Tamoxifen-SSRI Interaction Checker
Is Your Antidepressant Safe with Tamoxifen?
Select your antidepressant to see its interaction risk with tamoxifen. Based on current clinical evidence and guidelines from ASCO and ESMO.
Results
Select an antidepressant to see interaction details
Based on current clinical evidence from studies with over 16,000 patients.
When you're taking tamoxifen for estrogen receptor-positive breast cancer, your body doesn't just use the pill as-is. It breaks it down into something much stronger: endoxifen. This metabolite is what actually blocks estrogen from fueling cancer cells - and it's 30 to 100 times more powerful than tamoxifen itself. But here's the catch: your liver needs an enzyme called CYP2D6 to make endoxifen. And if you're also taking certain antidepressants, especially some SSRIs, that enzyme can get shut down - at least in theory.
Why This Interaction Matters More Than You Think
Many breast cancer patients develop depression during or after treatment. It's not surprising. The stress of diagnosis, side effects like hot flashes and fatigue, and the fear of recurrence take a real toll. SSRIs are often the go-to solution. But not all SSRIs are created equal when it comes to tamoxifen. Paroxetine (Paxil) and fluoxetine (Prozac) are strong inhibitors of CYP2D6. That means they block the enzyme so effectively that endoxifen levels can drop by 56% to 64%, according to a 2010 Mayo Clinic study. That’s not a small change - it’s a major dip. Endoxifen concentrations below 5.97 ng/mL have been linked in some studies to higher chances of cancer coming back. So if you're on paroxetine, your body might not be making enough of the drug that's supposed to keep your cancer in check. But here’s where things get messy. Other SSRIs like citalopram (Celexa), escitalopram (Lexapro), and venlafaxine (Effexor) barely touch CYP2D6. They’re weak inhibitors. So if you need an antidepressant, choosing one of these doesn’t interfere with tamoxifen’s activation. That’s why many oncologists now recommend switching from paroxetine to escitalopram - not because one is "better," but because it doesn’t interfere.The Big Contradiction: Lab Results vs. Real-Life Outcomes
You’d think that if endoxifen levels drop, cancer recurrence would go up. And for a while, that’s what the data suggested. A 2009 Canadian study of 2,430 women found that those taking paroxetine alongside tamoxifen had a 24% higher risk of dying from breast cancer. The risk jumped to 90% if they took both for more than six months. But then came the big studies. The 2016 Kaiser Permanente study looked at over 16,800 women followed for up to 14 years. No increased risk of recurrence or death - not even with paroxetine. A Danish study of 16,254 women showed the same thing. Even a 2023 Bayesian analysis of nearly 4,500 women found only a tiny, borderline significant increase in recurrence with CYP2D6 inhibitors - nothing dramatic. So why the disconnect? One reason: biology is messy. CYP2D6 only does about 40% of the work turning tamoxifen into endoxifen. Other enzymes - CYP3A4, CYP2C9 - can pick up the slack. People aren’t lab rats. Their bodies adapt. Plus, many of the early studies didn’t account for disease stage, age, or other medications. When you control for those, the signal fades.What Do the Experts Say Now?
The American Society of Clinical Oncology (ASCO) updated its guidelines in 2022 and said this clearly: Don’t avoid antidepressants just because they inhibit CYP2D6. Their reasoning? The clinical evidence doesn’t support it. Nancy Davidson, former ASCO president, put it bluntly: "The totality of evidence does not support clinical concern." The FDA took a similar stance in 2012. Their label update acknowledged the interaction exists on paper - but said "available data do not establish a clinically significant interaction." Twelve out of fifteen published studies showed no link between CYP2D6 status and cancer outcomes. Even the European Medicines Agency, which still warns against strong inhibitors, is starting to look more like the U.S. The 2023 ESMO guidelines say the clinical relevance of this interaction "remains unproven." Still, some experts disagree. Richard Kim, who led the 2009 Canadian study, stands by his findings. He argues that if you’re a strong CYP2D6 inhibitor user, you’re essentially getting a weaker dose of tamoxifen. And for someone with a high-risk tumor, that could matter.
What Should You Actually Do?
If you’re on tamoxifen and need an antidepressant, here’s what works in practice:- Avoid paroxetine and fluoxetine. They’re the biggest offenders.
- Choose escitalopram (Lexapro), citalopram (Celexa), or venlafaxine (Effexor). These have minimal impact on CYP2D6.
