Antibiotic Selection Calculator
Quick Summary
- Terramycin (generic tetracycline) is a broad‑spectrum antibiotic first approved in the 1950s.
- It works by blocking bacterial protein synthesis, but newer tetracyclines like doxycycline often offer better absorption and fewer side effects.
- Alternative classes-such as macrolides (azithromycin) or phenicols (chloramphenicol)-cover some of the same infections but differ in dosing convenience and safety profiles.
- Choosing the right drug depends on infection type, patient age, kidney function, and potential drug interactions.
- When possible, a newer tetracycline or a short‑course macrolide can spare patients the gastrointestinal upset common with Terramycin.
What is Terramycin?
Terramycin is the brand name for the generic antibiotic tetracycline hydrochloride. It belongs to the tetracycline class and was introduced in the United States in 1955. The drug is supplied as oral tablets (250mg) and as an injectable formulation for severe infections.
How does tetracycline work?
All tetracyclines, including Terramycin, share a single mechanism: they bind to the 30S ribosomal subunit of bacteria, preventing the addition of amino acids to the growing peptide chain. This halts protein synthesis and stops bacterial growth without directly killing the cells, making the drug bacteriostatic.
Typical uses for Terramycin
Terramycin is most often prescribed for:
- Acute uncomplicated urinary tract infections (UTIs)
- Respiratory tract infections such as Mycoplasma pneumoniae
- Sexually transmitted infections like chlamydia (when alternatives are unavailable)
- Acne vulgaris in low‑dose, long‑term regimens
- Rickettsial diseases (e.g., RockyMountain spotted fever)
Because the drug is excreted unchanged in the urine, dose adjustments are needed for patients with impaired renal function.
Key alternatives to Terramycin
When doctors weigh options, they look at three main axes: spectrum of activity, safety, and convenience. Below are the most common substitutes.
Doxycycline is a second‑generation tetracycline that offers better oral bioavailability (≈90% vs 60% for Terramycin) and a longer half‑life, allowing once‑daily dosing.
Minocycline is another newer tetracycline, noted for its high lipid solubility, making it especially effective against intracellular pathogens.
Chloramphenicol belongs to the phenicol class. It is a broad‑spectrum agent but carries a rare risk of aplastic anemia, limiting its use to severe infections where other drugs fail.
Azithromycin is a macrolide that works by blocking the 50S ribosomal subunit. It is prized for its short, three‑day course and minimal GI upset.
| Drug | Class | Spectrum | Typical Dosage | Key Advantages | Common Side Effects |
|---|---|---|---|---|---|
| Terramycin | Tetracycline | Broad (Gram‑positive, Gram‑negative, atypicals) | 250mg PO q6h | Low cost, widely available | nausea, photosensitivity, teeth staining in children |
| Doxycycline | Second‑gen. tetracycline | Similar to Terramycin, better for intracellular organisms | 100mg PO bid | High bioavailability, once‑daily possible, less GI upset | photosensitivity, esophagitis |
| Minocycline | Second‑gen. tetracycline | Strong against acne‑related bacteria, good intracellular penetration | 100mg PO bid | Effective for acne, crosses blood‑brain barrier | dizziness, vestibular symptoms, hyperpigmentation |
| Chloramphenicol | Phenicol | Very broad, including anaerobes | 500mg PO q6h | Excellent CSF penetration | aplastic anemia (rare), gray baby syndrome |
| Azithromycin | Macrolide | Broad, especially good for respiratory pathogens | 500mg PO daily x3 days | Short course, good tolerance | mild GI upset, QT prolongation in high‑risk patients |
How to choose the right antibiotic
Think of the decision as a three‑step checklist:
- Identify the pathogen. If a lab confirms a tetracycline‑sensitive organism, Terramycin remains an option. For atypical or intracellular bugs, doxycycline or minocycline often outperform the older drug.
