When a pharmacist fills a prescription for NTI generics, they’re not just handing out a cheaper version of a drug-they’re managing a high-stakes balancing act. A small change in blood concentration can mean the difference between effective treatment and life-threatening complications. For drugs like warfarin, levothyroxine, and phenytoin, the margin for error is razor-thin. And yet, across hospitals and community pharmacies, pharmacists are reporting growing unease about how these generics are being handled.
What Makes a Drug an NTI Drug?
Narrow Therapeutic Index (NTI) drugs are those where even minor changes in dosage or absorption can lead to serious harm. Think of it like driving a sports car with no cruise control-small steering adjustments matter a lot. The FDA doesn’t publish an official list, but it flags certain drugs in the Orange Book with a therapeutic equivalence code. If a drug has an ‘A’ code, it’s considered interchangeable. But for NTI drugs, even an ‘A’ code doesn’t guarantee safety in practice.
Drugs like warfarin (a blood thinner), levothyroxine (for thyroid function), and phenytoin (for seizures) fall into this category. Their therapeutic window is tiny. For warfarin, a 10% difference in bioavailability can push a patient’s INR out of range, leading to clots or bleeding. For levothyroxine, a slight shift can cause fatigue, weight gain, or even heart rhythm problems. These aren’t theoretical risks. Between 2020 and 2024, the FDA’s adverse event database recorded 1,247 incidents linked to NTI generic substitutions-more than triple the number for non-NTI generics.
Why Are NTI Generics Different?
Standard generic drugs must show bioequivalence within 80-125% of the brand-name version. That’s a 45% range. For NTI drugs, the FDA recommends a much tighter window: 90-111%. That’s less than half the variability allowed for most generics. But even that narrower standard isn’t foolproof.
Here’s the problem: multiple manufacturers can make the same NTI generic. One batch might be 95% bioavailable. Another, made by a different company or even a different production line, might be 107%. Both meet FDA requirements. But for a patient on warfarin, that 12% difference could mean switching from a safe INR of 2.5 to a dangerous 4.2. And patients often don’t know they’ve been switched-pharmacists are legally allowed to substitute unless the prescriber says otherwise.
A 2024 study from the University of Florida found that 34% of pharmacists would never automatically substitute a warfarin generic. For non-NTI drugs, that number was just 8%. The gap tells you everything.
What Pharmacists Are Seeing in Real Life
It’s not just data-it’s stories.
A hospital pharmacist in Ohio reported three cases in six months where patients were switched from one warfarin generic to another, then ended up in the ER with bleeding. Their INR levels spiked overnight. No dose change. No new meds. Just a different generic.
On Reddit’s r/pharmacy, a thread about phenytoin level instability after a generic switch got 287 upvotes. Pharmacists shared how patients went from stable seizure control to having breakthrough seizures after a pharmacy switched to a cheaper generic. One wrote: “We had to run labs every 48 hours for a month just to stabilize him.”
Community pharmacists hear it from doctors too. A 2025 survey by the National Community Pharmacists Association found that 73% of independent pharmacies had received direct requests from prescribers to avoid substituting NTI generics. Warfarin topped the list (68%), followed by levothyroxine (52%) and carbamazepine (47%).
And it’s not just about switching between brands. Switching between lots from the same manufacturer can cause issues too. The FDA reported that 23% of NTI drug shortages were worsened by inconsistent switching between different generic suppliers.

The Cost-Savings Trap
Generics save money. That’s the point. NTI generics cost 80-85% less than their brand-name counterparts. For patients on long-term therapy, that’s huge. One pharmacy owner said switching to a generic levothyroxine cut patient abandonment by 35%. That’s a win.
But here’s the catch: the savings don’t always translate to better outcomes. When a patient has to go back to the ER because their INR went haywire, the cost of that one visit can wipe out months of savings. And that’s not even counting lost workdays, emergency transport, or long-term complications.
NTI drugs make up only 6% of all generic prescriptions, yet they account for 22% of pharmacist substitution concerns. They’re a small slice of the market-but a high-risk one.
State Laws Are a Patchwork
There’s no national standard for NTI generic substitution. As of January 2025, only 28 states have laws restricting automatic substitution for NTI drugs. In 22 of those, the prescriber must specifically note “dispense as written” or “no substitution.” Six states ban automatic substitution entirely.
That means a patient in California might get the same generic every time. A patient in Texas might get a different one every refill-with no one telling them. Pharmacists are stuck in the middle. They know the risks, but they’re often legally required to substitute unless told not to.
And even when prescribers write “no substitution,” pharmacies still switch. Why? Because insurance companies push for the cheapest option. If the brand is more expensive, the pharmacy might be forced to call the doctor for prior authorization. That delays care. Patients get frustrated. Pharmacists feel powerless.
What Pharmacists Are Doing About It
Despite the system’s flaws, many pharmacies are taking matters into their own hands.
