Every year, millions of people take generic drugs because they’re affordable and effective. But what if the pill in your bottle isn’t what it claims to be? Fake generic drugs are a growing global crisis - not just a problem in faraway countries, but one that sneaks into pharmacies and online stores everywhere. These counterfeit medicines look real. They have the right color, shape, and packaging. But inside? They might have no active ingredient, too little, or worse - toxic chemicals. And they’re getting harder to spot.
How fake drugs are made
Counterfeit generic drugs don’t appear out of nowhere. They’re made in hidden labs, often in places with weak drug regulations. Think small factories in Southeast Asia, Eastern Europe, or parts of Africa. These aren’t high-tech labs with scientists in white coats. They’re basements, garages, or warehouses with basic equipment: mixing bowls, tablet presses, and printers. The goal? Copy the real thing as closely as possible - and save every penny.Take a common generic blood pressure pill, like losartan. The real version costs $0.10 per tablet. A fake one? It might cost $0.02 to make. The manufacturer skips the real active ingredient and uses cheap fillers - chalk, flour, or even sawdust. Sometimes they add a tiny bit of the real drug to trick tests. Other times, they use harmful substitutes like industrial chemicals. One 2021 study found that 77% of fake drugs seized were oral tablets - the most common form - and many targeted high-demand generics like antibiotics, antimalarials, and heart meds.
And the packaging? It’s scary accurate. Using commercial-grade printers and real packaging templates, counterfeiters replicate logos, fonts, and even batch numbers. A 2023 analysis by TrueMed Inc. found that 95% of fake drug packages look identical to the real thing under normal light. Even pharmacists can’t tell the difference without lab tools.
The three main ways fake drugs get into the supply chain
Counterfeit drugs don’t just show up on your pharmacy shelf. They slip in through cracks in the system. Here’s how:
- Parallel importation - This happens when drugs are bought legally in one country, then resold in another where regulations are looser. A batch of genuine pills might be mixed with fake ones at a warehouse. The fake ones look identical, so no one notices until patients stop responding to treatment.
- Grey market sales - Unauthorized distributors buy drugs from wholesalers, then sell them to pharmacies without proper documentation. These sellers often don’t verify the source. In 2022, the National Association of Boards of Pharmacy found that 95% of online pharmacies operating without licenses were selling fake drugs. Many of these sites look like real pharmacies - they even have fake certifications.
- Online pharmacies - This is the biggest loophole. People search for cheap meds online, click a link, and get a box in the mail. No prescription needed. No verification. In 2023, a Reddit user named u/PharmaWatcher posted about buying counterfeit Lipitor. The pills had the wrong scoring, a slightly different color, and dissolved too fast in water - a clear sign they weren’t real. He sent them to a lab. They contained no atorvastatin at all.
These aren’t rare cases. The U.S. Pharmacopeia’s database recorded over 1,200 incidents of fake or substandard drugs between 2013 and 2023. The top three targets? Cardiovascular drugs (28.7%), antibiotics (22.4%), and antimalarials (18.9%).
Why generics are the main target
Why not go after brand-name drugs like Viagra or Humira? Because they’re harder to copy legally. Brand-name drugs are protected by patents and monitored closely. Generics? They’re everywhere. The global generic drug market hit $438.7 billion in 2022. That’s a huge target. Companies making generics compete on price. To cut costs, some legitimate manufacturers cut corners. Counterfeiters? They cut everything.
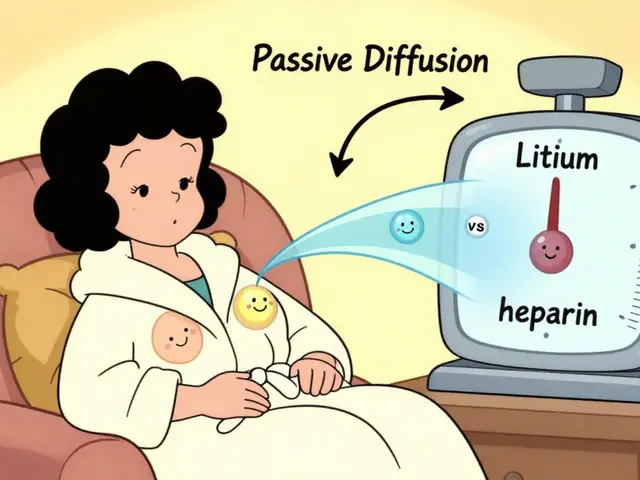
Plus, generics are often produced in multiple countries. One batch might come from India, another from China, another from Brazil. Each step adds a chance for fraud. A 2008 case in the U.S. showed how dangerous this can be: contaminated heparin - a blood thinner - came from a Chinese supplier. It had been adulterated with a chemical that caused 149 deaths. That wasn’t a fake drug. It was a real drug made with a fake ingredient. The same risk exists today.

