When you pick up a prescription, you might see a label that says generic instead of the name you recognize. It’s cheaper-often 80% less-but do you really get the same medicine? That’s the question swirling in the minds of millions. Some people swear their brand-name drug worked better. Others say the generic made them feel worse. And then there are the stories online: seizures after switching, thyroid levels going haywire, infections that won’t clear. Are these real risks-or just myths fed by fear and confusion?
What Exactly Is a Generic Drug?
A generic drug isn’t a copycat. It’s not a knockoff. It’s the exact same active ingredient, in the same strength, taken the same way-whether it’s a pill, injection, or inhaler-as the original brand-name version. The U.S. Food and Drug Administration (FDA) requires this. Every generic must deliver the same amount of active ingredient into your bloodstream at the same rate as the brand. That’s called bioequivalence. The FDA sets strict rules: the blood concentration of the generic must fall within 80% to 125% of the brand’s levels. That’s not a wide gap-it’s a tight window designed to ensure the same effect. The FDA doesn’t cut corners. Generic manufacturers must follow the same quality rules as brand-name makers. Their factories are inspected just as often. In 2022, 98.7% of generic facilities passed FDA inspections-slightly higher than the 97.3% pass rate for brand-name plants. The only real differences? The color, shape, flavor, or filler ingredients. These don’t affect how the drug works. But they can matter if you’re allergic to a dye or preservative. That’s why the label should list all ingredients. Too often, it doesn’t. Only 67% of generic labels fully list inactive ingredients, compared to 99% for brand-name drugs.Myth: Generics Are Less Effective
This is the biggest myth. If a drug works in the brand-name version, the generic must work the same. The FDA doesn’t approve generics based on guesswork. They require real studies-usually with 24 to 36 healthy volunteers. Blood samples are taken over hours to measure how much of the drug enters the system and how fast. The data must show the generic performs within the 80-125% range. If it doesn’t, it gets rejected. Real-world evidence backs this up. A 2020 study in Nature looked at 17 cardiovascular drugs. It found that patients on generics had fewer heart attacks, strokes, and deaths than those on brand-name versions. For drugs like metformin and gliclazide, the difference was clear: generics performed better. Another study of over 136,000 older adults on blood pressure meds found a spike in ER visits after switching to generics-but that wasn’t because the drugs were weaker. It was because patients were suddenly on a new pill, with a different shape, color, or brand name. Confusion led to missed doses, not drug failure.Myth: All Generics Are Identical
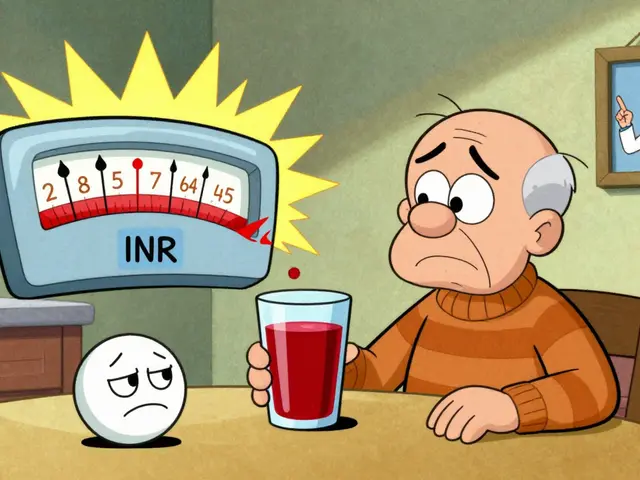
Not true. There are hundreds of generic versions of popular drugs like metformin, lisinopril, and sertraline. Each is made by a different company, sometimes in different countries. While the active ingredient is the same, the manufacturing process can vary. Particle size, crystal structure, or how the tablet breaks down in your stomach might differ slightly. For most drugs, this doesn’t matter. But for drugs with a narrow therapeutic index (NTID)-where the difference between a helpful dose and a dangerous one is tiny-those small changes can add up. Examples include warfarin (blood thinner), levothyroxine (thyroid hormone), and phenytoin (seizure control). The FDA treats these differently. For NTIDs, the acceptable bioequivalence range is tighter: 90-112%. Even then, some doctors recommend sticking with the same generic manufacturer once you’ve found one that works. Switching between different generic brands-even if both are FDA-approved-can cause instability in blood levels. That’s why the American Society of Health-System Pharmacists recommends avoiding multiple switches for NTID drugs.
