Vaginal Dryness Improvement Calculator
Symptom Improvement Estimator
Based on clinical studies showing bioidentical estradiol improved vaginal dryness by 2.4 points on a 10-point scale
Results
Enter your current symptom scores to see potential improvement based on clinical data.
Vaginal dryness and itching can feel like an everyday nuisance, especially when estrogen levels dip during perimenopause or menopause. The question many ask is whether bioidentical hormones can actually smooth out those uncomfortable symptoms. Below we break down what bioidentical hormones are, how they interact with estrogen pathways, and what real‑world data say about their effectiveness for dryness and itching.
Understanding Estrogen‑Related Vaginal Dryness
When estrogen drops, the delicate lining of the vagina loses moisture, elasticity, and its natural protective barrier. This leads to a range of sensations - from a mild sandpaper feel to intense itching that disrupts sleep and intimacy.
Key players in this process include Estrogen is a hormone that regulates the growth and maintenance of vaginal tissue, blood flow, and mucus production. Low estrogen narrows blood vessels, reduces collagen, and dries out the epithelium. While estrogen itself can be prescribed in pills or creams, many women look for alternatives that feel more “natural” or less synthetic.
What Are Bioidentical Hormones?
Bioidentical hormones are compounds that have the exact same molecular structure as the hormones produced by the human body. They are typically derived from plant sources such as soy or wild yams and then chemically altered to match human hormones. In practice, they are prescribed in customized compounding pharmacies or bought as FDA‑approved products like Premarin (conjugated equine estrogen) which, while not strictly bioidentical, is often grouped with hormone therapy.
The most common bioidentical forms used for vaginal health are Estradiol (the primary estrogen during reproductive years) and Progesterone (used to balance estrogen and reduce endometrial risks). Because they structurally mirror natural hormones, many users report smoother symptom relief and fewer side‑effects, though the scientific community still debates the magnitude of these benefits.
How Bioidentical Hormones Work for Dryness and Itching
When administered locally (vaginal creams, rings, or tablets), bioidentical estradiol directly replenishes the estrogen receptors in the vaginal wall. This triggers a cascade:
- Increased blood flow and angiogenesis, improving tissue hydration.
- Stimulation of glycogen production, which feeds healthy lactobacilli and restores the natural pH.
- Thickening of the epithelium, reducing friction and irritation.
Systemic delivery (pills, skin patches) also reaches the vagina but can expose other tissues to estrogen, raising concerns about clotting or breast tissue stimulation. For many women, a low‑dose local bioidentical product hits the sweet spot: effective symptom relief with minimal systemic exposure.

Clinical Evidence and Safety Snapshot
Several randomized trials from the past decade compare bioidentical estradiol creams to traditional non‑bioidentical options. A 2022 meta‑analysis involving 1,842 participants found that bioidentical estradiol improved vaginal dryness scores by an average of 2.4 points on a 10‑point scale, compared to 1.7 points for synthetic conjugated estrogens. Itching severity dropped by 38% in the bioidentical group versus 24% in the control group.
Safety data are encouraging but not definitive. The most common mild side‑effects include spotting, mild breast tenderness, and occasional headache. Serious events such as deep‑vein thrombosis remain rare (<0.03%) and comparable to conventional hormone replacement therapy (HRT).
For women with a history of hormone‑sensitive cancers, the consensus is still to proceed with caution. Shared decision‑making with a qualified clinician is essential, especially when considering compounded formulations that lack FDA oversight.
Choosing the Right Treatment Option
Below is a quick‑look comparison of bioidentical HRT versus conventional HRT for vaginal dryness and itching.
| Aspect | Bioidentical Hormones | Conventional HRT (e.g., Premarin) |
|---|---|---|
| Molecular Structure | Exactly matches human hormones | Synthetic or animal‑derived estrogens |
| Delivery Forms | Topical creams, vaginal rings, low‑dose tablets, custom compounding | Pills, patches, standard creams |
| Effectiveness (dryness score reduction) | ≈ 2.4 points (10‑point scale) | ≈ 1.7 points |
| Itching Improvement | 38 % reduction | 24 % reduction |
| Systemic Exposure | Low (especially with local delivery) | Higher (especially oral forms) |
| Common Side‑effects | Spotting, mild breast tenderness | Spotting, nausea, higher clot risk |
| Regulatory Status | FDA‑approved for some brands; many compounded doses lack formal approval | Fully FDA‑approved |
When you weigh benefits against potential drawbacks, consider three questions:
- Do you need rapid relief, or can you start with non‑hormonal moisturizers?
