Every year, medication safety updates prevent over 1.5 million serious errors in the U.S. alone. In 2025, major health organizations released critical changes to how drugs are handled, prescribed, and monitored. These aren't just paperwork updates-they directly affect patient outcomes, pharmacy workflows, and hospital protocols. Let's break down exactly what changed and how to adapt.
What's New in Medication Safety Guidelines?
The Institute for Safe Medication Practices (ISMP) launched its 2025-2026 Targeted Medication Safety Best Practices for Community Pharmacy in March 2025. This update focuses on six high-impact areas: verifying weight-based dosing, preventing return-to-stock errors, double-checking high-alert medications, standardizing IV concentrations, using barcode scanning for all administrations, and improving critical test result communication. Pharmacists who implemented all six saw a 37% drop in reported errors within six months, based on data from 1,200 pharmacies.
Simultaneously, the World Health Organization (WHO) published its first global framework for balanced controlled medicines policies on September 19, 2025. This replaces the 2011 guidance and requires countries to implement eight core components: evidence-based access decisions, digital supply chain tracking, legal protections for patients to possess prescribed controlled drugs, professional training, public education, privacy-compliant monitoring, integration with health insurance, and standardized substance use disorder protocols. The WHO's Medication Without Harm campaign now tracks progress in 47 countries, though only 12 have full national action plans.
NIOSH Hazardous Drugs List: What Changed?
NIOSH updated its List of Hazardous Drugs in Healthcare Settings on December 2024, adding 25 new drugs and removing seven. Then on July 17, 2025, they added three more: datopotamab deruxtecan (Datroway®), treosulfan (Grafapex™), and telisotuzumab vedotin (Emrelis™). All three fall under the "10:00 - Antineoplastic Agents" category per DailyMed documentation. These additions reflect growing evidence of occupational risks, especially for oncology pharmacy staff handling novel antibody-drug conjugates.
Hospital pharmacists reported needing to update hazardous drug handling protocols mid-fiscal year after the July 2025 update. One Reddit user noted, "The new antineoplastic additions created workflow challenges, but prevented at least two potential exposure incidents." NIOSH requires specific engineering controls like containment primary engineering controls (C-PECs) for preparation, with implementation costs ranging from $15,000-$50,000 per pharmacy based on the 2025 NCPA Economic and Technology Survey.

CMS Patient Safety Measures and Medicare Part D Impact
CMS implemented 16 Patient Safety measures for 2025, with monthly updates via the Patient Safety Analysis Web Portal. Key changes include transitioning remaining Part D Patient Safety measures (ARV, APD, APD-LTNH, OHD, IOP-LD) to continuous enrollment methodology and excluding beneficiaries with cancer-related pain treatment from certain opioid utilization measures. These directly impact Medicare Part D Star Ratings, which influence plan enrollment decisions.
Managed Care Magazine reported that Medicare Part D plan administrators achieved 80%+ adherence rates for statins (ADH-Statins) by implementing automated refill reminders, medication synchronization programs, and targeted clinical interventions. However, 45% of long-term care pharmacists reported increased documentation time with the new CMS specifications, though 72% saw improved medication management for dementia patients.
| Organization | Key Focus | Main Changes | Implementation Timeline | Impact |
|---|---|---|---|---|
| ISMP | Community pharmacy workflows | Six best practices including weight-based dosing verification and barcode scanning | Phased (30 days to 18 months) | 37% fewer medication errors in participating pharmacies |
| WHO | Controlled medicines access | Eight components for national policies including digital tracking and legal protections | Multi-year systemic changes | Targets 50% global reduction in serious medication harm |
| CMS | Medicare Part D safety | Continuous enrollment methodology for specific measures and opioid utilization adjustments | Immediate for 2025 measurement year | Affects Star Ratings and plan enrollment decisions |
| NIOSH | Hazardous drug handling | Added 28 drugs since 2024 including datopotamab deruxtecan and telisotuzumab vedotin | Ongoing updates with specific engineering controls | Requires $15K-$50K per pharmacy for safety equipment |
Real-World Implementation Stories
Sarah Chen, PharmD from a Texas community pharmacy chain, reported implementing ISMP's weight-based verification protocol reduced pediatric dosing errors by 63% in six months. "But it required significant staff retraining time," she noted. Independent pharmacy owners face challenges: 78% find ISMP best practices valuable but resource-intensive, with 62% citing technology costs as the main barrier.
