What Happens During an FDA Inspection of a Generic Drug Facility?
If you run a generic drug manufacturing plant and you’ve received notice of an FDA inspection, don’t panic. Most facilities pass. In fact, over 90% of inspections in 2023 found no major violations. But passing isn’t luck-it’s preparation. The FDA doesn’t show up to catch you off guard. They show up because they’ve already reviewed your records, complaints, and past performance. Your job isn’t to hide anything. It’s to prove you’re in control.
The Four Types of FDA Inspections You Might Face
Not all inspections are the same. The FDA uses four main types, and knowing which one you’re dealing with changes how you prepare.
- Pre-Approval Inspection (PAI): This happens before your generic drug gets approved. The FDA wants to confirm your facility can actually make the product the way you described in your application. They’ll check if your equipment, processes, and testing methods match what you submitted. If your stability samples aren’t stored where you said they’d be, or if your analytical methods don’t match the ones on file, you’ll get flagged.
- Routine Surveillance Inspection: These happen every 2-3 years, depending on your risk profile. The FDA uses a risk-based model to pick which sites to inspect. High-risk products, past issues, or even anonymous tips can bump you to the top of the list. During these, inspectors use the 6-System approach: Quality, Facilities & Equipment, Materials, Production, Packaging & Labeling, and Laboratory Control. The Quality System is always checked-no exceptions.
- For-Cause Inspection: Triggered by something specific: a spike in adverse events, a whistleblower report, or a problem found in another facility using the same raw material. These are intense. The inspectors zero in on the area of concern, but they still look at your overall quality system. Don’t assume they’ll only check one room.
- Follow-Up Inspection: If you got a warning letter or an FDA 483 with serious findings, expect a return visit. The FDA wants to see if you fixed what was broken-or if you just wrote a pretty letter.
The 6-System Inspection: What They’re Really Looking For
The FDA doesn’t just walk through your plant and take pictures. They’re building a case. Every system they inspect tells them whether your quality culture is real-or just on paper.
- Quality System: This is the foundation. Do you have a qualified Quality Unit that can say no to production? 21 CFR 211.22(a) is the rule here. If your quality team doesn’t have authority, or if they’re being overruled by production managers, you’re already in trouble. They’ll ask to see your deviation logs, change controls, and CAPA records. Are these tracked? Are they closed? Or are they buried in a folder no one opens?
- Facilities & Equipment: Clean rooms aren’t just for show. They’ll check if your HVAC systems are validated, if your water systems are monitored daily, and if your equipment has been properly calibrated. Did you validate that autoclave after you moved it? If not, you’ll get a finding.
- Materials: Every raw material must be tested and approved before use. They’ll pull your supplier qualification files. Do you know where your active ingredients come from? Do you have certificates of analysis for every batch? If you’re sourcing from a new vendor without proper audit records, that’s a red flag.
- Production: They’ll follow a batch from start to finish. Did your operators follow the SOP? Was the mixing time recorded? Was the equipment cleaned according to protocol? They’ll compare your batch records to your validation reports. If your actual process doesn’t match what you validated, you’re not compliant.
- Packaging & Labeling: Wrong label? Wrong strength? Wrong expiration date? This is where patients get hurt. They’ll check your label reconciliation, your barcode scanning logs, and your complaint records for mislabeling. Even a single mismatch can trigger a recall.
- Laboratory Control: Your lab is where the truth comes out. They’ll pull your HPLC chromatograms, check your method validation reports, and ask to see your stability data. Are your samples stored under the conditions you filed with the FDA? Are your analysts trained? Are your instruments calibrated? If your data looks too perfect-too clean-investigators will suspect manipulation.
What Is an FDA 483? And What Happens After?
If the inspectors find problems, they’ll give you an FDA Form 483. It’s not a citation. It’s not a fine. It’s a list of observations. Each item references a specific regulation-like 21 CFR 211.194(a) for missing test records.
You have 15 business days to respond. Don’t wait until the last day. Your response needs to be specific: what you found, why it happened, how you fixed it, and how you’ll prevent it from happening again. Vague answers like “we’ve retrained staff” won’t cut it. Show them the training records. Show them the updated SOP. Show them the audit you did to verify it worked.
After your response, the FDA reviews everything. They look at your history, your product risk, and your corrective actions. If they’re not satisfied, you’ll get a Warning Letter. That’s when things get serious. The FDA will publicly post it. Your customers will see it. Your bank might ask questions.
How to Prepare: It’s Not About the Day of the Inspection
Most companies panic when they get the inspection notice. That’s too late. The best facilities operate in a permanent state of readiness.
- Run mock inspections quarterly. Bring in someone from another site or hire a consultant to play FDA. Don’t tell your staff it’s a drill. See what happens when they’re caught off guard.
- Keep your documentation clean. If your batch records are handwritten in pencil, if your SOPs are outdated, if your equipment logs are missing signatures-those are easy finds. Digital records aren’t mandatory, but they’re easier to defend.
- Train your team on the 6 systems. Your operators should know why they’re following a procedure, not just what to do. If they can explain the risk of skipping a step, they’re more likely to follow it.
- Design your facility for inspection. Make sure the inspector can walk through without disrupting production. Have clean, well-lit areas ready. No clutter. No hidden files. If they ask to see your deviation log, you should be able to pull it in under 30 seconds.

The New PreCheck Program: A Game Changer
In 2024, the FDA launched PreCheck-a program designed to help manufacturers avoid inspection surprises. If you’re building a new facility or scaling up, you can submit a Type V Drug Master File (DMF) early. This includes your facility layout, quality system design, and validation plans.