How detection fails
You’d think drug regulators would catch these. But they don’t. Why? Because the system is broken.
Only 40% of countries have track-and-trace systems that follow drugs from factory to pharmacy. Of those, only 22 countries - out of 194 WHO member states - have fully working systems as of early 2023. That means most drugs move through the supply chain without a digital trail. No barcode. No serial number. No way to know if a batch was stolen, diverted, or swapped.
Even when systems exist, they’re not linked. A drug might be tracked in the U.S., but not in Nigeria. A wholesaler in Germany might have a scanner, but the pharmacy in Guatemala doesn’t. And counterfeiters know this. They ship drugs through countries with weak oversight, then repackage them for markets with stricter rules.
Testing is another problem. Labs can detect fake drugs - but only if they test. Most pharmacies don’t have the tools or budget. A 2022 survey of 1,200 pharmacists across 45 countries found that 68% had seen suspected counterfeit drugs. But 32% couldn’t tell the difference between real and fake without lab equipment.
What’s being done - and what’s not working
Some progress is being made. The EU’s Falsified Medicines Directive, rolled out in 2019, forced pharmacies to scan every package. Since then, counterfeit penetration in Europe has dropped by 18%. Companies like MediLedger are testing blockchain systems that track each pill from manufacturer to patient. In trials, they caught 97.3% of supply chain anomalies.
But these solutions cost money. Adding a hologram or DNA tag to a pill costs $0.02 to $0.05 per unit. For a generic drug that sells for $0.10, that’s a 50% cost increase. Most manufacturers won’t pay it. And in low-income countries, governments can’t afford it either.
Pharmaceutical companies like Pfizer have spent millions on anti-counterfeiting programs. Since 2004, they’ve stopped over 302 million fake doses from reaching patients. But they can’t do it alone. They need cooperation from customs, police, and online platforms - and that’s slow.
Meanwhile, criminals are adapting. In February 2023, Europol seized cancer drugs with AI-generated holograms. The fakes were so perfect, even trained inspectors missed them. AI can now design packaging that mimics every detail - down to the slight curve of a logo or the exact shade of blue on a blister pack.

What you can do
You can’t stop counterfeits alone. But you can protect yourself.
- Buy from licensed pharmacies only. If it’s not a physical store or a verified online pharmacy (like those listed by NABP), don’t trust it.
- Check the packaging. Compare it to a previous bottle. Look for spelling errors, mismatched fonts, or odd colors. If the tablets look different - smaller, smoother, or oddly shaped - ask your pharmacist.
- Don’t buy from social media or Google ads. Fake pharmacies use targeted ads. If the price seems too good to be true, it is.
- Report suspicious drugs. If something feels off, tell your pharmacist or local health authority. One report can trigger an investigation.
And if you’re taking life-saving meds - like insulin, antivirals, or heart drugs - never skip your refill. Going without can be deadly. Counterfeit drugs might not kill you right away. But they’ll make your condition worse. And that’s just as dangerous.
What’s next
The OECD predicts counterfeit drugs could make up 5-7% of global medicine sales by 2030 if nothing changes. That’s not a guess - it’s a projection based on current trends. The problem is growing faster than the solutions.
What’s needed? Global standards. Better tracking. Real penalties for violators. And more transparency. Right now, the system is a patchwork. A drug might be safe in one country, fake in another. A pharmacy might be licensed in one city, but illegal in the next.
Until we fix that, fake generics will keep slipping through. And people will keep getting sick - not because their disease is untreatable, but because the medicine they trusted never worked at all.
 Asthma in Children: How Spacers, Schools, and Care Plans Work Together
Asthma in Children: How Spacers, Schools, and Care Plans Work Together
 Zhewitra Oral Jelly (Vardenafil) vs Alternatives: What Works Best for ED
Zhewitra Oral Jelly (Vardenafil) vs Alternatives: What Works Best for ED
 Proven Strategies to Prevent Osteoporosis - A Complete Guide
Proven Strategies to Prevent Osteoporosis - A Complete Guide
 How Medications Enter Breast Milk and What It Means for Your Baby
How Medications Enter Breast Milk and What It Means for Your Baby
 Can Bioidentical Hormones Relieve Estrogen‑Related Vaginal Dryness & Itching?
Can Bioidentical Hormones Relieve Estrogen‑Related Vaginal Dryness & Itching?