Levonorgestrel Effectiveness Calculator
How Effective Is Levonorgestrel?
Estimate the effectiveness of levonorgestrel emergency contraception based on how long after unprotected sex you take it. Effectiveness decreases the longer you wait.
When it comes to preventing an unintended pregnancy after unprotected sex, few names appear as often as Levonorgestrel a synthetic progestin used in emergency contraception and certain hormonal IUDs. This guide walks you through what the hormone does, when to take it, how effective it is, and what to watch out for.
What is Levonorgestrel?
Levonorgestrel belongs to the class of hormones called Progestin synthetic compounds that mimic the activity of natural progesterone. First approved for medical use in the 1970s, it has become a staple in both emergency contraception pills (often sold as “Plan B” or “Ella”) and the hormonal intra‑uterine device (IUD) marketed under names like Mirena.
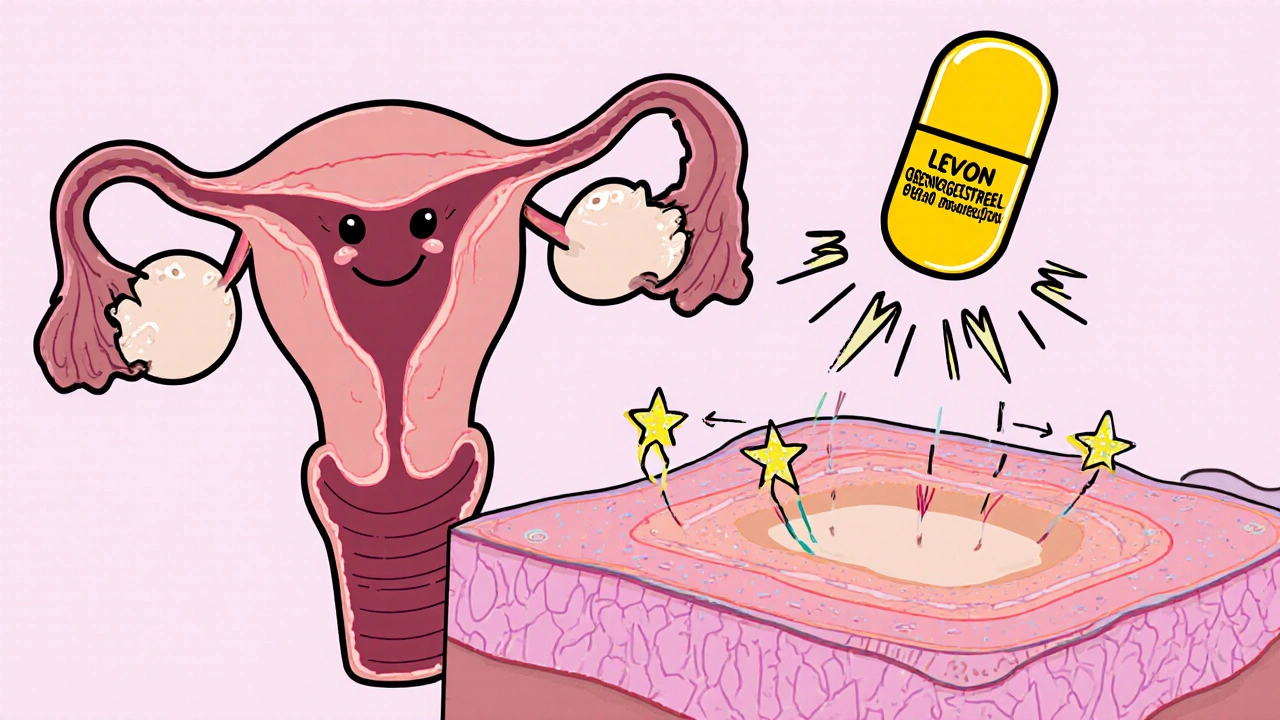
How Does Levonorgestrel Work?
In the body, levonorgestrel works by interfering with Ovulation the release of an egg from the ovary. If taken before the egg is released, the hormone can prevent it from reaching the fallopian tube, effectively stopping fertilization before it starts. When used after fertilization, it thickens cervical mucus and alters the uterine lining, making it less receptive to implantation.
