Stopping benzodiazepines cold turkey can be dangerous. For people who’ve taken them daily for months or years, sudden withdrawal can trigger seizures, hallucinations, or even life-threatening complications. Yet many patients stay on these medications far longer than they should-often because they don’t know how to quit safely. The good news? With the right plan, most people can reduce and stop benzodiazepines without serious harm. The key is benzodiazepine tapering: a slow, controlled reduction guided by evidence and personalized to your body and history.
Why Tapering Matters
Benzodiazepines like Xanax, Valium, and Klonopin work fast. They calm anxiety, help you sleep, and stop seizures. But after just four to six weeks of daily use, your brain starts adapting. It reduces its own natural calming chemicals, like GABA, and becomes dependent on the drug to function normally. When you stop suddenly, your nervous system goes into overdrive. That’s when symptoms like panic attacks, tremors, insomnia, and tingling skin show up. The Joint Clinical Practice Guideline on Benzodiazepine Tapering (2024), backed by 10 major medical societies, confirms that abrupt discontinuation carries a 20-40% risk of severe withdrawal-especially with short-acting drugs like alprazolam. That’s why tapering isn’t optional. It’s the standard of care.How Slow Should You Go?
There’s no single answer, but most experts agree on a starting point: reduce your total daily dose by 5-10% every 2 to 4 weeks. This pace gives your brain time to readjust without triggering intense symptoms. The Oregon Health Authority breaks it down by duration of use:- 2-8 weeks of use: taper over at least 2 weeks
- 8 weeks to 6 months: taper over at least 4 weeks
- 6 months to 1 year: taper over at least 8 weeks
- More than 1 year: taper over 6 to 18 months
Choosing the Right Medication for Tapering
Not all benzodiazepines are made the same. Short-acting ones like alprazolam (Xanax) and triazolam (Halcion) leave your system fast. That means withdrawal symptoms hit harder and sooner. Longer-acting ones like diazepam (Valium) stay in your body longer, smoothing out the drop. That’s why many doctors switch patients from short-acting to long-acting benzos before tapering. For example:- 1 mg of alprazolam = 20 mg of diazepam
- 0.5 mg of lorazepam (Ativan) = 10 mg of diazepam

What If You Can’t Taper Alone?
Tapering isn’t just about pills. It’s about support. Studies show that when patients get cognitive behavioral therapy (CBT) along with medical tapering, success rates jump from 42% to nearly 68%. CBT helps you replace the drug with healthier coping tools-breathing techniques, sleep hygiene, mindfulness, and managing triggers. The VA recommends team-based care: a prescriber, a clinical pharmacist, and even a peer support specialist-someone who’s been through it themselves. These people help you track symptoms, adjust your plan, and stay motivated. You should also use one pharmacy and one prescriber to avoid accidental double-dosing or diversion. Some clinics limit prescriptions to once every 1-2 weeks, so you can’t stockpile. Regular check-ins-every 2-4 weeks-are non-negotiable.Who Should Taper?
The guidelines are clear: tapering should be considered for most long-term users-especially if you’re over 65. Benzodiazepines increase fall risk, confusion, and car accidents in older adults. The Beers Criteria lists them as potentially inappropriate for seniors. Other high-priority groups:- People with a history of substance use disorder
- Those taking multiple benzodiazepines or combining them with opioids or stimulants
- Patients with PTSD or chronic pain (benzos reduce the effectiveness of trauma therapy)
- Anyone with cognitive decline or traumatic brain injury
Common Mistakes and How to Avoid Them
Many people fail at tapering not because they’re weak, but because they make predictable errors:- Skipping doses: This causes unstable blood levels and spikes in withdrawal. Always reduce by percentage, not by skipping.
- Using alcohol or other sedatives: This masks symptoms but increases overdose risk and delays recovery.
- Expecting perfection: Some days will be harder. Anxiety might flare. Sleep might vanish. That’s normal. Don’t see it as failure-it’s part of the process.
- Going too fast: If you’re losing sleep, feeling shaky, or having panic attacks, you’re moving too quickly. Slow down. Stay where you are until you feel steady.