- Assess patient factors. Children under 8years and pregnant women should avoid tetracyclines because they can cause permanent tooth discoloration and affect bone growth. In those cases, azithromycin or chloramphenicol (if benefits outweigh risks) may be safer.
- Consider practicality. Dosing frequency matters-four times daily for Terramycin can be a compliance nightmare. A once‑daily doxycycline regimen usually leads to better adherence.
When all else fails, culture and sensitivity testing can pinpoint the most effective drug and reduce unnecessary broad‑spectrum exposure.
Managing side effects and drug interactions
Terramycin’s most frequent complaints are stomach upset and extreme sensitivity to sunlight. Here are quick fixes:
- Take the tablet with a full glass of water and stay upright for at least 30minutes.
- Avoid dairy, antacids, and iron supplements within two hours of dosing-they bind to tetracycline and cut absorption.
- Use sunscreen (SPF30+) and wear protective clothing when outdoors.
- If nausea persists, ask the prescriber about switching to doxycycline, which many patients tolerate better.
Both Terramycin and newer tetracyclines interact with warfarin, increasing bleeding risk. Routine INR monitoring is advised if the two are combined.
Practical tips for clinicians
When you write a prescription, include these three notes:
- “Take with food or a full glass of water; avoid dairy within 2h.”
- “Do not expose to direct sunlight; wear sunscreen.”
- “If you are pregnant, breastfeeding, or a child under 8y, consider alternative therapy.”
These reminders cut down on the most common complaints you’ll hear during follow‑up calls.
Frequently Asked Questions
Is Terramycin still used in modern practice?
Yes, but mostly in settings where cost is a major factor or when newer tetracyclines are unavailable. Many clinicians favor doxycycline for its once‑daily dosing and lower GI side‑effect rate.
Can I take Terramycin with calcium supplements?
No. Calcium chelates tetracycline and can reduce absorption by up to 50%. Separate the doses by at least two hours.
What makes doxycycline better for acne?
Doxycycline penetrates skin oil glands more effectively and is taken less frequently, which improves adherence for the long‑term treatment acne often needs.
Are there any severe risks with chloramphenicol?
The biggest concern is rare but fatal aplastic anemia. Because of that, it’s reserved for life‑threatening infections when no safer options exist.
How long does a typical Terramycin course last?
Usually 7‑10days for most bacterial infections, but some urinary‑tract infections may need up to 14days based on severity.
 Bemzocaine and Inflammation: A Promising Connection
Bemzocaine and Inflammation: A Promising Connection
 2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
 Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
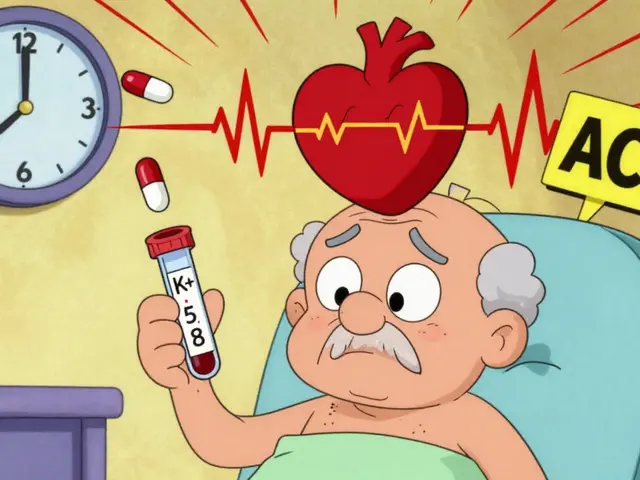 ACE Inhibitors with Spironolactone: Managing the Hyperkalemia Risk
ACE Inhibitors with Spironolactone: Managing the Hyperkalemia Risk
 Top 10 Reliable Alternatives to Drugwatch for Drug Information
Top 10 Reliable Alternatives to Drugwatch for Drug Information
Steve Holmes
October 17, 2025 AT 03:36Wow, this guide really breaks down the differences between Terramycin and the newer tetracyclines, and I have to say, the high bioavailability of doxycycline is a game‑changer, especially for patients who struggle with the four‑times‑daily dosing of Terramycin, plus the reduced GI upset is a big win for compliance, and the cost factor still keeps Terramycin relevant in some settings, but overall the convenience of doxycycline often outweighs the cheap price tag of the old drug!