Medical Uses of Levonorgestrel
There are three main ways levonorgestrel is prescribed:
- Emergency contraception a short‑term, high‑dose method to prevent pregnancy after unprotected sex. A single dose (1.5 mg) or two‑dose regimen (0.75 mg 12 hours apart) is typical.
- Hormonal IUD an intra‑uterine device that releases levonorgestrel over several years. These devices provide both ongoing birth control and a lighter, more predictable menstrual flow.
- Off‑label support for treating irregular menstrual cycles or endometriosis, though this is less common.
Dosage Forms and How to Take Them
Emergency contraception pills come in two common brands:
- Plan B One‑Step - 1.5 mg levonorgestrel in a single tablet.
- Ella - 1.5 mg levonorgestrel in a single tablet, approved for use up to 120 hours (5 days) after intercourse.
The IUD version, such as Mirena a levonorgestrel‑releasing intra‑uterine system, is inserted by a clinician and can remain effective for up to 5 years.
Effectiveness and Timing
When taken within 72 hours, levonorgestrel emergency pills reduce the chance of pregnancy by roughly 75‑89 %. The effectiveness drops after 72 hours but remains higher than doing nothing. The IUD, on the other hand, is over 99 % effective at preventing pregnancy from the moment of insertion.
If you’re wondering whether levonorgestrel is right for you, the key factor is how quickly you can access the pill. The sooner you take it, the better the odds.
Side Effects and Risks
Most people experience only mild, short‑term side effects such as:
- Nausea or mild stomach upset.
- Headache or dizziness.
- Temporary spotting or changes in menstrual timing.
Serious reactions are rare but can include severe abdominal pain (which may signal an ectopic pregnancy), allergic rash, or pronounced mood swings. Women who are pregnant, have uncontrolled hypertension, or have a history of blood‑clotting disorders should avoid levonorgestrel unless a doctor advises otherwise.
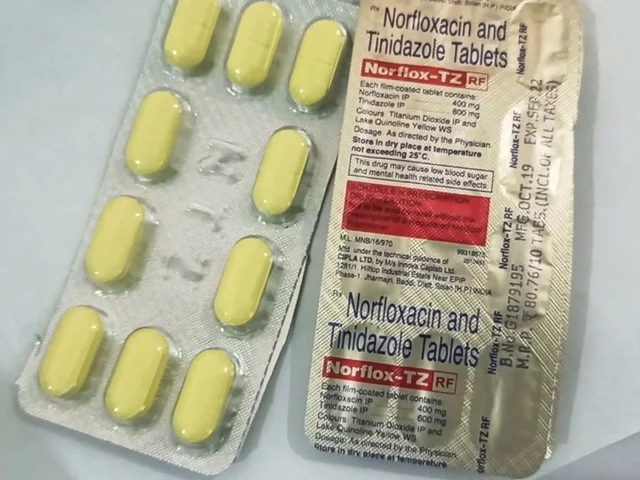
Drug Interactions and Precautions
Levonorgestrel’s efficacy can be lowered by certain medications that affect liver enzymes, especially:
- Rifampin (an antibiotic used for tuberculosis).
- Certain anti‑epileptic drugs like carbamazepine and phenytoin.
- St. John’s Wort, a popular herbal supplement.
If you’re on any of these, consider a copper IUD or a prescription‑only method like ulipristal acetate (another type of emergency pill).
Comparing Levonorgestrel with Other Options
| Method | Active Ingredient | Window of Use | Typical Failure Rate |
|---|---|---|---|
| Levonorgestrel pill | Levonorgestrel | Up to 120 hours (best < 72 h) | 0.9‑2 % |
| Ulipristal acetate (Ella) | Ulipristal | Up to 120 hours | 0.6‑1 % |
| Copper IUD | Copper (non‑hormonal) | Within 5 days | 0.1 % |
While levonorgestrel is widely available over the counter, the copper IUD offers the lowest failure rate. However, it requires a clinician for insertion and can cause heavier periods for some users.
Frequently Asked Questions
Can I use levonorgestrel if I am already pregnant?
No. Levonorgestrel will not terminate an existing pregnancy; it only works to prevent fertilization or implantation. If you discover you are pregnant, consult a healthcare provider about other options.
Will the pill cause my next period to be delayed?
