Sleep Duration & Fertility Impact Calculator
This tool estimates how your nightly sleep duration impacts your fertility potential based on current research. Enter your average sleep hours per night below to see the recommended impact on hormone balance and conception odds.
Your Sleep-Fertility Report
Understanding the link between sleep fertility can change the way you plan for a family. A solid night’s rest isn’t just about feeling fresh - it directly feeds the hormones, cells, and rhythms that determine whether you can conceive.
Key Takeaways
- Both quantity and quality of sleep shape hormone balance, which is essential for sperm production and ovulation.
- Less than 6hours or more than 9hours of sleep each night can lower fertility odds.
- Shift work, high stress, and poor bedroom habits disrupt the body’s natural clock and hurt reproductive health.
- Simple changes - dark room, consistent bedtime, limited caffeine - boost sleep quality and improve fertility markers.
- Track sleep for a few weeks; if problems persist, consult a specialist who can test hormone levels and sleep patterns.
How Sleep Influences Hormones and Fertility
Sleep is a physiological state that allows the body to repair, consolidate memory, and regulate the endocrine system. During deep REM cycles, the brain releases Melatonin, a hormone that signals darkness and helps synchronize the Circadian Rhythm. This rhythm acts like a master clock, timing everything from cortisol spikes to the release of sex hormones such as estrogen, progesterone, and testosterone.
When sleep is fragmented, cortisol - the stress hormone - stays elevated, and Hormone production becomes erratic. Elevated cortisol suppresses luteinizing hormone (LH) and follicle‑stimulating hormone (FSH), both crucial for ovulation and sperm maturation. In men, chronic sleep loss reduces testosterone levels by up to 15% and lowers Sperm Quality, affecting count, motility, and morphology.

What the Research Says
A 2023 meta‑analysis of 18 cohort studies involving over 150,000 participants found a “U‑shaped” relationship between sleep duration and pregnancy rates. Couples in which both partners slept 7-8hours per night had a 22% higher chance of conceiving within a year compared to those sleeping less than 6hours or more than 9hours.
In men, a 2022 Australian study measured semen parameters after a 4‑week sleep‑restriction protocol (5hours/night). Results showed a 12% drop in total sperm count and a 9% decline in progressive motility. Women in the same study experienced a 14% reduction in the number of mature follicles during the menstrual cycle.
Shift‑work research adds another layer. Nurses working rotating night shifts displayed a 31% increase in anovulatory cycles and a 27% rise in early miscarriage rates, directly linked to disrupted melatonin secretion and altered estrogen‑progesterone ratios.
Major Risk Factors That Sabotage Fertility Sleep
- Insufficient or excessive sleep: Both extremes confuse hormone feedback loops.
- Irregular schedules: Night‑shift or on‑call jobs break the circadian rhythm.
- High Stress levels: Chronic cortisol spikes suppress reproductive hormones.
- Unhealthy body composition: A high BMI (>30) is associated with sleep apnea, which reduces oxygen flow and hormonal balance.
- Age: As Age rises, sleep quality naturally declines, compounding fertility challenges.
Practical Sleep Hygiene for Better Fertility
Below are evidence‑backed habits you can start tonight.
- Set a consistent bedtime. Aim for the same sleep window (e.g., 10pm-6am) even on weekends. Consistency strengthens the circadian rhythm.
- Create a dark, cool bedroom. Use blackout curtains and keep the temperature around 18‑20°C. Darkness spikes melatonin, while a cooler room deepens REM sleep.
- Limit screen exposure. Blue‑light wavelengths suppress melatonin; switch off phones, tablets, and TVs at least 60minutes before bed.
- Watch caffeine and alcohol. Avoid caffeinated drinks after 2pm and keep alcohol to a minimum; both can fragment sleep cycles.
- Incorporate a wind‑down ritual. Light stretching, meditation, or reading signals the brain that it’s time to transition.
- Exercise earlier in the day. Moderate aerobic activity boosts deep sleep, but vigorous workouts within two hours of bedtime can raise heart rate and delay sleep onset.
- Manage stress proactively. Techniques such as diaphragmatic breathing, progressive muscle relaxation, or journaling lower cortisol levels before sleep.
For couples trying to conceive, consider synchronizing sleep patterns. Shared bedtime routines improve relational intimacy and reduce nighttime stress, both of which positively affect hormone balance.
Tracking Sleep and Knowing When to Seek Help
Using a wearable or smartphone app for at least two weeks gives you baseline data on total sleep time, sleep efficiency, and REM proportion. Look for these red flags:
- Sleep efficiency below 85% (spending a lot of time awake in bed).
- Frequent awakenings (more than three per night).