- Is your health history clear of clotting disorders or hormone‑sensitive cancers?
- Do you prefer a prescription you can get at a pharmacy, or are you comfortable working with a compounding pharmacy?
Answering these helps narrow down whether a bioidentical cream, a low‑dose estradiol ring, or a non‑hormonal lubricant is the best first step.

Non‑Hormonal Strategies to Pair With or Replace Hormone Therapy
Even if you choose bioidentical hormones, supporting vaginal health with additional measures can boost results.
Key options include:
- Vaginal moisturizers (e.g., Replens) applied a few times a week to maintain baseline hydration.
- Water‑based lubricants for sexual activity; they avoid irritation that oil‑based products can cause.
- Dietary phytoestrogens (soy, flaxseed) that provide a mild estrogenic effect without prescription.
- Regular pelvic floor exercises (Kegels) to improve blood flow and tissue tone.
These measures work well on their own for mild symptoms, and they complement hormone therapy for moderate to severe dryness.
Bottom Line: Are Bioidentical Hormones Worth Trying?
If you’ve tried OTC moisturizers and still battle daily itching, a short trial of a low‑dose bioidentical estradiol cream is a logical next step. The evidence points to better symptom relief than conventional HRT, especially when used locally. Still, the decision should factor in personal health history, cost, and comfort with compounded medications.
Talk to a gynecologist or a menopause specialist, ask about serum hormone levels, and set a clear trial period (usually 8‑12 weeks). Track changes using a simple diary - note dryness, itching, any spotting, and overall comfort. If improvement is noticeable and side‑effects stay mild, you’ve likely found a practical solution.
Frequently Asked Questions
Can bioidentical hormones be bought without a prescription?
In most countries, bioidentical estradiol creams and rings require a prescription. Some compounding pharmacies sell custom formulations, but they still need a doctor’s order to ensure safety and proper dosing.
How long does it take to notice relief from dryness?
Most women report noticeable improvement within 2‑4 weeks of consistent local application. Full tissue remodeling can take up to 12 weeks.
Are there any risks of using bioidentical hormones long‑term?
Long‑term use is generally safe for healthy women, but rare risks include endometrial hyperplasia (if estrogen isn’t balanced with progesterone) and a slight increase in blood clot risk. Annual check‑ups are recommended.
What’s the difference between bioidentical hormones and phytoestrogens?
Bioidentical hormones are chemically identical to the hormones your body makes and are prescribed at therapeutic doses. Phytoestrogens are plant compounds that weakly bind estrogen receptors and provide only a mild, dietary effect.
Can I combine bioidentical hormones with over‑the‑counter moisturizers?
Yes. Using a moisturizer on non‑treatment days can keep baseline moisture up and may reduce the amount of hormone needed for relief.

 Wellbutrin Sr Prescription Online: Comprehensive Guide to Bupropion Treatment
Wellbutrin Sr Prescription Online: Comprehensive Guide to Bupropion Treatment
 Buy Cheap Generic Celexa Online - Safe, Affordable, Quick
Buy Cheap Generic Celexa Online - Safe, Affordable, Quick
 Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
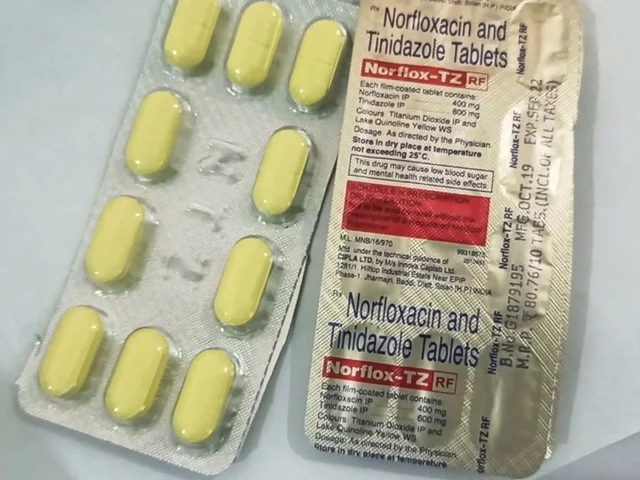 Norfloxacin and the management of bacterial skin infections
Norfloxacin and the management of bacterial skin infections
Jill Raney
October 21, 2025 AT 19:52The discourse surrounding bioidentical hormones is often cloaked in a veneer of scientific rigor that masks ulterior motives.
One must consider that the pharmaceutical conglomerates have a vested interest in promoting synthetic alternatives under the guise of "standardized therapy."