The FDA reviews it before you start production. They give you feedback. You fix issues before you invest millions in equipment. It’s not mandatory, but companies using it report fewer 483s and faster approvals. If you’re planning a new plant, this isn’t optional-it’s smart business.
What Happens If You Fail?
An “unacceptable” inspection result means your product can’t enter the U.S. market. You won’t get approval. Existing products might be detained at the border. You could face import alerts or even a consent decree.
But failure isn’t the end. The FDA offers Post-Warning Letter Meetings (PWLMs), finalized in June 2025. These are formal discussions where you can walk them through your corrections. It’s your chance to show you’ve changed-not just fixed, but improved.
The goal isn’t to scare you into submission. It’s to make sure the pills patients take are safe, effective, and consistent. If you’re doing that, you’ll pass. If you’re cutting corners, you’ll get caught.
Final Thought: Compliance Isn’t a Checklist
The FDA doesn’t care if you have the right forms. They care if you have the right culture. Do your people take pride in their work? Do they speak up when something’s wrong? Do you reward quality over speed?
Facilities with mature quality systems don’t just survive inspections. They thrive. Their teams know the rules because they live them. Their data tells a true story-not a rehearsed one.
So ask yourself: Is your facility ready for inspection-or are you just ready to answer questions?
Are FDA inspections announced in advance?
Most routine inspections are unannounced. The FDA gives no warning to prevent facilities from cleaning up or staging operations. Pre-Approval Inspections (PAIs) are scheduled in advance because they’re tied to a drug application. For-Cause inspections can be sudden, based on complaints or data anomalies.
Can a facility be inspected more than once a year?
Yes. High-risk facilities-those with past violations, complex products, or recent complaints-can be inspected multiple times a year. The FDA’s risk-based model prioritizes sites that need more oversight. A facility with a clean record might only see an inspection every 3 years. One with multiple 483s could be inspected every 6-12 months.
What’s the biggest mistake companies make during an FDA inspection?
Trying to hide or explain away problems instead of owning them. The FDA expects imperfections. What they don’t tolerate is lack of transparency. If you say, “We didn’t know that was required,” they’ll assume you don’t have a proper quality system. If you say, “We found this gap, here’s how we fixed it, and here’s how we’re preventing it,” you earn credibility.
Do inspectors check digital records and electronic signatures?
Yes. The FDA has been focused on data integrity since 2018. They’ll request access to your LIMS, ERP, or electronic batch records. They’ll check for audit trails, user access logs, and whether data can be deleted or altered without trace. If your system doesn’t have proper controls, it doesn’t matter how clean your paper records are-you’ll fail.
How long does an FDA inspection usually last?
Most inspections last 3-7 days. Complex facilities or those with multiple products may take longer. The length depends on how organized you are. If your documentation is clear and your staff is prepared, inspectors can move quickly. If they’re digging through files or chasing down answers, the inspection drags on-and the risk of finding more issues goes up.
Can a generic drug be approved without an FDA inspection?
No. Every facility producing a generic drug for the U.S. market must pass an FDA inspection. Even if your drug is bioequivalent and your application is perfect, the FDA won’t approve it unless they’ve verified your facility can consistently make it to specification. This applies to both U.S. and foreign facilities.
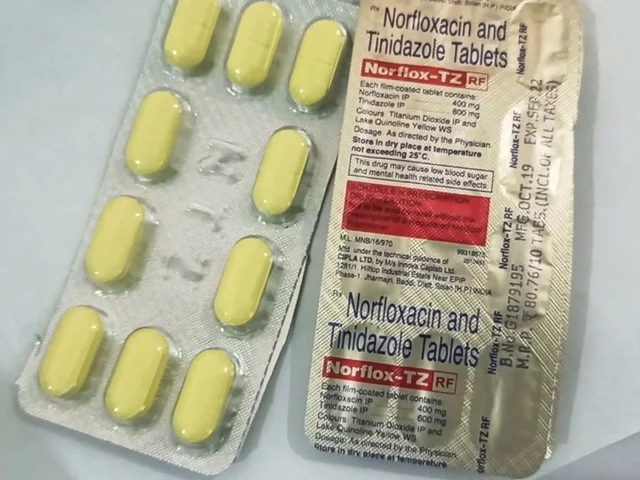 Norfloxacin and the management of bacterial skin infections
Norfloxacin and the management of bacterial skin infections
 Unlock the Power of Blessed Thistle: A Dietary Supplement for a Healthier You!
Unlock the Power of Blessed Thistle: A Dietary Supplement for a Healthier You!
 Food Environment: How to Set Up Your Home Kitchen to Support Weight Loss Goals
Food Environment: How to Set Up Your Home Kitchen to Support Weight Loss Goals
 Roccat Burst Pro Air Review: Revolutionizing Gaming with Lightweight, Wireless Design
Roccat Burst Pro Air Review: Revolutionizing Gaming with Lightweight, Wireless Design
 How to Buy Cheap Generic Crestor Online Safely
How to Buy Cheap Generic Crestor Online Safely
Chinmoy Kumar
February 3, 2026 AT 17:52Brett MacDonald
February 5, 2026 AT 11:24Solomon Ahonsi
February 5, 2026 AT 13:27George Firican
February 6, 2026 AT 11:05Murarikar Satishwar
February 7, 2026 AT 21:37Dan Pearson
February 9, 2026 AT 02:26Matt W
February 9, 2026 AT 12:00Hannah Gliane
February 10, 2026 AT 19:35