When you're over 65 and taking blood pressure medication, standing up too fast can feel like walking on thin ice. One moment you're fine, the next you're seeing stars, your legs give out, and you're on the floor. This isn't just old age-it's orthostatic hypotension, a dangerous drop in blood pressure when standing. And it's more common than you think. About 1 in 5 older adults with high blood pressure experience it. The scary part? Many of the drugs meant to protect their hearts are making this worse.
What Is Orthostatic Hypotension-and Why Does It Matter?
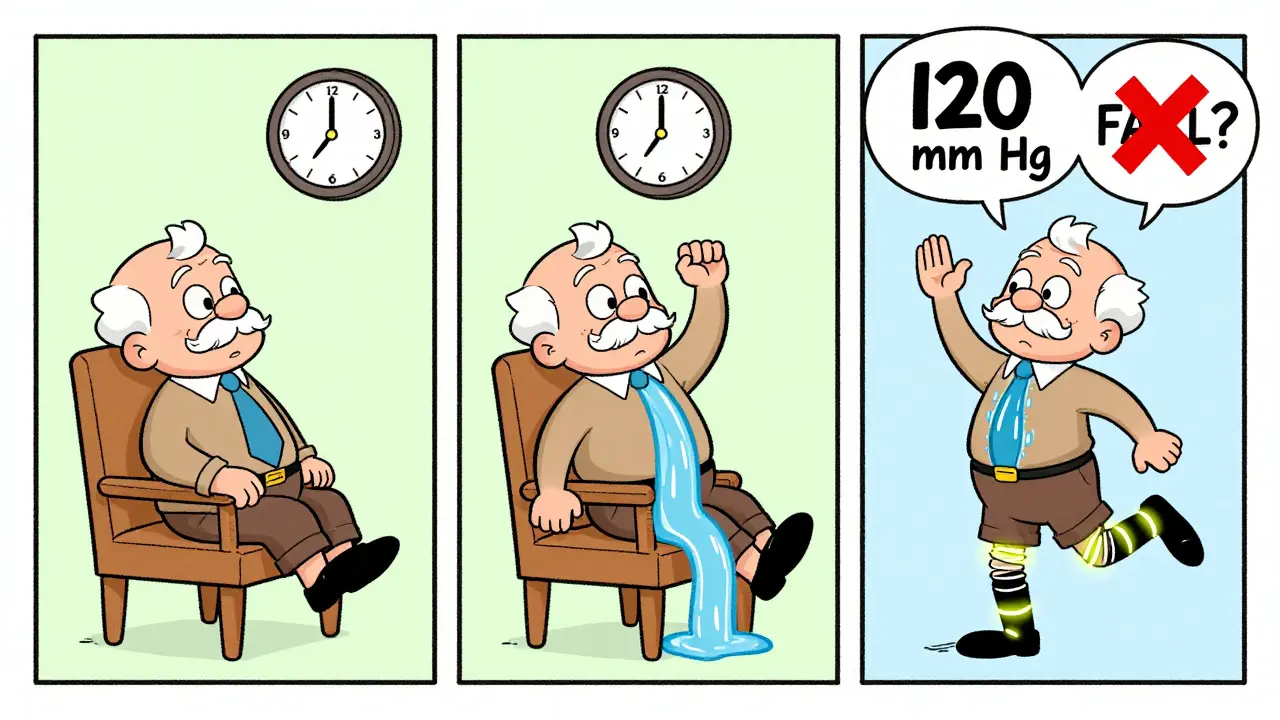
Orthostatic hypotension happens when your blood pressure drops at least 20 mm Hg systolic or 10 mm Hg diastolic within three minutes of standing. For younger people, the body quickly adjusts: blood vessels tighten, heart beats faster. But in older adults, that system slows down. Baroreceptors-your body’s pressure sensors-don’t respond as well. Blood pools in the legs. The brain gets less oxygen. Dizziness, blurred vision, nausea, and fainting follow. This isn’t just uncomfortable. It’s deadly. Falls are the leading cause of injury-related death in seniors. About 30% of older adults fall each year. Orthostatic hypotension contributes to nearly half of those falls. And when you break a hip after 70, your chances of surviving the next year drop sharply.Which Blood Pressure Medications Carry the Highest Risk?
Not all blood pressure drugs are created equal when it comes to orthostatic risk. Some are safer than others-and some should be avoided altogether in older adults.- Alpha blockers (like doxazosin, terazosin): These carry the highest risk. Up to 28% of older adults taking them develop orthostatic hypotension. They relax blood vessels too aggressively, especially when standing.