Tom Green
October 17, 2025 AT 13:20Good points, Steve! In practice, I always remind the team to consider patient age and renal function before defaulting to Terramycin; a mixed approach-starting with a broad‑spectrum agent and de‑escalating based on culture results-helps balance efficacy and safety, especially in community clinics where cost constraints exist.
James Falcone
October 17, 2025 AT 23:03Listen up, folks-our great nation’s doctors should prioritize American‑made antibiotics, and while Terramycin is a classic, we’ve got to push for modern, home‑grown options like doxycycline that give us fewer side‑effects and better adherence, so let’s keep our prescriptions proudly American and up‑to‑date!
Valerie Vanderghote
October 18, 2025 AT 08:46Honestly, reading through the comparison reminded me of the countless evenings I’ve spent wrestling with patients who cannot tolerate the relentless nausea that Terramycin brings, and I’ve seen how the simple act of taking the pill with a full glass of water can sometimes feel like a small mercy amidst the larger battle against infection, yet even that mercy is overshadowed by the fact that the drug’s binding to calcium, iron, and even certain antacids can shave half the dose’s effectiveness, which is why timing becomes a ritualistic dance of separation that adds stress to already fraught treatment courses, and the photosensitivity-oh, the photosensitivity!-it forces patients to become nocturnal beings, dodging sunlight like vampires, which can be both mentally exhausting and socially isolating, especially for those who simply want to enjoy a sunny day without fearing blistering rashes, and let’s not forget the dental staining that haunts children under eight, leaving permanent reminders of a medication they never chose, so when we consider alternatives like doxycycline, with its higher bioavailability and once‑daily dosing, we’re not just prescribing a drug, we’re offering a lifeline that respects a patient’s daily routine, their dignity, and their ability to maintain normalcy, and while the cost of newer tetracyclines can be higher, the hidden costs of non‑adherence-hospital readmissions, prolonged illness, and diminished quality of life-are far greater, thus the decision matrix should always tip in favor of the drug that minimizes collateral damage, and in the end, it’s not just about bacterial kill rates, it’s about preserving the human experience amidst the necessary medical interventions.
Michael Dalrymple
October 18, 2025 AT 18:30From a coaching perspective, the key is to empower clinicians with clear guidelines: assess pathogen susceptibility, weigh patient-specific factors, and prioritize regimens that enhance adherence; philosophically, medicine is a partnership-every prescription should reflect a shared commitment to both efficacy and the patient’s lived experience.
RJ Samuel
October 19, 2025 AT 04:13Interesting take, Michael-though I’d argue that the “cost vs convenience” debate sometimes blinds us to the creative possibilities of repurposing older agents when supply chains falter, especially in remote settings where a reliable generic like Terramycin can be a lifeline.
Kate Marr
October 19, 2025 AT 13:56Terramycin is still used in some clinics. 😎
Frank Diaz
October 19, 2025 AT 23:40While many laud the convenience of doxycycline, let us not be blinded by its sleek dosing schedule; the pharmacodynamic nuances matter, and the reality is that every tetracycline carries a burden-photosensitivity, GI upset, or rarely, hepatotoxicity-so prescribing with a blind eye to these trade‑offs reflects a superficial understanding of therapeutic stewardship.
Richard O'Callaghan
October 20, 2025 AT 10:46i think the cuurent guidlines are confusng, the table is abundnnt with infomration but it could be more short and easier to read, also the sideeffects list could be breifed, the longer text make it hard to find key point for a busily doctor, maybe use bullet or highlight.