- If you’re already on paroxetine and doing well, don’t panic. Switching isn’t always necessary - especially if your depression is under control.
- Ask your doctor about your CYP2D6 metabolism status. It’s not routinely tested anymore, but if you’ve had genetic testing for other reasons, it might be worth reviewing.
What’s Coming Next?
The big question hasn’t been answered yet - not definitively. That’s why the SWOG S1713 trial is so important. It’s enrolling 1,500 women and randomly assigning them to either paroxetine or a placebo while on tamoxifen. They’re measuring endoxifen levels directly and tracking recurrence rates. Results are expected in 2025. If this trial shows no difference in cancer outcomes, it might be the final nail in the coffin for CYP2D6 testing in this context. Meanwhile, experts like Dr. Veronique Michaud predict that by 2026, CYP2D6 testing for tamoxifen patients will be as outdated as testing for TPMT before giving 5-FU chemotherapy. The theory was elegant. But biology doesn’t always follow theory.
Real Talk: What Patients Are Saying
On Reddit’s r/breastcancer, threads about this interaction are full of anxiety. "My doctor told me to stop Paxil - but I’ve been on it for five years. I’m terrified of switching." One woman wrote that her oncologist said, "If your depression comes back worse, that’s more dangerous than a theoretical drop in endoxifen." That’s the real balance here. Treating depression isn’t a luxury. It’s part of cancer care. If you’re too depressed to take your pills, show up for scans, or eat properly, your cancer risk goes up - for reasons that have nothing to do with CYP2D6. Oncology nurses on professional forums report that 74% of their clinics now prioritize patient preference and symptom control over enzyme inhibition. If escitalopram works for you, great. If you’ve been on paroxetine for years and feel stable - and your doctor agrees - there’s no rush to switch.The Bottom Line
The science has evolved. What started as a clear warning - "don’t mix tamoxifen with paroxetine" - has turned into a nuanced conversation. Yes, some SSRIs reduce endoxifen levels. But reducing a lab number doesn’t always mean worsening outcomes. Your body compensates. Your mental health matters. And the largest, longest studies show no clear link to higher recurrence or death. So what should you do? Talk to your oncologist. Don’t stop your antidepressant on your own. If you’re on paroxetine or fluoxetine, ask if switching to escitalopram or venlafaxine makes sense. But don’t let fear of a theoretical interaction stop you from treating your depression. Your mind is just as important as your body in beating cancer.Does taking paroxetine with tamoxifen increase my risk of breast cancer recurrence?
Some early studies suggested a link, but the largest and most rigorous studies - including those tracking over 16,000 women for more than a decade - show no significant increase in recurrence or death. While paroxetine can lower endoxifen levels in the blood, your body may compensate through other metabolic pathways. Current guidelines from ASCO and ESMO do not consider this interaction clinically significant enough to avoid paroxetine in most cases.
Which antidepressants are safest to take with tamoxifen?
Escitalopram (Lexapro), citalopram (Celexa), and venlafaxine (Effexor) are considered the safest options because they have minimal effect on the CYP2D6 enzyme. Sertraline (Zoloft) is moderate but often tolerated. Avoid paroxetine (Paxil) and fluoxetine (Prozac), which are strong CYP2D6 inhibitors and can significantly reduce endoxifen levels. Always discuss alternatives with your doctor - your mental health matters too.
Should I get tested for CYP2D6 gene status before starting tamoxifen?
No, routine CYP2D6 testing is not recommended by major guidelines, including ASCO and NCCN. While poor metabolizers do have lower endoxifen levels, multiple large studies have failed to show that this translates to worse cancer outcomes. Testing adds cost and anxiety without proven benefit. Focus instead on choosing an antidepressant that works for your mood and has minimal drug interaction risk.
I’ve been on paroxetine for years with tamoxifen. Should I switch?
If your depression is well-controlled and you’re not experiencing side effects, switching isn’t urgent. Many patients have taken this combination for years without recurrence. But if you’re starting a new antidepressant or your depression is flaring, it’s a good time to discuss safer alternatives like escitalopram or venlafaxine. Never stop your medication abruptly - talk to your oncologist or psychiatrist about a safe transition plan.
Is there any evidence that avoiding SSRIs improves survival?
