Medication Monitoring Timeline Calculator
This tool helps you determine when to schedule blood tests based on your medication and health factors. Always consult your healthcare provider for personalized recommendations.
Select Your Medication
Recommended Monitoring Timeline
When you start a new medication, you’re not just hoping it works-you’re also hoping it doesn’t make you sick. But many side effects don’t show up right away. Some creep in slowly. Others only appear after months, or after you add another drug to the mix. That’s why routine monitoring isn’t optional-it’s your safety net.
Why Waiting for Symptoms Isn’t Enough
Most people think if something’s wrong, they’ll feel it. But that’s not how drugs work. Take statins, for example. A common side effect is muscle damage, but you might not notice until your creatine kinase levels spike. Or consider blood thinners like warfarin-your INR can drift out of range for days before you bleed internally. By the time you feel dizzy or bruise easily, it’s already too late. Clinical trials don’t catch everything. They test drugs on a few thousand people over months. Real life? Millions take the same drug for years, often with other meds, chronic conditions, or changing liver and kidney function. That’s where things go wrong. Studies show only about 6% of serious drug reactions ever get reported to official systems like the FDA’s FAERS. That means 94% slip through the cracks-until someone ends up in the ER.What Tests Actually Matter-and When
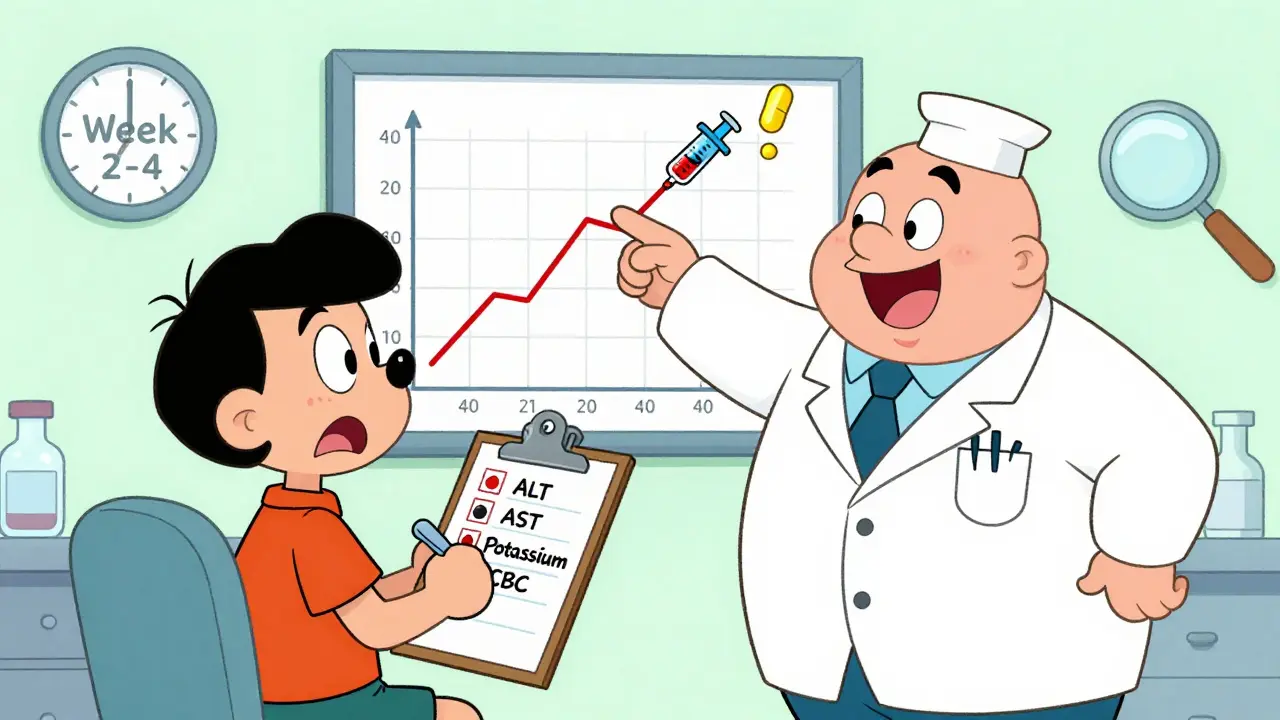
Not every drug needs a full lab panel. But for many, routine blood tests are the only way to catch problems before they become emergencies.- Liver enzymes (ALT, AST, bilirubin): Needed within 4-6 weeks of starting drugs like statins, antibiotics, or seizure meds. If ALT rises more than 3x the upper limit, stop the drug and retest.