- Daytime fatigue lasting over an hour despite a full night’s rest.
If any of these persist, schedule a consultation with a reproductive endocrinologist or a sleep specialist. Blood tests can reveal hormone levels (testosterone, LH, FSH, estradiol, progesterone) while a polysomnography can identify sleep‑apnea or periodic limb movement disorder - both known to impair fertility.
Recommended Sleep Duration vs. Fertility Impact
| Sleep Hours (per night) | Typical Hormone Profile | Fertility Effect |
|---|---|---|
| 5or less | Low testosterone, high cortisol | Reduced sperm count, lower ovulation frequency |
| 6‑7 | Improving testosterone, moderate cortisol | Gradual rise in conception odds |
| 7‑8 (optimal) | Balanced testosterone, estrogen, progesterone | Highest natural conception rates |
| 9or more | Potential oversleeping‑related hormone dip | Small decline in fertility odds |
Frequently Asked Questions
Can a single night of bad sleep really affect my chances of getting pregnant?
One night of poor sleep won’t ruin fertility, but chronic patterns disrupt hormone cycles. Consistently low sleep quality over weeks can lower ovulation frequency and sperm quality, making conception harder.
Is it better for fertility to sleep on the left side?
There’s no solid evidence that side‑sleeping directly boosts fertility. However, left‑side sleeping can improve circulation and reduce heartburn, which may make sleep more comfortable for pregnant women.
How does melatonin supplementation affect fertility?
Low‑dose melatonin (0.5‑3mg) taken 30minutes before bed can improve sleep onset and has been shown in a 2021 pilot study to modestly raise IVF success rates by enhancing embryo implantation timing. Always discuss with a doctor before adding supplements.
Do naps interfere with fertility‑focused sleep goals?
Short power naps (10‑20minutes) early in the day usually don’t harm nighttime sleep quality. Longer naps after 3pm can delay sleep onset and reduce REM, potentially weakening hormone rhythms.
What sleep‑related medical conditions should I rule out when trying to conceive?
Sleep apnea, restless‑leg syndrome, and chronic insomnia are the top conditions linked to reduced fertility. A sleep study can diagnose apnea, while cognitive‑behavioral therapy is effective for chronic insomnia.

 Transform Your Health with Gossypol – The Game-Changing Supplement
Transform Your Health with Gossypol – The Game-Changing Supplement
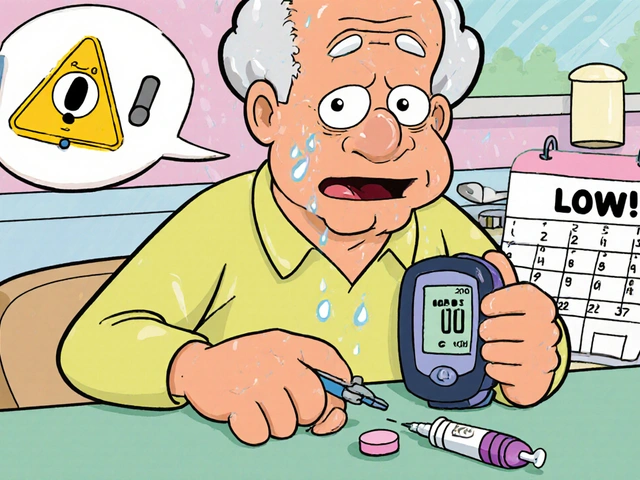 Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
 Buy Cheap Generic Atenolol Online - Safe Tips & Best Prices
Buy Cheap Generic Atenolol Online - Safe Tips & Best Prices
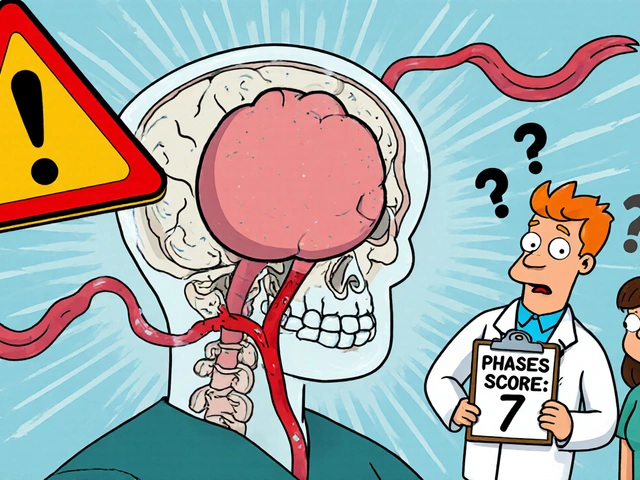 Cerebral Aneurysm: Understanding Rupture Risk and Modern Treatment Options
Cerebral Aneurysm: Understanding Rupture Risk and Modern Treatment Options
Kyle Olsen
October 5, 2025 AT 23:33While the correlation between sleep duration and reproductive hormones is well-documented, one must not overlook the confounding variables such as diet, stress, and underlying health conditions. The literature you cited indeed suggests a “U‑shaped” curve, yet the effect size remains modest, especially when controlling for socioeconomic status. Moreover, the mechanistic pathways involving melatonin and cortisol are far more intricate than a simple duration metric can capture. In short, adequate sleep is a component of fertility, but it is not a panacea.