It can. Some people get their period up to a week early or late. This is normal and does not mean the pill failed.
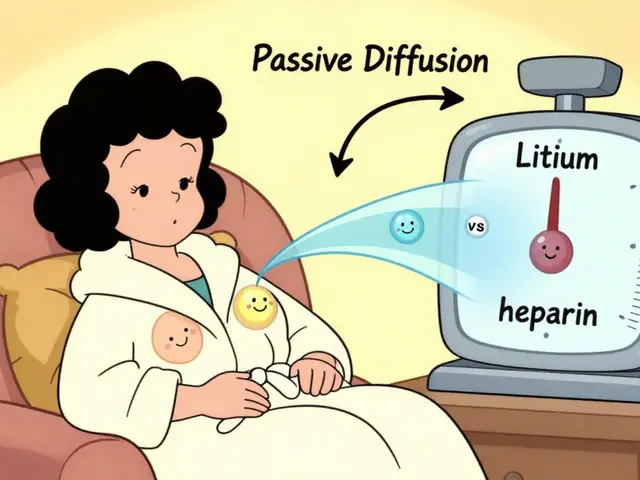
Is it safe to take levonorgestrel while breastfeeding?
Yes, the amount that passes into breast milk is minimal and not associated with adverse effects in infants. Nonetheless, discuss any concerns with your doctor.
How does levonorgestrel differ from the hormonal IUD?
The IUD releases a low, steady dose of levonorgestrel directly into the uterus, providing continuous birth control for years. The emergency pill delivers a high, single dose meant for one‑time use within a short window.
Can I take levonorgestrel if I have a history of blood clots?
Generally, a single emergency dose is considered low risk, but you should talk to a physician first because progestins can affect clotting factors in susceptible individuals.
Next Steps and Where to Get Levonorgestrel
In most countries, including Australia, levonorgestrel emergency pills are available without a prescription at pharmacies, clinics, and even some supermarkets. If you prefer a longer‑acting method, schedule an appointment with a GP or a family‑planning clinic to discuss IUD insertion.
Remember, the best protection is consistent, everyday use of a reliable contraceptive method. Levonorgestrel is a valuable safety net, but it’s not a substitute for regular birth control.

 Norfloxacin and the management of bacterial skin infections
Norfloxacin and the management of bacterial skin infections
 How Medications Enter Breast Milk and What It Means for Your Baby
How Medications Enter Breast Milk and What It Means for Your Baby
 Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
 Rheumatoid Arthritis: How Biologic DMARDs Can Lead to Disease Remission
Rheumatoid Arthritis: How Biologic DMARDs Can Lead to Disease Remission
 Bacterial vs. Viral Infections: What Sets Them Apart and How They're Treated
Bacterial vs. Viral Infections: What Sets Them Apart and How They're Treated
JessicaAnn Sutton
October 20, 2025 AT 13:01It is disconcerting that society continues to normalize the indiscriminate consumption of hormonal agents without rigorous moral scrutiny. The over‑the‑counter availability of levonorgestrel, while convenient, implicitly encourages a cavalier attitude toward reproductive responsibility. One must consider the ethical implications of treating profound biological processes as mere retail items. Consequently, a more educated discourse is essential to uphold the dignity of human life.
Israel Emory
November 1, 2025 AT 01:47While I respect the previous point-however, the practicality of emergency contraception cannot be dismissed; it provides a vital safeguard, especially when unplanned exposure occurs. Moreover, the timeliness of administration directly correlates with efficacy; therefore, accessibility remains paramount. Let us also acknowledge the scientific consensus that supports safe usage; any moralizing must be grounded in evidence. Finally, consider that stigmatizing the pill does more harm than good.
Sebastian Green
November 12, 2025 AT 15:34I appreciate how clearly the guide breaks down the mechanisms; it helps reduce anxiety for many. Knowing the timing window really eases the decision‑making process.