Myth: Generics Are Made in Shady Factories
You’ve heard the rumors: generics are made in dirty labs in India or China. The truth? The FDA inspects all facilities-whether they make brand-name or generic drugs-using the same standards. As of 2023, over 78% of active pharmaceutical ingredients come from India and China. But that doesn’t mean they’re unsafe. The FDA has offices in both countries to monitor production. In 2022, 98.7% of generic manufacturing sites passed inspection. That’s better than the pass rate for many brand-name facilities. The real issue isn’t location-it’s transparency. The FDA doesn’t always tell you which company made your generic. If you have a bad reaction, you might never know if it was the generic, the batch, or something else. That’s why tracking your medication’s manufacturer matters. Keep the pill bottle. Note the name on the label. If you switch and feel off, go back to the previous version and ask your pharmacist to note it in your record.Myth: Generics Cause More Side Effects
Some people report new or worse side effects after switching. But is it the drug-or the change? Your body gets used to a specific pill shape, size, or even the taste. Switching to a new generic can trigger a psychological response. You expect to feel different, so you notice minor changes more. That’s the nocebo effect. But there are real cases where side effects changed. A 2022 study in Epilepsia found patients on generic levetiracetam had a 23% higher risk of seizure recurrence than those on the brand version, Keppra. That’s not common-but it’s documented. Another case: a patient’s urinary tract infection didn’t clear on generic ciprofloxacin but improved immediately after switching back to Ciproxin. These are rare, but they happen. The FDA tracks these reports. In 2023, they launched a database of 187 complex generics-drugs that are hard to copy, like inhalers, creams, or injectables-because they’re more likely to have these issues.When You Should Be Cautious
Not all drugs are created equal. Here’s when to pay extra attention:- Narrow therapeutic index drugs (warfarin, levothyroxine, lithium, phenytoin, cyclosporine): Stick with one manufacturer. Don’t switch unless your doctor approves.
- Complex formulations (extended-release pills, patches, inhalers): These are harder to replicate. Ask if your generic is on the FDA’s Complex Generic Drug Product Database.
- Psychiatric medications (SSRIs like sertraline, escitalopram): Some studies show slightly higher hospitalization rates with generics. If you’re stable on brand, talk to your doctor before switching.
- Medications for chronic conditions (diabetes, high blood pressure): Adherence drops by 5.3% in the first 90 days after switching to generic. Make sure you’re still taking it regularly.
What the Data Really Says
Let’s cut through the noise. Here’s what the science says about generics:- 90.2% of U.S. prescriptions are filled with generics.
- They account for only 19.3% of total drug spending.
- Between 2010 and 2020, generics saved the U.S. healthcare system $2.29 trillion.
- 99.8% of approved generics meet or exceed bioequivalence standards.
- For 99% of drugs, generics are just as safe and effective.
What You Can Do
You don’t have to guess. Here’s how to protect yourself:- Ask your pharmacist: “Is this the same manufacturer as last time?”
- Check the label. Write down the manufacturer name and lot number.
- Don’t switch generics without talking to your doctor-especially for NTID drugs.
- If you feel different after switching, don’t assume it’s all in your head. Track symptoms. Take your blood pressure, check your TSH levels, note seizure frequency.
- Report side effects to the FDA’s MedWatch program. Your report helps others.
Bottom Line
For most people, generics are safe, effective, and the smart choice. They’re not cheaper because they’re worse. They’re cheaper because the brand-name company spent millions on research and marketing-and now, after the patent expires, others can make the same drug without those costs. But for a small group-those on thyroid meds, blood thinners, seizure drugs, or complex treatments-switching can be risky. That’s not a myth. That’s science. And it’s why knowing your drug, your dose, and your manufacturer matters more than ever.If your doctor says a generic is fine, trust them. But if you’ve had a bad experience-or you’re on a drug where small changes matter-speak up. Your health isn’t a cost-saving metric. It’s personal. And you deserve to know exactly what’s in your pill.
Are generic drugs as safe as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of drug into your bloodstream at the same rate. Manufacturing standards are identical. In 2022, 98.7% of generic facilities passed FDA inspections, slightly higher than brand-name facilities. The only differences are inactive ingredients, which rarely cause issues unless you have an allergy.
Why do some people feel worse on generic drugs?
Sometimes, it’s not the drug-it’s the change. Switching from a familiar pill shape, color, or brand name can trigger psychological effects, making people believe they feel different. Other times, it’s a real issue: for drugs with a narrow therapeutic index-like levothyroxine or warfarin-tiny differences in how the drug dissolves can affect blood levels. A 2022 study found generic levetiracetam had a 23% higher seizure recurrence rate than the brand. If you notice changes after switching, track symptoms and talk to your doctor.
Can I switch between different generic brands?
For most drugs, yes. But for drugs with a narrow therapeutic index-like thyroid meds, blood thinners, or seizure drugs-it’s risky. Even if two generics are FDA-approved, they may be made by different companies with slightly different manufacturing processes. That can cause fluctuations in your blood levels. Experts recommend sticking with the same manufacturer once you find one that works. If your pharmacy switches your generic without telling you, ask them to note your preference.