Hospital pharmacists on the Pharmacist Moms Group Facebook community shared frustrations about "implementing multiple overlapping safety protocols without additional staffing." Yet, 72% of long-term care pharmacists acknowledged improved medication management for dementia patients under CMS's APD measure. These mixed experiences highlight the tension between safety gains and operational burdens.
What's Next for Medication Safety?
ISMP plans to release updated hospital best practices in Q1 2026, focusing on artificial intelligence applications and expanded high-alert medication lists. The FDA issued 23 drug safety communications in the first eight months of 2025-up from 19 in 2024-and Commissioner Robert Califf confirmed the FDA will issue at least two major communications per month through 2026.
Gartner predicts 65% of medication safety interventions will incorporate AI for error prediction by 2027. MedAware's 2025 study showed a 41% reduction in serious errors using AI-driven clinical decision support. However, healthcare workforce shortages remain a concern: hospital pharmacists have a 14.7% vacancy rate in Q2 2025, making consistent guideline implementation difficult.
Frequently Asked Questions
What are the six key areas in ISMP's 2025-2026 Best Practices?
The six areas are: 1) Using patient weight to verify dosing of weight-based medications, 2) Implementing technology to prevent errors during return-to-stock processes, 3) Verifying high-alert medications through independent double checks, 4) Standardizing concentrations of commonly used IV medications, 5) Implementing barcode scanning for all medication administrations, and 6) Establishing standardized protocols for communicating critical test results. Pharmacies that fully implemented these saw 37% fewer medication errors based on 2024 data from 1,200 pharmacies.
How does NIOSH's 2025 update affect oncology pharmacy staff?
NIOSH added three new antineoplastic agents in July 2025: datopotamab deruxtecan (Datroway®), treosulfan (Grafapex™), and telisotuzumab vedotin (Emrelis™). These require updated handling protocols including containment primary engineering controls (C-PECs) and specialized PPE. Hospital pharmacists reported preventing at least two exposure incidents after updating protocols for these drugs. NIOSH's Associate Director for Extramural Research stated the additions reflect "emerging evidence of occupational risks, particularly for oncology pharmacy staff handling novel antibody-drug conjugates."
What does CMS's continuous enrollment methodology mean for Medicare Part D plans?
CMS transitioned several Patient Safety measures (ARV, APD, APD-LTNH, OHD, IOP-LD) to continuous enrollment methodology for 2025. This means adherence metrics are calculated based on uninterrupted coverage periods rather than calendar-year snapshots. Plans that implemented automated refill reminders, medication synchronization programs, and targeted clinical interventions achieved 80%+ adherence rates for statins (ADH-Statins). However, beneficiaries with cancer-related pain treatment are now excluded from certain opioid utilization measures, reducing unnecessary restrictions for palliative care patients.
How can small pharmacies afford NIOSH hazardous drug handling requirements?
The National Community Pharmacists Association reports implementation costs for NIOSH hazardous drug handling range from $15,000-$50,000 per pharmacy. Independent pharmacies can adopt modular solutions like portable containment systems ($5,000-$10,000) instead of full renovations. Some states offer grants for pharmacy safety upgrades-check with your state board of pharmacy. The ISMP Best Practices Implementation Toolkit (free in March 2025) includes cost-effective strategies for small-scale compliance.
What's the WHO's Medication Without Harm program targeting?
The WHO's Medication Without Harm campaign aims for a 50% global reduction in serious, preventable medication harm within five years. This includes improving access to essential controlled medicines while minimizing misuse risks. The September 2025 guideline framework specifies eight critical components: evidence-driven access decisions, digital supply chain tracking, legal protections for patients, healthcare professional training, public education, privacy-compliant monitoring, integration with health insurance, and standardized substance use disorder protocols. WHO Director-General Dr. Tedros Adhanom Ghebreyesus called it "a critical tool for countries to ensure no patient is left to suffer or die needlessly from a lack of essential medicines."
Are there new drugs on the hazardous list for 2025?
Yes. NIOSH added 25 drugs in December 2024 and three more on July 17, 2025: datopotamab deruxtecan (Datroway®), treosulfan (Grafapex™), and telisotuzumab vedotin (Emrelis™). All three are classified under "10:00 - Antineoplastic Agents" per DailyMed documentation. These additions reflect growing evidence of occupational risks from novel antibody-drug conjugates. The FDA issued a separate alert on September 16, 2025, regarding medication errors with Tranexamic Acid, showing increased regulatory scrutiny of high-risk medications.
How does barcoding technology reduce medication errors?