The ASHP’s 2025 toolkit recommends sticking to a single generic manufacturer for each NTI drug. Sixty-three percent of hospital systems now do this. They track which generic a patient is on and refuse to switch unless absolutely necessary. Some pharmacies even keep a log-like a medication passport-so patients know exactly which version they’re taking.
Therapeutic drug monitoring is critical. Pharmacists are now routinely checking INR levels, thyroid hormone levels, or phenytoin concentrations after a switch. One hospital implemented a 48-hour protocol: after any NTI generic change, the pharmacist calls the patient, checks labs, and confirms stability before letting the refill go through.
Pharmacy residency programs are catching up too. Eighty-one percent now include specialized NTI drug training. That’s up from 45% just five years ago. Pharmacists are learning to read lab trends, understand chiral separations, and spot bioequivalence red flags.
What’s Changing in 2025 and Beyond
The FDA announced a new bioequivalence framework in April 2025, targeting 12 high-priority NTI drugs with stricter standards by 2026. That’s a step forward. But pharmacists are skeptical. The current 90-111% range still allows for a 21% variation. For some drugs, that’s too wide.
Then there’s Medicare’s new price negotiation program. Three NTI drugs-warfarin, levothyroxine, and phenytoin-are among the first 10 selected. The catch? Reimbursement delays of up to 21 days. That’s a death sentence for small pharmacies. If they can’t afford to stock these drugs for three weeks, patients go without. Lisa Schwartz of the NCPA warned that this could trigger shortages worse than what we’ve seen.
And supply chains? 80% of NTI generics are finished overseas. A single factory shutdown in India or China can ripple across the U.S. market. The FTC is investigating group purchasing organizations for manipulating NTI drug pricing and availability. The system is fragile.
Where Do We Go From Here?
Most pharmacists aren’t against generics. They’re against the illusion of interchangeability when it comes to NTI drugs.
They want:
- Clearer, stricter bioequivalence standards
- Consistent state laws requiring prescriber consent before substitution
- Transparency about which manufacturer’s generic is being dispensed
- Pharmacist-led stewardship programs to monitor patients after switches
- Supply chain protections to prevent shortages
One thing is clear: NTI drugs aren’t like other generics. They need a different approach. Until then, pharmacists will keep watching labs, calling prescribers, and praying the next refill doesn’t push a patient over the edge.
What Patients Should Know
If you’re on warfarin, levothyroxine, or another NTI drug:
- Ask your pharmacist which generic you’re getting-and stick with it.
- Don’t assume “generic” means identical. Ask if it’s the same brand as last time.
- Monitor symptoms closely after any switch: fatigue, dizziness, irregular heartbeat, bleeding, or seizures.
- Request that your prescriber writes “dispense as written” on the prescription.
- Keep a list of your medications, including the manufacturer name if possible.
You don’t need to fight the system alone. But you do need to be informed.

 Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
 Buy Cheap Generic Tylenol Online - 2025 Guide
Buy Cheap Generic Tylenol Online - 2025 Guide
 How to Manage Exercise-Induced Asthma Without Ventolin: Proven Warm-Ups, Cromolyn, and Preventive Tips
How to Manage Exercise-Induced Asthma Without Ventolin: Proven Warm-Ups, Cromolyn, and Preventive Tips
 Rheumatoid Arthritis Medications: How DMARDs and Biologics Interact in Treatment
Rheumatoid Arthritis Medications: How DMARDs and Biologics Interact in Treatment
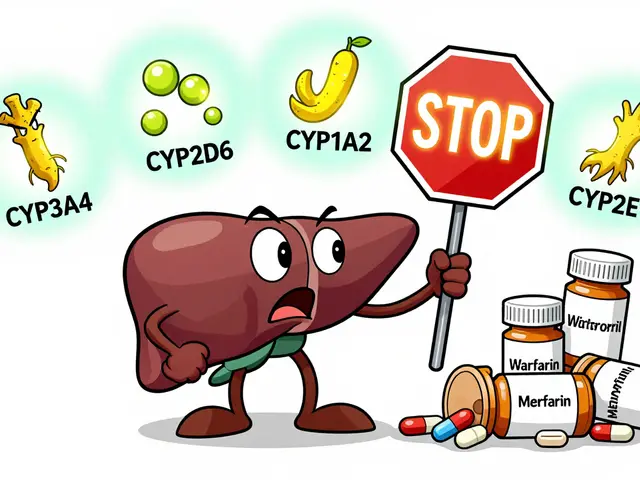 Goldenseal and Medications: What You Need to Know About Liver Enzyme Interactions
Goldenseal and Medications: What You Need to Know About Liver Enzyme Interactions
Zoe Brooks
January 18, 2026 AT 17:52Just had my mom switch to a new generic levothyroxine last month. She went from feeling fine to exhausted, gaining 8 lbs, and crying for no reason. Took three weeks and three lab visits to get back to baseline. Why the hell are we gambling with people’s health over $2 a pill? 🤦♀️
Aysha Siera
January 20, 2026 AT 15:59Big Pharma and the FDA are in bed together. The real story? They let cheap generics in so they can push the expensive brand names later when the patient crashes. You think this is about safety? Nah. It’s about profit cycles. Watch the next recall - it’ll be the same plant in India that made the last one. 🕵️♀️
Eric Gebeke
January 22, 2026 AT 01:28People who don’t understand pharmacology shouldn’t be allowed to make decisions about medication. If you can’t handle the fact that generics aren’t identical, maybe you shouldn’t be on life-saving drugs at all. It’s not rocket science - just follow your labs and stop blaming the pharmacist. You’re the reason healthcare costs are insane.