What to Expect During Tapering
Withdrawal symptoms vary. You might experience:- Increased anxiety or panic
- Insomnia or vivid dreams
- Tremors, muscle aches, or tingling
- Sensory sensitivity (light, sound, touch)
- Brain zaps (brief electric-shock feelings)
- Depersonalization or dizziness
The Future of Tapering
New tools are emerging. The NIH is testing a mobile app that tracks symptoms in real time and suggests dose adjustments based on your input. Early results show it improves adherence and reduces panic around tapering. Regulatory pressure is also growing. In 28 U.S. states, doctors must create a formal tapering plan if they prescribe benzodiazepines for more than 90 days. The FDA now requires warning labels on all prescriptions about the risks of sudden discontinuation. In the VA system, long-term benzodiazepine use dropped 23.7% between 2020 and 2023 thanks to mandatory tapering protocols. That’s over 100,000 veterans who’ve reduced or stopped these drugs safely.Final Thoughts
Benzodiazepine tapering isn’t easy. But it’s doable. It’s not about willpower-it’s about science, patience, and support. Whether you’ve been on benzos for six months or six years, there’s a path forward. Start with your doctor. Ask about switching to diazepam. Ask about therapy. Ask for a written plan. And remember: progress isn’t linear. Some weeks you’ll feel stronger. Others, you’ll need to pause. That’s okay. The goal isn’t to rush off the medication. It’s to reclaim your nervous system-on your terms.Can I taper off benzodiazepines on my own?
While some people manage mild tapers independently, it’s strongly recommended to work with a doctor. Withdrawal can be unpredictable, especially with long-term or high-dose use. A prescriber can help you choose the right medication, adjust your pace, and catch early signs of complications. If you’re on multiple medications, have a history of seizures, or are over 65, professional supervision is essential.
How long does benzo withdrawal last?
Acute withdrawal symptoms usually last 1-4 weeks after each dose reduction. For long-term users, symptoms can linger for months, but they typically become milder over time. Protracted withdrawal-lasting more than 6 months-is rare but possible. Most people see significant improvement within 3-6 months after completing their taper. Consistent sleep, stress management, and avoiding alcohol help speed recovery.
Is diazepam safer than other benzos for tapering?
Yes. Diazepam has a long half-life and active metabolites that provide a smoother decline in blood levels. This reduces the intensity of withdrawal symptoms compared to short-acting drugs like alprazolam or lorazepam. It’s also available in low-dose tablets, making precise reductions easier. Switching from a short-acting benzo to diazepam before tapering is a standard clinical practice recommended by the 2024 Joint Guideline.
What if I relapse and go back to my old dose?
Relapse doesn’t mean failure. It means your taper was too fast-or you needed more support. Many people need to try multiple times. The key is to pause, reflect, and restart slower. Don’t rush back to your highest dose. Stay at your last stable level for at least 2-4 weeks before trying again. Talk to your doctor about adding therapy or adjusting your taper plan. Most people eventually succeed with persistence.
Are there alternatives to benzodiazepines for anxiety or insomnia?
Yes. For anxiety, SSRIs like sertraline or escitalopram are first-line and safe for long-term use. For insomnia, cognitive behavioral therapy for insomnia (CBT-I) is more effective than any sleep medication over time. Other options include melatonin (for circadian rhythm issues), hydroxyzine (a non-addictive antihistamine), or low-dose trazodone. None of these carry the same dependence risk as benzodiazepines. The goal is to replace the drug with sustainable, non-pharmacological tools.

 FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
 How Clavulanic Acid Revolutionizes Antibiotic Treatments for Resistant Infections
How Clavulanic Acid Revolutionizes Antibiotic Treatments for Resistant Infections
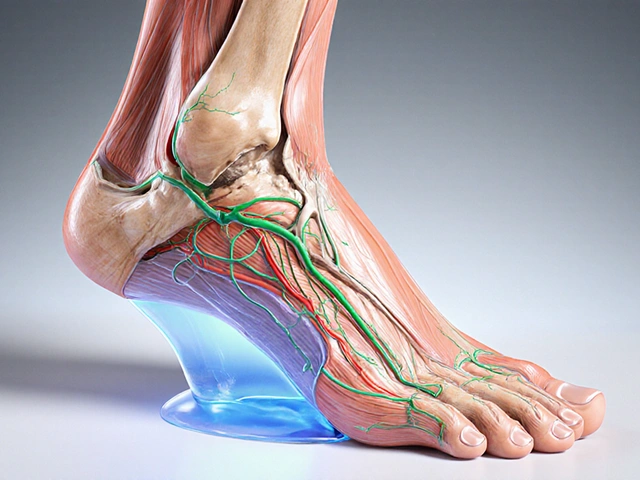 Massage Therapy for Edema: Reduce Swelling & Boost Circulation
Massage Therapy for Edema: Reduce Swelling & Boost Circulation
 How Osteoarthritis and Osteoporosis Influence Each Other
How Osteoarthritis and Osteoporosis Influence Each Other
 Sleep and Fertility: How to Boost Reproductive Health with Better Rest
Sleep and Fertility: How to Boost Reproductive Health with Better Rest
Josh josh
January 27, 2026 AT 12:40just quit xanax cold turkey once thought i was gonna die but lived to tell it lol
Mohammed Rizvi
January 28, 2026 AT 11:33the real villain here isnt the benzo its the doctor who prescribed it like candy while you were crying over a breakup
Dan Nichols
January 29, 2026 AT 11:29youre all missing the point the real issue is that psychiatry has turned anxiety into a pharmaceutical product