- Beta-blockers (like atenolol, metoprolol): These slow the heart and reduce its ability to compensate for blood pressure drops. Studies show they increase the risk of sustained low blood pressure by over three times.
- Diuretics (like furosemide, hydrochlorothiazide): They drain fluid, which lowers blood volume. Less volume means less pressure to push blood to the brain when standing.
- Central sympatholytics (like clonidine): These suppress the nervous system’s ability to raise blood pressure on demand.
On the flip side, some medications are surprisingly safe-or even protective.
- ACE inhibitors (like lisinopril) and ARBs (like losartan): These have the lowest risk. Studies show they reduce orthostatic hypotension by 14-15% compared to other classes. They work by relaxing arteries without overloading the system.
- Calcium channel blockers: Not all are equal. Amlodipine and lacidipine are well-tolerated because they dilate blood vessels slowly. Diltiazem and verapamil, however, can be riskier due to how the aging liver processes them.
- Isradipine: A lesser-known calcium blocker, it shows only a 5.2% incidence of orthostatic hypotension in older adults-the lowest of any class.
Here’s the twist: The more aggressively you treat high blood pressure, the less likely you are to get orthostatic hypotension. That’s right. The SPRINT trial and nine other major studies found that lowering systolic pressure to under 120 mm Hg didn’t increase falls or dizziness. In fact, it reduced orthostatic hypotension by 17% compared to standard targets of 140 mm Hg.
Why Less Is Sometimes More-And Why It’s Not Always True
Many doctors still think: “If they’re dizzy when they stand, we should lower the dose.” But that’s often the wrong move. Dr. Harry Goldblatt from Case Western Reserve University found something surprising: The real danger isn’t the drop when standing-it’s the high blood pressure when lying down. If you reduce meds to fix dizziness, you might leave the patient with uncontrolled nighttime hypertension. That raises stroke and heart attack risk. The American Heart Association says: Don’t stop or reduce blood pressure meds just because someone feels lightheaded when standing-unless they’re having symptoms like fainting or falls. Asymptomatic orthostatic hypotension doesn’t need treatment. Treating the symptom, not the cause, can do more harm.
What to Do Instead: A Practical Safety Plan
If you or a loved one is on blood pressure meds and feels dizzy on standing, here’s what actually works:- Review every medication. Ask your doctor: “Which of these could be causing this?” Cut out alpha blockers and certain beta-blockers first. Switch to ARBs or ACE inhibitors if possible.
- Change how you stand. Don’t jump out of bed. Sit on the edge for 30 seconds. Then stand slowly. Do this three times a day-morning, after meals, after using the bathroom. It trains your body to adapt.
- Stay hydrated. Dehydration worsens orthostatic hypotension. Drink 1.5-2 liters of water daily, unless you have heart failure. A glass of water before standing can help boost blood pressure.
- Wear compression stockings. These squeeze your legs and help push blood back up. They’re simple, cheap, and effective.
- Avoid alcohol and large meals. Both cause blood vessels to widen and blood pressure to drop.
- Time your meds. If you take a long-acting pill, take it at least three hours before bedtime. This reduces the chance of low pressure overnight and high pressure in the morning.
Most people see improvement within 2-4 weeks of making these changes. No drugs needed.
When Medication for Orthostatic Hypotension Itself Is Needed
Sometimes, lifestyle changes aren’t enough. If someone keeps falling, fainting, or can’t get out of bed without help, doctors may add a drug specifically for orthostatic hypotension.- Midodrine: A vasoconstrictor that tightens blood vessels. Works fast but can cause high blood pressure when lying down. Use with caution.
- Droxidopa: Turns into norepinephrine, which raises blood pressure. Used for neurogenic orthostatic hypotension, like in Parkinson’s.
- Fludrocortisone: A steroid that helps the body hold onto salt and water. Increases blood volume. Can cause swelling or high blood pressure if overused.
- Pyridostigmine: Helps nerves communicate better. Less effective but fewer side effects than others.
These are not first-line treatments. They’re last-resort options. And they’re expensive. Midodrine costs over $200 a month in the U.S. Most seniors don’t need them if their antihypertensive regimen is optimized first.
