Every year, over 1.5 million people in the U.S. get the wrong medication, wrong dose, or wrong instructions from the pharmacy. Most of these errors are preventable - and the final line of defense isn’t the pharmacist. It’s you. Right before you walk out the door, you have 30 seconds to stop a mistake that could land you in the hospital. This isn’t about being suspicious. It’s about being smart.
Why Your Last Check Matters
Pharmacists are trained professionals. They double-check prescriptions, scan barcodes, and run drug interaction alerts. But they’re also human. They work long shifts. They juggle multiple patients. And sometimes, even with all the tech, something slips through. A 2024 study in JAMA Internal Medicine found that when patients do a quick, structured check before leaving, they catch 87% of dispensing errors. That’s not luck. That’s a system that works. The FDA, ISMP, and APhA all agree: patient verification is the last, most powerful safety net. You don’t need to be a doctor. You don’t need to memorize drug names. You just need to ask yourself seven simple questions - and take the time to look.The 7-Point Medication Bag Audit
Here’s what to check, one by one. Do this slowly. Don’t rush. If you’re in a hurry, wait. This takes 30 seconds. It could save your life.- Is your name on the label? Exactly as it appears on your ID? This sounds obvious, but it’s one of the most common errors. In 2024, the NCPA found that 12.7% of mistakes happened because someone got a prescription meant for a person with a similar name - like “John Smith” instead of “Jon Smith.” Look at the full legal name. Not just the first name. Not just the last name. Full name. If it’s wrong, don’t leave.
- Does the medication name match what your doctor prescribed? Check both the brand name and the generic. If your doctor wrote “Lisinopril,” but the bottle says “Zestril,” that’s fine - they’re the same drug. But if it says “Lisinopril” and you were supposed to get “Lisinopril-HCTZ,” that’s a problem. Look at the prescription slip or your doctor’s note. If you don’t have it, call the pharmacy back. Don’t guess.
- Is the dosage strength correct? This is where things get dangerous. A 5 mg pill is not the same as a 50 mg pill. A 10 mL dose is not the same as 1 mL. The ISMP reports that 32% of serious medication errors involve wrong strength. Look at the label: “5 mg,” “100 mg,” “5 mL.” Now look at the pill or liquid. Is it what you expected? If your blood pressure pill used to be white and now it’s blue and bigger, ask why.
- Does the quantity match what was prescribed? If your doctor ordered 30 pills, but you got 60, that’s a red flag. If you were supposed to get 10 tablets but the bottle has 25, that’s a mistake. CMS data shows 8.3% of errors are wrong pill counts. This can lead to overuse or running out too soon. Count them if you can. If it’s a liquid, check the volume on the bottle versus what was written.
- Is the expiration date at least six months away? For chronic medications - like blood pressure, diabetes, or thyroid pills - you should never get a bottle that expires in two months. Medications lose potency over time. USP guidelines say most drugs are safe for a while past expiration, but if you’re taking it daily, you want it to last. If the date is too close, ask for a newer batch. Pharmacists can usually swap it.
- Does the pill or liquid look right? Color, shape, markings - all matter. If you’ve taken metformin for years and it’s always been a white, round tablet with “500” stamped on it, but now it’s a blue oval with “M5,” that’s not normal. Use the FDA’s Drugs@FDA database on your phone or ask the pharmacist for a picture. Many pharmacies now have printed reference sheets behind the counter. Don’t be shy. Say: “This doesn’t look like my usual pill.”
- Do the instructions match what your doctor told you? “Take one by mouth daily” is different from “Take one twice daily.” “Take with food” is different from “Take on an empty stomach.” The APhA reports that 14.2% of errors involve wrong directions. Did your doctor say “take in the morning”? Is the label saying “take at bedtime”? If it’s not matching, ask. Don’t assume the pharmacist knows what your doctor meant.
What If You’re Not Sure?