people dont need tapering they need to stop believing theyre broken
if you cant handle life without a chemical crutch maybe the problem isnt the drug
the 2024 guidelines are just corporate propaganda dressed as science
im not saying dont taper im saying dont start in the first place
theres no such thing as safe long term benzo use only delayed consequences
your brain was fine before the pill
why are we normalizing chemical sedation as a lifestyle choice
youre not addicted to xanax youre addicted to avoiding your own thoughts
the taper is just a placebo for guilt
Renia Pyles
January 31, 2026 AT 04:48oh so now were supposed to trust doctors who gave us 30mg of xanax a day for 5 years because we were sad
yeah right
theyll tell you to taper then disappear when you start shaking
imagine being told to cut your dose by 10% while your heart is pounding out of your chest
the system is designed to keep you dependent not to help you quit
my doctor laughed when i asked for help
you think this is science
its corporate control wrapped in medical jargon
the only thing safe about tapering is the profit margin for pharma
rasna saha
February 1, 2026 AT 19:49i tapered over 14 months and it was the hardest thing ive ever done
but i did it with therapy and a support group
some days i cried for hours
some days i felt like i was losing my mind
but i kept going because i wanted to feel real again
youre not weak for needing help
youre brave for trying
if you need someone to talk to im here
no judgment just listening
Skye Kooyman
February 2, 2026 AT 21:26so if i switch from xanax to valium does that mean im just swapping one problem for another
or is it actually helping
also what even are brain zaps
do they feel like a static shock
or more like a tiny lightning bolt
just curious
James Nicoll
February 4, 2026 AT 10:44ah yes the classic benzo taper narrative
the brave soul conquers addiction through science and patience
while ignoring the fact that the entire system created this problem
we medicate sadness because we dont know how to sit with it
the taper is just a bandaid on a bullet wound
and the doctors? theyre the ones who handed you the gun
congrats you survived
now go be productive
Uche Okoro
February 6, 2026 AT 04:35the pharmacokinetic profile of diazepam makes it the optimal agent for pharmacological de-escalation in chronic benzodiazepine-dependent populations
its long half-life and active metabolites mitigate receptor supersensitivity
this is evidenced by reduced incidence of rebound anxiety and seizure threshold destabilization
however the lack of standardized titration protocols across primary care settings remains a critical implementation gap
furthermore comorbidities such as hepatic impairment necessitate individualized dosing algorithms
the 2024 joint guideline represents a paradigm shift but adherence remains suboptimal
clinical decision support tools are urgently required
Kipper Pickens
February 8, 2026 AT 01:09the real issue isnt the taper its the lack of integration between mental health and primary care
you cant fix a systemic problem with a pill schedule
people need housing therapy social connection and purpose
not a 5% reduction every 28 days
we treat symptoms not causes
and then wonder why no one gets better
the taper is just a distraction
the real work is rebuilding a life
Joanna Domżalska
February 9, 2026 AT 09:01so youre telling me the solution to being addicted to a drug is to take another drug
and call it science
brilliant
just like how we solve obesity with diet pills
and depression with antidepressants
and insomnia with sleeping pills
we keep medicating the symptoms because the system cant handle real healing
its not a taper its a trap
youre not getting better
youre just changing the flavor of your prison
Faisal Mohamed
February 10, 2026 AT 00:21just started my taper 🙌
switched to diazepam last week
brain zaps are wild 😵⚡
but im feeling more present than i have in years
therapy is a game changer 💬
no more panic attacks
just slow steady progress
you got this 💪
bella nash
February 10, 2026 AT 07:28It is imperative to underscore the necessity of a meticulously structured, clinically supervised, and individually calibrated reduction protocol when discontinuing benzodiazepines
Failure to adhere to evidence-based guidelines may result in significant morbidity
Moreover, the presence of concomitant psychiatric or somatic conditions necessitates a multidisciplinary approach
Furthermore, the regulatory framework governing prescription practices must be harmonized across jurisdictions
Without such standardization, patient safety remains compromised
Sally Dalton
February 10, 2026 AT 18:22i just want to say thank you to everyone who shared their story
i was scared to even start reading this
but seeing you all talk about it made me feel less alone
im gonna talk to my doctor tomorrow
im not ready yet but im trying
and thats enough for today
youre all doing amazing things
even if it feels slow
even if it hurts
i see you