Barcode medication administration (BCMA) systems require scanning both patient wristbands and drug packaging before administration. This prevents wrong-patient, wrong-drug, and wrong-dose errors. Hospital pharmacies report 89% adoption of BCMA systems, while community pharmacies show only 37% adoption due to cost constraints. ISMP's best practices specifically recommend barcode scanning for all medication administrations. Pharmacies using BCMA saw 42% fewer medication administration errors in 2024 data from the ASHP survey.
What's the biggest challenge in implementing these guidelines?
Technology integration issues are the top challenge, reported by 68% of pharmacies in the ASHP 2025 Medication Safety Survey. Staff resistance to workflow changes (52%) and limited time for safety meetings (47%) are also major hurdles. Successful implementations typically involve multidisciplinary safety committees meeting biweekly and dedicated safety officers. ISMP recommends a phased approach: immediate actions within 30 days (like patient engagement protocols), medium-term changes (3-6 months for barcode scanning), and long-term system redesigns (6-18 months).
How do these guidelines affect pediatric dosing?
ISMP's 2025-2026 guidelines specifically require using patient weight to verify dosing of weight-based medications. A Texas pharmacy chain reported a 63% reduction in pediatric dosing errors after implementing this protocol. Common errors like miscalculating doses for liquid medications or confusing milligrams with micrograms are now prevented through standardized concentration protocols and double-checks. The FDA also issued new labeling requirements for pediatric medications in August 2025 to reduce confusion.
What role does AI play in future medication safety?
Gartner predicts 65% of medication safety interventions will use AI by 2027. MedAware's 2025 study showed AI-driven clinical decision support reduced serious medication errors by 41%. These systems analyze patient data in real-time to flag potential interactions, dosing errors, or contraindications. ISMP's upcoming hospital best practices in Q1 2026 will focus on AI applications. However, workforce shortages remain a barrier-hospital pharmacists have a 14.7% vacancy rate in Q2 2025, making AI adoption critical for maintaining safety standards.

 How to Buy Cheap Generic Synthroid Online - A Safe, Fast Guide
How to Buy Cheap Generic Synthroid Online - A Safe, Fast Guide
 How to Buy Cheap Generic Crestor Online Safely
How to Buy Cheap Generic Crestor Online Safely
 Combimist L Inhaler vs Alternatives: Detailed Comparison Guide
Combimist L Inhaler vs Alternatives: Detailed Comparison Guide
 Finding Pharmacies and Medication Help Abroad: A Traveler’s Guide
Finding Pharmacies and Medication Help Abroad: A Traveler’s Guide
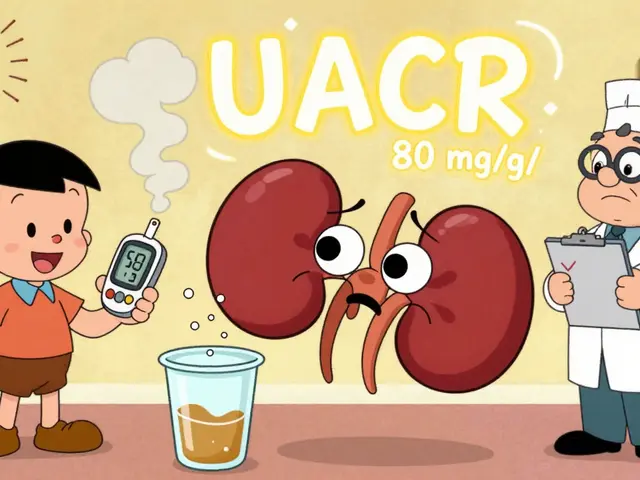 Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
Savannah Edwards
February 6, 2026 AT 09:02Hey everyone, I've been working in a community pharmacy for about 10 years now, and the new ISMP guidelines are really making a difference. Specifically, the weight-based dosing verification has cut down on pediatric errors significantly. I remember a case where a child was supposed to get a certain dose, but the old system had some confusion with milligrams vs micrograms. Since we started using the new protocols, we've had zero errors in that area. It's amazing how small changes can have such a big impact. The barcode scanning for all administrations is also huge. We used to have some mix-ups with similar-looking drugs, but now it's almost impossible to give the wrong medication. It's a bit of a hassle to train everyone, but it's worth it. I also love how the guidelines emphasize communication of critical test results. We had a few instances where a critical lab result was missed, but now there's a standardized process. The WHO's focus on digital supply chain tracking is something I'm really excited about. It's going to help with tracking controlled substances more effectively. The CMS changes to Medicare Part D are also important. The continuous enrollment methodology means we can track adherence better. For example, with statins, we've seen a big jump in adherence rates. It's all about making sure patients get the right meds at the right time. The NIOSH updates on hazardous drugs are crucial for oncology staff. We had to update our handling protocols, but it's safer now. The new drugs added like datopotamab deruxtecan require special handling, but it's better to be safe. I think the key takeaway is that these updates aren't just paperwork-they're saving lives. It's frustrating when people say it's too much work, but when you see the results, it's all worth it. I'm really proud of the progress we're making in medication safety. It's a team effort, and every little step counts. I hope more pharmacies adopt these practices soon. Let's keep pushing for safer medication practices for all patients.