Are generic drugs made in unsafe countries?
No. Over 78% of active ingredients come from India and China, but the FDA inspects all manufacturing sites-domestic and foreign-using the same strict standards. In 2022, 98.7% of generic facilities passed inspection. The FDA has inspectors stationed in both countries. The real issue isn’t location-it’s transparency. Generic labels often don’t list all inactive ingredients, making it harder to trace reactions. Always keep your pill bottle and note the manufacturer name.
Do generics cost less because they’re lower quality?
No. Generics cost less because the original company already paid for research, clinical trials, and marketing. Once the patent expires, other companies can make the same drug without those upfront costs. The active ingredient is identical. The manufacturing standards are identical. The FDA doesn’t allow lower quality. The savings come from competition, not compromise. Generics saved the U.S. healthcare system over $2 trillion between 2010 and 2020.
How do I know if my generic drug is working?
Monitor your condition. If you’re on blood pressure medication, check your readings. If you’re on thyroid hormone, get your TSH levels tested. If you have epilepsy, track seizure frequency. If you’re on an antidepressant, note your mood and sleep patterns. If you notice changes after switching to a generic, don’t ignore them. Talk to your doctor. Keep the original pill bottle. Write down the manufacturer name. These details help your doctor determine if the issue is the drug-or something else.
 Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
 How to Compare Manufacturer Expiration Dates vs. Pharmacy Beyond-Use Dates for Medications
How to Compare Manufacturer Expiration Dates vs. Pharmacy Beyond-Use Dates for Medications
 Understanding the Link Between Increased Thirst and Frequent Headaches
Understanding the Link Between Increased Thirst and Frequent Headaches
 Generic Drug Prices: Why Americans Pay Less Than Europeans
Generic Drug Prices: Why Americans Pay Less Than Europeans
 Thyroid Medications: Levothyroxine Safety and Monitoring
Thyroid Medications: Levothyroxine Safety and Monitoring
Daniel McKnight
November 25, 2025 AT 16:34I’ve been on generic levothyroxine for five years-same bottle, same pharmacy. Last month they switched me to a different maker without telling me. My TSH went from 2.1 to 6.8 in six weeks. I didn’t even realize it was the pill until I dug up the old bottle. Now I keep the packaging like it’s a birth certificate. If your doctor says ‘it’s all the same,’ ask them if they’d swap their insulin for a mystery brand. I didn’t think I’d be the type to care about pill color… until my body started screaming.
Jaylen Baker
November 27, 2025 AT 11:29Generics saved my life. I’m on disability. Without them, I couldn’t afford my blood pressure meds, my antidepressants, or my diabetes pills. I’ve switched generics five times-never had a problem. The people who say they ‘feel different’? They’re not sick-they’re anxious. Your mind can make you feel worse than any inactive ingredient ever could. Stop overthinking your pills. Trust the science. The FDA doesn’t lie. And neither do the stats: 99.8% of generics are perfect. Stop being paranoid. Your health depends on you taking the damn thing-not staring at it.
Fiona Hoxhaj
November 27, 2025 AT 11:52One must, with the gravitas of a physician-scholar, confront the epistemological fallacy that equates bioequivalence with therapeutic equivalence. The FDA’s 80–125% window is not a scientific triumph-it is a regulatory compromise, a neoliberal concession to corporate efficiency masquerading as public health. To assert that a drug is ‘the same’ because its active ingredient matches is to confuse chemical identity with physiological resonance. The crystal lattice, the dissolution profile, the excipient synergy-these are not trivialities; they are the silent symphonies of pharmacokinetics. To reduce human biology to a spreadsheet of concentration curves is to misunderstand the very essence of healing. I, for one, refuse to be a statistical footnote in a cost-cutting experiment.
Merlin Maria
November 28, 2025 AT 20:13Fiona’s post is technically correct but emotionally detached. The real issue isn’t the FDA’s standards-it’s the lack of transparency. Pharmacies rotate generics without consent. Patients don’t know what they’re getting. That’s not a flaw in the system-it’s a failure of communication. And yes, for NTID drugs, switching manufacturers is like playing Russian roulette with your thyroid. But here’s the kicker: most doctors don’t know this either. They’re trained to prescribe, not to track pill batches. So if you’re on warfarin or levothyroxine, don’t wait for your doctor to catch up. Be your own pharmacist. Write down the manufacturer. Take a photo of the bottle. Report every weird symptom. If you don’t advocate for yourself, no one will. The system doesn’t care. You do.
Nagamani Thaviti
November 29, 2025 AT 15:47