You don’t have to know everything. You just have to ask. If something feels off - even if you can’t put your finger on why - say so. Say: “I’m not comfortable with this. Can we double-check?” Many pharmacies now have staff trained to help. The 2024 Pharmacy Technician Certification Board requires all certified techs to assist with patient verification. Ask for help. Bring your old bottle. Show them your prescription. Use the free MedCheck app from the FDA - it lets you scan the barcode on your pill bottle and instantly compares it to your prescription record.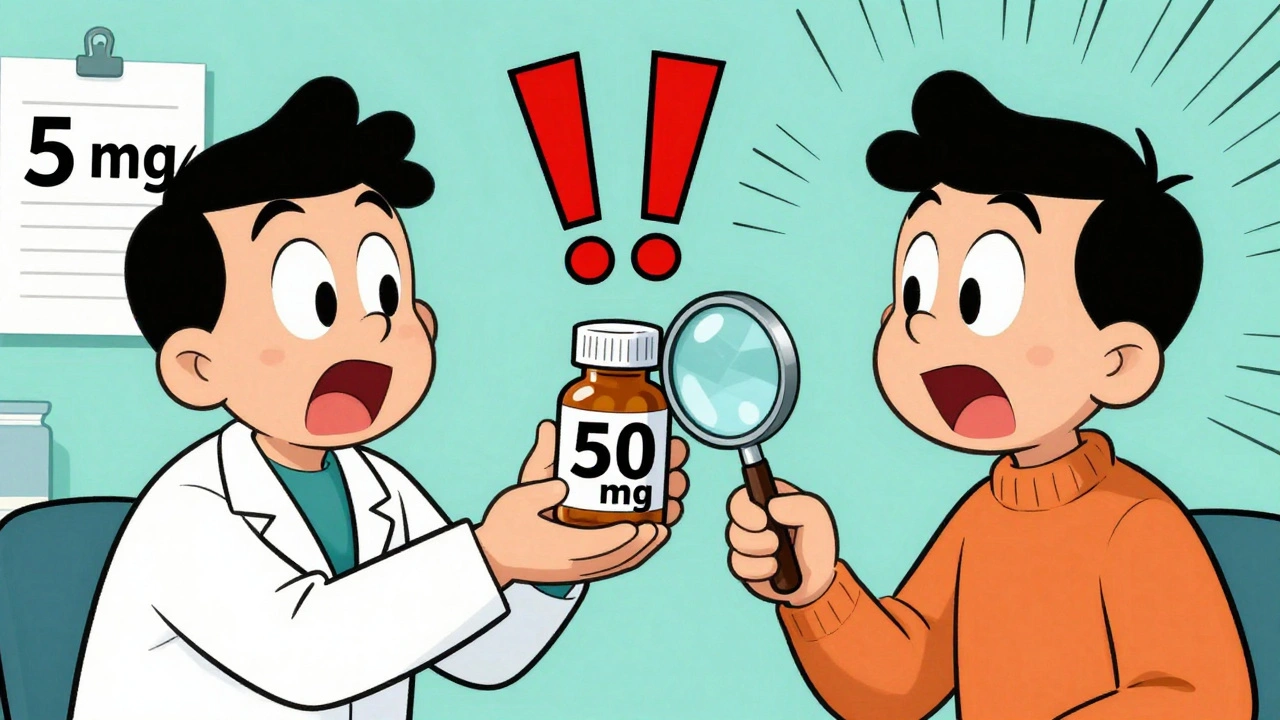
What About Vision or Memory Problems?
If you’re over 65, have macular degeneration, or struggle with memory, you’re not alone. 63% of serious medication errors happen in older adults. But you still have rights. Ask for:- Larger print labels
- Magnifying cards (available free at 67% of Walgreens locations since March 2024)
- Blister packs with days of the week printed on them
- Verbal confirmation from the pharmacist before you leave
What Doesn’t Work
Don’t rely on:- Just glancing at the label while walking out
- Assuming “it looks right”
- Trusting the pharmacy “always gets it right”
- Using apps if you’re not tech-savvy - they’re helpful, but not required
Real Stories, Real Results
In January 2025, a woman in Pennsylvania caught a fatal error. Her warfarin dose was supposed to be 5 mg. The label said 50 mg. She noticed the difference because she checked the number. She called the pharmacy. They had dispensed the wrong strength to three other patients that day. They fixed it. On Reddit, a mom saved her child from a 10x overdose. The label said “give 5” - but didn’t say “5 mL.” She knew the concentration was 50 mg per 5 mL. She asked: “Is this 5 mL or 5 mg?” The pharmacist realized they’d left off the unit. That’s the power of asking.What’s Changing in 2025
The FDA just mandated that all prescription labels must include a QR code by the end of 2025. Scan it, and you’ll get a video explanation of your medication - in plain language, with pictures. Pharmacies are also rolling out voice-guided checks via Alexa and Google Home for seniors. These tools help, but they don’t replace your eyes and your voice. The goal is simple: zero preventable errors. And the most effective tool isn’t a robot. It’s a patient who knows what to look for.Start Today
Print out the seven points. Tape them to your fridge. Save them on your phone. Practice once. Next time you pick up a prescription - even if it’s the same one you’ve taken for years - stop. Look. Ask. Confirm. You’re not just getting medicine. You’re getting your safety back.What should I do if I find a mistake in my medication?
Stop. Don’t take the medication. Call the pharmacy immediately. Ask them to confirm the prescription with your doctor. Most pharmacies will replace the medication at no cost. If they refuse or seem dismissive, ask to speak to the pharmacist-in-charge. Document what you found - take a photo of the label. Report it to the FDA’s MedWatch program online. Your report helps prevent this from happening to someone else.
Do I need to audit every prescription, even if it’s the same drug?
Yes. Even if you’ve taken the same medication for years, the manufacturer, dose, or formulation can change. A pill that was white last time might now be blue. The strength might be different. The instructions might have been updated. Never assume it’s the same. Always check.
Can I ask the pharmacist to verify the medication with me?
Absolutely. In fact, the 2024 NACCHO Pharmacy Audit Guide recommends it. Say: “Can we go over the name, dose, and instructions together?” Many pharmacists now do this as part of their standard process. You’re not bothering them - you’re helping them do their job better. Shared verification reduces errors by 73%.
What if the label is too small to read?