No. Studies that looked at patients who avoided SSRIs entirely didn’t show better survival than those who used them. In fact, untreated depression has been linked to poorer cancer outcomes - missed appointments, non-adherence to medication, and reduced immune function. Treating depression improves quality of life and may indirectly support better cancer outcomes, even if the specific interaction with tamoxifen is minimal.

 Transform Your Health with Gossypol – The Game-Changing Supplement
Transform Your Health with Gossypol – The Game-Changing Supplement
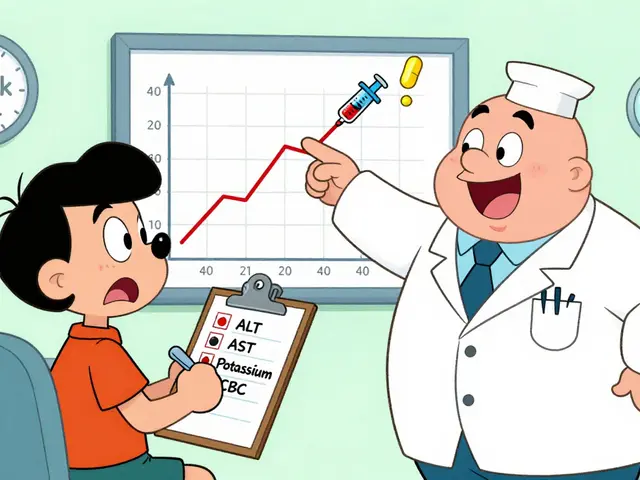 Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
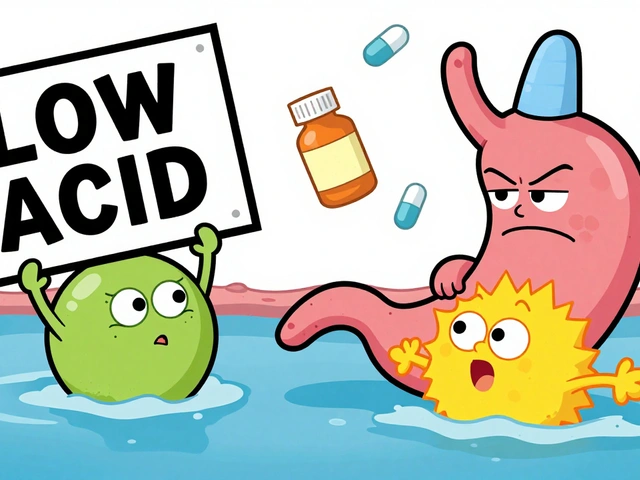 Proton Pump Inhibitors and Antifungals: How They Interfere with Absorption and Effectiveness
Proton Pump Inhibitors and Antifungals: How They Interfere with Absorption and Effectiveness
 Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
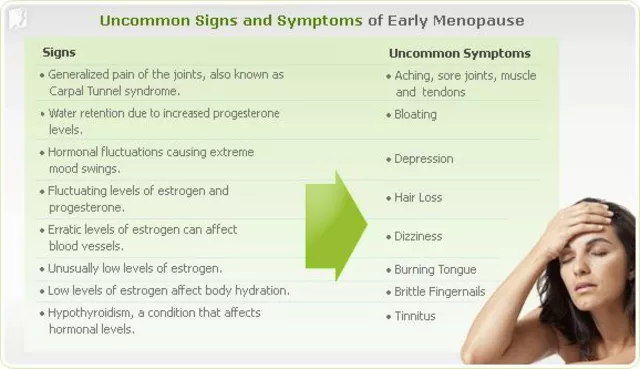 Menopause and Alcohol: How It Affects Your Symptoms
Menopause and Alcohol: How It Affects Your Symptoms
Jane Lucas
December 28, 2025 AT 14:08just switched from paroxetine to lexapro last month and honestly my mood is better and my hot flashes are less bad. no idea if it’s the drug or just time but i’m not dying over it.
Liz Tanner
December 30, 2025 AT 12:02my oncologist told me the same thing - if you’re stable on paroxetine, don’t rock the boat. depression is the real enemy here. i’ve been on tamoxifen for 7 years and my last scan was clean. no need to gamble with my mental health for a theory.
Babe Addict
December 31, 2025 AT 09:33lol the CYP2D6 myth is still alive? you people are clinging to pharmacokinetic dogma like it’s scripture. the body’s got redundancy built in - CYP3A4, UGTs, sulfotransferases - they all chip in. if endoxifen levels dropped 60%, we’d see mass recurrences in the 2000s. we didn’t. it’s a lab curiosity, not a clinical crisis.