The Bigger Picture: Trends and What’s Coming
In 2023, ARBs and ACE inhibitors made up 38% of new prescriptions for seniors over 65-up from 32% in 2020. Why? Because doctors are finally learning: safety matters more than speed. The American Geriatrics Society’s 2023 Beers Criteria now lists alpha blockers and some beta-blockers as “potentially inappropriate” for older adults with orthostatic risk. Research is moving fast. Two new drugs in Phase II trials are designed to work only when you’re standing-not when you’re lying down. Imagine a pill that knows your posture. That’s the future. The bottom line? Treating high blood pressure in older adults isn’t about lowering numbers at all costs. It’s about balancing safety, function, and longevity. The goal isn’t just to live longer-it’s to live independently, without fear of falling.Frequently Asked Questions
Can blood pressure medication cause fainting in seniors?
Yes. Certain blood pressure medications-especially alpha blockers, beta-blockers, and diuretics-can cause a sudden drop in blood pressure when standing, leading to dizziness, lightheadedness, or fainting. This is called orthostatic hypotension. It’s not a normal part of aging, and it’s often preventable by switching to safer drugs like ACE inhibitors or ARBs.
Should I stop my blood pressure medicine if I feel dizzy when I stand?
Not without talking to your doctor. Stopping your meds can raise your risk of stroke or heart attack. Instead, ask your doctor to review your full list of medications. Often, the fix isn’t stopping the drug-it’s switching to a safer one. For example, replacing doxazosin with losartan can eliminate dizziness without losing blood pressure control.
Are ARBs better than ACE inhibitors for seniors with orthostatic hypotension?
Both are excellent choices. Studies show they have nearly identical low risks for orthostatic hypotension. ARBs (like losartan or valsartan) may cause fewer side effects like cough, which is common with ACE inhibitors. If your loved one has a cough on lisinopril, switching to an ARB often helps without losing protection.
How long does it take for orthostatic hypotension to improve after changing medications?
It usually takes 2 to 4 weeks. Blood pressure medications need time to fully leave the system, and your body needs time to adapt to new ones. Combine medication changes with slow position changes and hydration, and most seniors notice less dizziness within a month.
Can compression socks help with dizziness from blood pressure meds?
Yes. Compression stockings help prevent blood from pooling in the legs when standing. This keeps more blood flowing to the brain, reducing dizziness. They’re especially helpful when combined with other strategies like hydration and slow standing. Look for knee-high, 15-20 mmHg pressure socks-available without a prescription.
Is it safe to take blood pressure meds at night?
For most older adults, yes-and it’s often better. Taking long-acting blood pressure meds (like amlodipine or losartan) at least 3 hours before bedtime reduces the risk of morning spikes and nighttime lows. It also helps avoid the dangerous dip in pressure that can happen right after waking up, which is when most falls occur.
Next Steps for Seniors and Caregivers
If you’re managing blood pressure for an older adult:- Write down every medication, including over-the-counter pills and supplements.
- Ask the doctor: “Which of these could be causing dizziness when standing?”
- Request a standing blood pressure test: measure BP lying down, then again after standing for 1 minute and 3 minutes.
- Start slow standing practice-three times a day, for 30 seconds each.
- Keep a symptom journal: note when dizziness happens, what they were doing, and how long it lasted.
- Don’t rush. Fixing this takes weeks, not days. But the payoff-fewer falls, more independence-is worth it.
High blood pressure isn’t a problem to be crushed. It’s a condition to be managed wisely. For older adults, the safest treatment isn’t the strongest one-it’s the one that lets them stand up without fear.

 Blood Pressure Medication Safety in Older Adults: Managing Orthostatic Hypotension Risks
Blood Pressure Medication Safety in Older Adults: Managing Orthostatic Hypotension Risks
 2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
 Authorized Generics: Same Drug, Different Label
Authorized Generics: Same Drug, Different Label
 How Osteoarthritis and Osteoporosis Influence Each Other
How Osteoarthritis and Osteoporosis Influence Each Other
 Generic Drug Concerns: Myths vs. Reality for Safety and Efficacy
Generic Drug Concerns: Myths vs. Reality for Safety and Efficacy
Janette Martens
December 28, 2025 AT 11:51Marie-Pierre Gonzalez
December 30, 2025 AT 10:46Louis Paré
December 30, 2025 AT 13:52Ellen-Cathryn Nash
December 31, 2025 AT 18:12Samantha Hobbs
January 2, 2026 AT 05:24Nicole Beasley
January 4, 2026 AT 02:58sonam gupta
January 5, 2026 AT 19:53Debra Cagwin
January 6, 2026 AT 12:56Hakim Bachiri
January 7, 2026 AT 15:25Celia McTighe
January 7, 2026 AT 21:19