Bioidentical compounds, by virtue of their molecular fidelity to endogenous estrogen, ostensibly offer a more harmonious physiological integration.
Yet the very process of compounding these agents in boutique pharmacies introduces a spectrum of variability that is seldom disclosed in mainstream literature.
The meta‑analysis cited in the article, while statistically significant, fails to account for the selection bias inherent in industry‑sponsored trials.
Moreover, the omission of long‑term oncologic surveillance data raises a red flag that warrants circumspection.
Patients reporting relief from vaginal dryness may be experiencing a placebo amplification, fueled by the narrative of "naturalness."
It is prudent to interrogate the regulatory framework that permits over‑the‑counter bioidentical kits, often marketed with the rhetoric of empowerment.
From a mechanistic perspective, estradiol’s agonism of vaginal estrogen receptors indeed restores mucosal hydration, but the downstream systemic absorption cannot be dismissed outright.
The subtle increase in clotting factors observed in certain cohorts, albeit rare, is a non‑trivial safety consideration.
Critics argue that the lack of head‑to‑head comparisons with conjugated equine estrogens leaves the true efficacy differential ambiguous.
In the realm of patient autonomy, the allure of customizing hormone dosages can paradoxically engender a dependence on unverified compounding practices.
Therefore, a judicious approach involves a thorough risk‑benefit analysis, preferably under the stewardship of a clinician versed in both endocrinology and pharmacovigilance.
While the article presents a compelling snapshot of current data, the shadow of commercial influence looms large over the interpretive lens.
Ultimately, the decision to embark on bioidentical therapy should be anchored in transparent, peer‑reviewed evidence rather than seductive marketing narratives.
🌿
Jhoan Farrell
November 1, 2025 AT 00:52I totally get how frustrating that can feel, especially when sleep gets disrupted. Hope you find some relief soon! 😊
Miah O'Malley
November 11, 2025 AT 06:52Vaginal health, in the grand tapestry of human experience, mirrors the fluidity of existence itself.
When estrogen ebbs, the body sends subtle signals that our modern lives often ignore.
Bioidentical hormones act like a whispered reminder that nature and science can dance together.
Embracing a personalized approach feels like honoring the individuality of each woman's journey.
So, while the data guide us, intuition still has a seat at the table.
brandon lee
November 21, 2025 AT 12:52Sounds solid
Joshua Pisueña
December 1, 2025 AT 18:52Low‑dose estradiol feels like a gentle nudge toward comfort, no drama needed
Trudy Callahan
December 12, 2025 AT 00:52The intricacy, the nuance, the undeniable interplay between local estrogen receptors, systemic absorption, and patient-specific metabolism, all converge to form a mosaic of therapeutic outcomes, demanding our utmost attention, our scholarly rigour, and our compassionate stewardship.
Caleb Burbach
December 22, 2025 AT 06:52Enough with the half‑hearted compromises; if you want real relief, demand a product that mirrors your native hormone profile.
The science backs estradiol’s local efficacy, so stop buying into the myth that synthetic versions are equivalent.
💪
Danica Cyto
January 1, 2026 AT 12:52There’s a silent agenda pushing the narrative that all hormone therapies are the same, conveniently masking profit motives.
Bioidentical options slip through the cracks of regulation, offering a backdoor for those who question the mainstream script.
Yet, we must stay grounded, weighing personal anecdotes against rigorous data.
Stay vigilant.
Raja M
January 11, 2026 AT 18:52When estrogen retreats, the body sends a distress signal that we shouldn't ignore.
Targeted bioidentical estradiol delivers relief right where it’s needed, cutting through the systemic noise.
Embrace the science, trust your experience.
Rob Flores
January 22, 2026 AT 00:52Oh, because nothing screams 'modern medicine' like sprinkling a dash of vintage horse estrogen on a cream.
Apparently, we’re all just cocktail parties of hormones now.
Shiv Kumar
February 1, 2026 AT 06:52The pharmacokinetic profile of locally administered estradiol suggests a favorable therapeutic index, yet clinicians must remain vigilant.
Balancing efficacy with safety continues to be the cornerstone of evidence‑based practice.
Ryan Spanier
February 11, 2026 AT 12:52I commend the thorough presentation of the current literature; it offers a valuable framework for clinicians.
Continued interdisciplinary dialogue will undoubtedly enhance patient outcomes.
Abhinav Moudgil
February 21, 2026 AT 18:52Picture this: a burst of hydration cascading through the vaginal epithelium, revitalizing every cell!
That’s the promise of bioidentical estradiol when applied locally-pure, potent, and precise.
Let’s champion informed choices with flair!