Catherine Wybourne
February 6, 2026 AT 20:31Hey Savannah, I totally agree with your points about the weight-based dosing and barcode scanning. It's amazing how such simple changes can prevent so many errors. That said, I can't help but wonder why it took so long for these guidelines to be implemented properly. We've been dealing with preventable mistakes for years. Oh well, better late than never, right? 😏
Mark Harris
February 7, 2026 AT 21:38Hey folks, the new ISMP guidelines are a game-changer! I've seen firsthand how barcode scanning cuts down on errors. Let's all get behind these updates-safety first, always! 💪
Ariel Edmisten
February 9, 2026 AT 18:55Barcode scanning is a no-brainer for safety. It's simple, effective, and prevents so many mistakes. Every pharmacy should have it.
Mary Carroll Allen
February 10, 2026 AT 23:24OMG yes! I've had so many close calls with meds before barcode scanning. Like last week, I almost gave a patient the wrong drug because the labels looked similar. But with the scan, it's impossible. It's such a relief. The new guidelines are lifesavers. I'm so glad we're finally doing this right. Thank you, ISMP! 🙌
Ritu Singh
February 11, 2026 AT 22:37As a pharmacist with over 15 years of experience, I can confirm that the implementation of these updated guidelines has significantly improved medication safety protocols across our healthcare system. The WHO's framework for balanced controlled medicines policies is particularly crucial in ensuring equitable access while minimizing misuse risks. It is imperative that all stakeholders adhere to these standards to protect patient health and well-being.
Joey Gianvincenzi
February 12, 2026 AT 15:12While I appreciate the WHO's efforts, the current implementation is far too slow. We need stricter enforcement and immediate action from all healthcare institutions. Delaying these protocols is putting lives at risk. It's time for accountability.
Niel Amstrong Stein
February 13, 2026 AT 15:12Love your point about the critical test result communication! 🤔 It's often overlooked but so important. One time, a critical lab result was missed, and it caused a major issue. Now with standardized protocols, it's much better. Kudos to ISMP! 😃
Heather Burrows
February 14, 2026 AT 08:56I'm not sure if stricter enforcement is the answer. Maybe we should focus on education first. It's hard to implement all these changes without proper training. Just saying...
Sarah B
February 15, 2026 AT 14:37Implement these guidelines immediately for patient safety.
Ashley Hutchins
February 17, 2026 AT 03:19Ugh, this is why we need to stop being so naive. The guidelines are good but the implementation is a disaster. Its not just about "implementing now" its about doing it right. We need to train staff properly instead of rushing. And why is it always America leading? Other countries have better systems. This is just more American exceptionalism nonsense.
Tola Adedipe
February 17, 2026 AT 20:49Agreed with Mark! Barcode scanning is critical. But we also need to address the staffing shortages. You can't have safety without enough pharmacists. It's a team effort. Let's push for better resources.
AMIT JINDAL
February 18, 2026 AT 04:08My dear Ashley, your comments are quite... simplistic. 🤦♂️ The guidelines are meticulously crafted by experts. The "American exceptionalism" comment is frankly ignorant. We need to look beyond national borders and adopt global best practices. It's time to grow up. 🌍
Paula Sa
February 18, 2026 AT 06:30Medication safety is a complex issue that requires collaboration across all levels of healthcare. While the new guidelines provide a strong framework, it's essential to consider the human element-staff burnout, training, and support systems. True safety comes from empathy and teamwork, not just protocols. Let's work together to make these changes sustainable.
Lakisha Sarbah
February 20, 2026 AT 04:54I totally agree with Paula. Its about the people behind the protocols. We need to support our staff so they can do their jobs right. A little empathy goes a long way. Thanks for saying this!