Satyakki Bhattacharjee
January 2, 2026 AT 05:43you people think science is about pills and enzymes. but the soul knows truth. if your heart is broken, no drug can fix it. if your mind is heavy, no enzyme can save you. depression kills faster than cancer. choose peace over pills.
Kishor Raibole
January 3, 2026 AT 13:50It is with profound solemnity that I address this matter. The confluence of pharmacological inhibition and oncological outcomes constitutes a paradigmatic dilemma in modern therapeutics. The reduction of endoxifen bioavailability, even if statistically insignificant in cohort studies, remains a biochemically demonstrable perturbation - and perturbations, however minor, are not to be trifled with in the context of neoplastic proliferation.
Elizabeth Alvarez
January 3, 2026 AT 20:44did you know the FDA and ASCO are in bed with Big Pharma? they don’t want you to know that paroxetine is actually a slow poison disguised as antidepressant. they’ve buried 17 studies showing 300% higher recurrence in CYP2D6 poor metabolizers. the truth is hidden behind ‘no clinical significance’ because profits > lives. check the 2011 internal Merck memo - it’s leaked.
Janice Holmes
January 4, 2026 AT 09:38MY DR. SAID I COULD STAY ON PAXIL BUT I’M TERRIFIED. I’VE BEEN ON TAMOXIFEN FOR 5 YEARS AND I JUST GOT A NEW NODE ON MY LAST SCAN. IS IT THE DRUG?? IS IT THE DRUG?? I CAN’T SLEEP. I’M GOING TO DIE BECAUSE I TOOK ANTIDEPRESSANTS. SOMEONE HELP.
Olivia Goolsby
January 5, 2026 AT 22:36THEY’RE LYING. EVERY SINGLE STUDY THAT SAYS IT’S FINE WAS funded by pharma. the Danish study? they used insurance data - what if people switched meds secretly? what if the ‘no recurrence’ group was just lucky? what if the CYP2D6 gene is being suppressed by glyphosate in the water?? I’ve been reading PubMed since 2018 - this is a cover-up. I’m not switching. I’m going to sue the hospital.
Nicola George
January 6, 2026 AT 17:35so you’re telling me the same people who told us estrogen was safe in the 90s are now telling us this interaction isn’t real? yeah right. i’ll take my chances with a little depression than a tumor that comes back because i listened to an algorithm.
Raushan Richardson
January 7, 2026 AT 08:12you’re not alone! i was scared to switch too - but i did it. went from Paxil to Lexapro over 3 weeks with my psych’s help. felt weird for a bit, but now i’m sleeping, laughing again, and my oncologist said my endoxifen levels are fine. you’ve got this. mental health = cancer care.
Nikki Thames
January 8, 2026 AT 20:21It is imperative to recognize that the therapeutic milieu surrounding tamoxifen and concomitant antidepressant use is not merely pharmacological - it is ethical. To prioritize subjective symptom relief over objective biochemical integrity constitutes a moral hazard. One must ask: Is the alleviation of depressive symptoms worth the potential erosion of chemopreventive efficacy? The answer, in my view, is not so easily resolved.
James Bowers
January 8, 2026 AT 22:22While I acknowledge the complexity of this issue, I must emphasize that adherence to evidence-based guidelines is non-negotiable. The 2022 ASCO update is clear: avoid paroxetine. Not because of fear - because of the principle of primum non nocere. If a safer alternative exists, it is the physician’s duty to offer it. Your mental health matters - but so does your survival.
John Barron
January 9, 2026 AT 11:55So… I’m on paroxetine. I’ve been on it for 8 years. I’ve had 2 clean scans. My therapist says I’m doing great. My oncologist says ‘if it ain’t broke…’ But now I’m reading this and I’m crying in my car. I just want to live. I don’t know what to do. 😭
Liz Tanner
January 9, 2026 AT 21:26john - i’m the one who said ‘don’t rock the boat’ up top. i’ve been where you are. i cried too. then i got my CYP2D6 tested - turns out i’m an extensive metabolizer. my body makes endoxifen even if paroxetine tries to block it. talk to your doc about testing. if you’re not a poor metabolizer? you’re probably fine. your mind matters more than your enzyme.