Sarah Kherbouche
October 7, 2025 AT 03:20Honestly, your “well‑documented” claim is just a glorified excuse for people who cant get enough sleep because they’re lazy, and you’re ignoring the real issue-nutritional deficiencies in our country. This whole thing is overhyped.
MANAS MISHRA
October 9, 2025 AT 10:53Thanks for laying out the data. I’d add that tracking sleep consistency over a few cycles can reveal patterns that a single night’s average hides. For couples trying to conceive, synchronizing bedtime can also improve relational stress, which in turn benefits hormone balance. Using a wearable to monitor REM proportion can be especially enlightening.
Lawrence Bergfeld
October 11, 2025 AT 18:26Great summary; remember: consistent bedtime-same hour every night; cool dark room-around 18‑20°C; limit blue light-no screens 1 hour before sleep; regular exercise-morning or afternoon; stress‑relief-meditation or breathing exercises. These steps boost REM, balance cortisol, and support fertility.
Chelsea Kerr
October 14, 2025 AT 02:00Absolutely love the practical checklist! 🌙💤 It’s amazing how a few simple tweaks-like blackout curtains and a short power‑nap-can make a big difference for anyone trying to start a family. 😊 Remember, the goal is consistency, not perfection.
Tom Becker
October 16, 2025 AT 09:33Yo, you think those “simple tweaks” are enough? The pharma industry doesn’t want you to know that many sleep aids actually mess with melatonin receptors, lowering fertility on purpose. Wake up, folks-question the “standard” advice.
Laura Sanders
October 18, 2025 AT 17:06It is imperative to recognize that the reductionist view presented in many popular articles fails to capture the multifaceted nature of endocrinological regulation. Sleep, as a physiological construct, interacts with the hypothalamic‑pituitary‑gonadal axis in a bidirectional fashion. Empirical evidence demonstrates that nocturnal melatonin surges modulate GnRH pulsatility, thereby influencing downstream LH and FSH secretion. Concurrently, cortisol oscillations, which are attenuated by restorative sleep, exert inhibitory effects on gonadal steroidogenesis. The temporal alignment of these hormonal cascades is further complicated by peripheral feedback loops involving leptin and ghrelin, which themselves are sensitive to sleep architecture. Moreover, genetic polymorphisms in clock genes have been correlated with variances in reproductive outcomes, underscoring a heritable component to sleep‑fertility interplay. From a clinical perspective, the heterogeneity among patient populations necessitates individualized assessment rather than a one‑size‑fits‑all recommendation. For instance, individuals with obstructive sleep apnea present a distinct pathophysiological profile characterized by intermittent hypoxia, which can impair Leydig cell function and reduce testosterone synthesis. In contrast, shift workers experience circadian misalignment that desynchronizes melatonin rhythms, leading to suboptimal ovulatory timing. While the epidemiological data suggest a U‑shaped association, causality remains elusive due to residual confounding by lifestyle factors such as diet, alcohol intake, and psychosocial stress. Therefore, a comprehensive approach that integrates sleep hygiene with metabolic health is essential. Practitioners should consider adjunctive therapies, such as timed melatonin supplementation, calibrated to the patient’s chronotype. It is also prudent to evaluate comorbid conditions, including thyroid dysfunction and adrenal disorders, which may masquerade as sleep‑related fertility issues. Ultimately, the convergence of chronobiology and reproductive medicine offers fertile ground for future research, provided that methodological rigor is maintained. In summary, sleep is a pivotal, yet not solitary, determinant of reproductive potential.
Keith Laser
October 21, 2025 AT 00:40Sure, just add a blackout curtain and you’ll be sprinting to the nursery in no time.
Winnie Chan
October 23, 2025 AT 08:13Sleep more, stress less, good luck.
Kyle Rensmeyer
October 25, 2025 AT 15:46Honestly, the whole “7‑8 hours is optimal” narrative feels like a marketing ploy; I’ve seen people thrive on 10 hours, and you’ll still get a baby 😊.