Joni O
January 23, 2026 AT 06:52i just wanted to say thank you to all the pharmacists out there who call patients after a switch. i had no idea you were doing that. my dr never told me to ask, but my pharmacist did - and she called me 2 days later to check my INR. i cried. you’re the real heroes. ❤️
Max Sinclair
January 24, 2026 AT 15:56This is such a well-researched post. I’ve seen this in my own family - my uncle’s phenytoin levels went wild after a pharmacy switch, and no one told him it wasn’t the same brand. The fact that pharmacists are legally forced to substitute unless explicitly told not to is a systemic failure. We need national standards, not a patchwork of state laws.
Nishant Sonuley
January 25, 2026 AT 21:06Let’s be real - the whole system is designed to make you think you’re saving money when you’re actually just getting a gamble with your life. One generic might be fine, the next one might be a different crystal structure, different fillers, different dissolution rates - and you won’t know unless you’re literally reading the FDA’s bioequivalence reports. And who has time for that? The real solution? Stop outsourcing everything to countries with zero oversight. But hey, that’s just me being idealistic, right?
Emma #########
January 27, 2026 AT 14:11I work in a hospital pharmacy. We stopped automatic substitution for NTI drugs two years ago. No more surprises. No more ER visits from our patients. It’s extra work, but it’s worth it. The families thank us. The doctors thank us. The patients live longer. Sometimes doing the right thing is just… inconvenient.
Andrew McLarren
January 28, 2026 AT 19:40It is imperative to acknowledge the regulatory framework’s current limitations in ensuring bioequivalence for narrow therapeutic index agents. The 90–111% interval, while an improvement over standard generics, remains insufficiently stringent to guarantee clinical equivalence across heterogeneous manufacturing processes. A paradigm shift toward individualized pharmacokinetic monitoring is not merely advisable - it is ethically obligatory.
Andrew Short
January 29, 2026 AT 01:56Stop coddling patients. If you can’t handle switching generics, you shouldn’t be on these drugs. You’re not special. Your thyroid isn’t a snowflake. This is why America is broke - people think they’re entitled to brand-name drugs because they ‘feel better.’ Get a lab test. Take the pill. Stop whining.
Chuck Dickson
January 30, 2026 AT 09:07Hey everyone - I’m a pharmacy resident, and we just finished our NTI drug rotation. The training is wild. We learn how to read dissolution profiles, spot chiral impurities, and even track batch numbers like detectives. Pharmacists aren’t just dispensers - we’re clinical guardians. If your pharmacy switches your warfarin without telling you, ask for the manufacturer name. You’ve got a right to know. And if they push back? Tell them to call me. I’ll explain it to them.
Robert Cassidy
January 31, 2026 AT 13:42Let’s not pretend this is about safety. It’s about control. The government wants you dependent on their system. They let cheap generics in so you can’t leave the system. You think they care if you bleed out from warfarin? No. They care if you stop taking pills and start asking questions. The real danger isn’t the generic - it’s the lie that it’s ‘the same.’
Dayanara Villafuerte
February 1, 2026 AT 13:21My aunt got switched to a new levothyroxine and started having panic attacks. We traced it to the manufacturer - it was a different one from her old bottle. Now she keeps the box. Every time. I made her a little card with the name and batch #. She carries it like a talisman. 💊🩵
Andrew Qu
February 2, 2026 AT 22:14One thing I’ve learned: if a patient is stable on a generic, don’t switch it. Period. It’s not about the brand - it’s about consistency. I’ve seen patients on the same generic for 10 years. No issues. Then a new batch comes in from a different supplier, and boom - labs go sideways. It’s not the drug. It’s the variability. We track every batch now. It’s a pain, but it’s saving lives.
kenneth pillet
February 4, 2026 AT 21:58Been a pharmacist for 18 years. Seen this movie 100 times. Same script. Same outcome. The only thing that changes is the name on the bottle. I stopped arguing with insurance. Now I just write ‘dispense as written’ on every NTI script. And I tell every patient to check the bottle. If it’s different, they call me. Simple. No drama. Just safety.