Ask for a larger print label. Most pharmacies offer this for free. If they don’t, ask for a magnifying card - many Walgreens and CVS locations keep them behind the counter. You can also request a blister pack with printed days of the week, or ask for a verbal explanation. Your vision matters. The pharmacy is required to accommodate you.
Is this really necessary if I trust my pharmacist?
Trust is good. Verification is better. Even the best pharmacists make mistakes - and they’re often caused by system issues, not carelessness. A 2024 Johns Hopkins study showed that when patients checked their meds, they caught errors that even the pharmacy’s own systems missed. Your check is the final safety net. Don’t skip it.
Are there free tools to help me audit my meds?
Yes. The FDA’s free MedCheck app lets you scan your pill bottle’s barcode and instantly compares it to your prescription. You can also use the Drugs@FDA website to look up what your pill should look like. Many pharmacies offer free wallet cards with the 7-point checklist - ask for one. And if you’re over 65, AARP offers a free Medication Safety Kit with magnifiers and checklists mailed to your home.

 Medication Safety at Home: A Step-by-Step Guide to Preventing Errors
Medication Safety at Home: A Step-by-Step Guide to Preventing Errors
 FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
 Levonorgestrel Explained: Complete Guide to Uses, Safety, and How It Works
Levonorgestrel Explained: Complete Guide to Uses, Safety, and How It Works
 Drug-Disease Interactions: How Your Health Conditions Can Change How Medications Work
Drug-Disease Interactions: How Your Health Conditions Can Change How Medications Work
 Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Cole Newman
December 13, 2025 AT 06:01Bro, I once got a bottle of metformin that was shaped like a tiny football and neon green. I thought it was candy. My grandma almost ate it. I called the pharmacy and they were like, 'Oh yeah, we switched manufacturers.' No one told me. Never trust the label. Always check the damn thing. I keep a photo of my pills on my phone now. If it doesn't match, I walk back in and demand answers. No apology needed.
Casey Mellish
December 14, 2025 AT 22:51Brilliant breakdown. As an Australian who’s had to navigate the U.S. pharmacy system while visiting family, I’m stunned by how little emphasis is placed on patient verification here. In Australia, pharmacists routinely walk patients through their scripts - even for refills. This checklist should be mandatory in every pharmacy chain, not just a nice suggestion. Kudos for making it so clear and actionable. I’ve shared this with my sister in Texas.
Emma Sbarge
December 16, 2025 AT 17:06This is exactly why we need to stop letting foreign corporations run our healthcare. Big Pharma and CVS don’t care if you live or die - they care about profit margins. I got a 10x overdose on my thyroid med last year because the barcode got scanned wrong. The pharmacist shrugged and said, 'It happens.' No one gets fired. No one gets punished. We need real accountability, not some feel-good checklist. This post is good, but it’s Band-Aid on a bullet wound.
Tommy Watson
December 18, 2025 AT 00:54lol i just look at the bottle and go 'yep that's my name' and walk out. if i get sick i'll go to the er. why are you all so paranoid? i trust my pharmacist. also why does this post have 7 steps? i can't even remember my own birthday.
Donna Hammond
December 18, 2025 AT 09:30I’m a registered nurse and I use this exact 7-step method every time I pick up meds for my elderly parents. One time, I caught a mislabeled insulin vial - the label said 'Lantus' but it was actually 'Humalog.' The difference could’ve killed my dad. This isn’t paranoia - it’s survival. And if you’re over 65 or caring for someone who is, please, please do this. I’ve printed this checklist and taped it to my fridge. I even made a version with bigger fonts for my mom. You’re not being difficult - you’re being the hero in your own story.
Richard Ayres
December 19, 2025 AT 05:25This is one of the most thoughtful, well-researched, and practically useful posts I’ve seen on health safety in years. The data cited is compelling, the structure is logical, and the tone is neither alarmist nor dismissive. The inclusion of real-world examples - like the Pennsylvania woman and the Reddit mom - makes the risk tangible. It’s rare to see a piece that empowers without condescension. I’ve forwarded this to my entire family, including my teenage daughter who manages her own ADHD prescriptions. Thank you for taking the time to write this.
Sheldon Bird
December 20, 2025 AT 00:16YOU GOT THIS. 🙌
Look, I used to skip the check too - until my niece almost got the wrong antibiotic. Now I do the 7-step audit every single time, even for my daily blood pressure pill. It takes 30 seconds. That’s less time than it takes to scroll through TikTok. You’re not just protecting yourself - you’re teaching everyone around you to be vigilant. Keep doing the right thing. Your life matters. 💪
Karen Mccullouch
December 21, 2025 AT 22:42Oh my god, I’m so tired of this 'trust your pharmacist' nonsense. I work at a pharmacy. I’ve seen the chaos. They’re understaffed, overworked, and getting paid minimum wage to handle 50 scripts an hour. The system is broken - and we’re supposed to fix it with a checklist? No. We need federal regulation. We need mandatory verification protocols. We need to stop treating patients like babysitters for a broken industry. This post is helpful, but it’s a distraction from the real problem: capitalism in healthcare. And I’m done being polite about it.