact that many OTC products contain retinyl palmitate-hidden under ‘vitamin A derivatives.’
So yes, the advice is mostly right. But the lack of nuance is what kills people. This isn’t a blog-it’s a clinical decision support tool. And if you’re not citing the actual pharmacokinetic models, you’re doing harm by omission.
Brooks Beveridge
December 22, 2025 AT 12:03Hey, I just wanted to say thank you for writing this. I’m a doula, and I’ve seen so many pregnant people panic over rashes or acne-like they’re doing something wrong just because their body is changing. This guide feels like a warm hug wrapped in science. 🤗
I especially love how you didn’t just say ‘avoid everything’-you gave real options. My client last week was using a steroid cream she found online, scared to stop because she thought she’d break out worse. We switched her to ceramide moisturizer + 1% hydrocortisone on tiny spots only. She cried when her skin cleared. That’s the power of good info.
And yes, the InfantRisk Center? I send everyone there. Free. Confidential. No judgment. They’re angels in lab coats. 🙏
Keep doing this work. You’re changing lives, one cream at a time.
Anu radha
December 23, 2025 AT 10:39I am from India and I use only coconut oil for my skin. Is it safe? I hear many say it is good but I am scared. My friend used cream and baby got rash. I don't want that. Please tell me.
Jigar shah
December 25, 2025 AT 02:25While the article provides a solid overview, it lacks quantitative context for absorption rates. For instance, benzoyl peroxide’s 5% systemic absorption is cited, but no reference is made to the actual serum concentration thresholds associated with teratogenicity. The same applies to azelaic acid-while classified as Category B, its placental transfer coefficient (Kp) in human placental perfusion models is 0.18, which is higher than many assume. The omission of pharmacokinetic parameters limits clinical applicability.
Additionally, the distinction between ‘topical’ and ‘mucosal’ application is critical: vaginal application of clotrimazole results in significantly higher local concentrations than dermal application, yet the systemic exposure remains negligible. This nuance is absent.
Finally, the recommendation to avoid tea tree oil is reasonable, but the absence of data on its metabolites (terpinen-4-ol) in amniotic fluid is a gap. While anecdotal safety exists, evidence-based thresholds are needed.