Wesley Humble
November 24, 2025 AT 05:21From a pharmacological standpoint, levonorgestrel functions primarily by inhibiting the luteinizing hormone surge, thereby preventing ovulation-a process well‑documented in endocrinology textbooks. Additionally, its secondary effects on cervical mucus viscosity and endometrial receptivity create a multi‑layered barrier against fertilization and implantation. The pharmacokinetics reveal a rapid absorption phase followed by hepatic metabolism via the CYP3A4 pathway, which explains the noted drug‑interaction profile with enzyme inducers such as rifampin and certain antiepileptic agents. Clinical trials have consistently demonstrated a reduction in pregnancy incidence ranging from 75% to 89% when administered within the recommended 72‑hour window, a statistic corroborated across diverse populations. Moreover, the comparative analysis between levonorgestrel and ulipristal acetate underscores the latter's marginally superior efficacy, yet the former's accessibility renders it a pragmatic first‑line option. Regarding safety, the adverse event spectrum is largely limited to transient gastrointestinal discomfort, mild headache, and brief menstrual irregularities-symptoms that resolve without intervention in the majority of cases. Rare but serious complications, such as ectopic pregnancy, warrant immediate medical attention and should be differentiated from common side effects. From a public health perspective, the over‑the‑counter model has been instrumental in increasing timely usage, thereby mitigating the societal burden of unintended pregnancies. Nevertheless, practitioners must remain vigilant about contraindications, particularly in individuals with uncontrolled hypertension or a history of thromboembolic disorders, due to the progestogenic influence on coagulation pathways. The guide’s inclusion of drug‑interaction data is commendable; clinicians should routinely review patient medication histories to preempt diminished efficacy. In summary, levonorgestrel represents a well‑characterized, efficacious, and generally safe emergency contraceptive, provided it is used according to established guidelines 😊.
barnabas jacob
December 5, 2025 AT 19:07yo, gotta say the guide is lit but it drops some heavy pharma jargon that most peeps might not vibe with. also, they kinda gloss over the fact that levonorgestrel can mess with your gut if you’re on antibiotics like rifampin. plus, the whole “it’s safe while breastfeeding” line feels like a blanket claim, no nuance. and don’t get me started on the copper iud vs. hormonal iud debate-people need real talk, not just stats.
jessie cole
December 17, 2025 AT 08:54Let’s take a step back and remember that empowerment comes from knowledge and support. While the guide’s technical depth is impressive, it’s essential to translate that into actionable advice that resonates with everyday experiences. Embrace the fact that you have options, and approach each decision with confidence and clarity. You are capable of navigating this with grace.
Kirsten Youtsey
December 28, 2025 AT 22:41One cannot ignore the insidious influence of pharmaceutical conglomerates that shape the narrative around emergency contraception. The commercial push for levonorgestrel appears meticulously orchestrated to promote dependency on synthetic hormones rather than holistic reproductive health. It is prudent to question the motives behind the widespread marketing of such products.
Matthew Hall
January 9, 2026 AT 12:27Seriously, the way big pharma spins these pills is straight out of a control‑freak playbook. You think it’s just about preventing a pregnancy, but there’s a whole agenda of keeping us hooked on a cycle of dependency. Wake up, folks! The drama isn’t just in the headlines-it’s in the hidden labs and the backdoor deals.
Demetri Huyler
January 21, 2026 AT 02:14From an American standpoint, it’s heartening to see that levonorgestrel remains readily available without prescription. This accessibility reflects our nation’s commitment to personal liberty and reproductive autonomy. While some criticize over‑the‑counter sales, the data clearly shows that timely use saves countless unintended pregnancies. Our healthcare system should continue to champion such pragmatic solutions.
Bobby Marie
February 1, 2026 AT 16:01Access is good, but affordability matters too.
Nicole Boyle
February 13, 2026 AT 05:47Observing the comparative efficacy data, it’s evident that the copper IUD exhibits a markedly lower failure rate, which aligns with the pharmacodynamic principle of localized spermicidal action. However, patient preference often skews towards systemic options due to perceived convenience, despite the marginally increased risk profile. This dichotomy underscores the importance of nuanced counseling that integrates both clinical evidence and individual lifestyle considerations.
Monika Bozkurt
February 24, 2026 AT 03:26Philosophically, the choice between systemic and intra‑uterine methods reflects a deeper dialogue about agency and embodiment. When individuals assert control over their reproductive trajectories, they engage in an act of self‑determination that transcends mere medical decision‑making. Therefore, providers must facilitate an environment where informed consent is truly informed, integrating both empirical data and the person’s existential framework.