- Kidney function (creatinine, eGFR): Essential for diabetes meds, NSAIDs, and some blood pressure drugs. Check at baseline, then every 3 months if you’re over 65 or have existing kidney issues.
- Electrolytes (potassium, sodium): Critical for diuretics, ACE inhibitors, and lithium. Check within 2 weeks of starting or changing dose. A potassium level below 3.5 or above 5.5 can trigger dangerous heart rhythms.
- Blood counts (CBC): Required for chemotherapy, antithyroid drugs, and some autoimmune treatments. Monitor every 2-4 weeks initially. Low white cells? That’s a red flag.
- Therapeutic drug monitoring (TDM): For drugs like digoxin, vancomycin, or anticonvulsants. Blood levels need to stay in a narrow window. Too low? It doesn’t work. Too high? You get toxicity.
Timing Isn’t Arbitrary-It’s Based on Science
When you get tested matters just as much as what’s tested. Here’s the real-world timeline most doctors follow:- Baseline: Before you even take the first pill. This gives you a reference point.
- Week 2-4: Early warning window. Most side effects show up here. For drugs like lithium or carbamazepine, this is when toxicity can start.
- Week 8-12: Second check. Confirms stability. If you’re still feeling off, this is when you dig deeper.
- Every 3-6 months: Maintenance phase. For long-term meds like metformin, beta-blockers, or antidepressants, this is the minimum.
- After any dose change: Always retest. Even a 5mg increase can tip the balance.

What You Can Do at Home
You don’t have to wait for your doctor to catch something. Start tracking your own symptoms. Keep a simple log:- Date and time of each symptom
- What it felt like (e.g., "tingling in fingers," "dizziness when standing")
- Severity on a scale of 1-10
- Duration (minutes, hours, days)
- Medication dose taken that day
- Potential triggers (alcohol, caffeine, new food, stress, other meds)
How Technology Is Changing the Game
Hospitals and clinics are now using tools that scan your electronic health records for hidden patterns. Stanford researchers found they could predict side effects up to two years before the FDA issued warnings-just by reading doctors’ notes. That’s not science fiction. It’s happening now. These systems look for things like:- "Patient reported fatigue after starting lisinopril"
- "New-onset rash following amoxicillin"
- "Elevated liver enzymes after switching from simvastatin to atorvastatin"

Why Polypharmacy Is the Silent Killer
If you’re on five or more medications-which 40% of adults over 65 are-you’re at higher risk. Each new drug adds layers of risk. A blood pressure pill might raise your potassium. A painkiller might hurt your kidneys. A sleep aid might make you dizzy. Together? That’s a perfect storm. Studies show the risk of a serious side effect jumps by 7% for every additional drug. At 10 meds? You’re looking at a 70% chance of at least one interaction. And most of these aren’t caught until someone falls, has a stroke, or ends up in the hospital. That’s why pharmacists now do medication reviews-especially for older patients. Ask for one. Bring a list of everything you take, including supplements. Your pharmacist can spot the red flags your doctor might miss.What to Do If You Notice Something Strange
You don’t need to wait for your next appointment. If you feel off, do this:- Don’t stop the drug unless it’s life-threatening (like swelling, trouble breathing, or chest pain). Stopping suddenly can be dangerous.
- Write it down using the log format above.
- Call your doctor or pharmacist within 24-48 hours. Say: "I’ve noticed [symptom] since I started [medication]. It’s happening [frequency]. I’ve attached my log. Should I get tested?"
- Ask for the test by name: "Can we check my liver enzymes? My potassium? My CBC?"
The Bottom Line
Medications save lives. But they also carry silent risks. Routine monitoring isn’t about being paranoid. It’s about being smart. You wouldn’t skip an oil change on your car. Don’t skip your blood tests. Your body gives you clues. Your doctor gives you tools. But you’re the one who connects the dots. Track your symptoms. Know your tests. Ask questions. If your provider says, "We don’t need to check that," ask why. If they can’t explain, get a second opinion. Early detection doesn’t mean you’ll avoid every side effect. But it means you’ll catch the ones that matter-before they turn into emergencies.How soon after starting a new medication should I get blood tests?
For most medications, the first blood test should be done between 2 and 4 weeks after starting. This is when early side effects like liver stress, electrolyte shifts, or low blood cell counts typically show up. Some drugs, like lithium or methotrexate, require testing even sooner-within 7-10 days. Always follow your provider’s specific instructions, but if none are given, ask for a baseline test at 2 weeks.
Can side effects appear years after taking a drug?
Yes. Some side effects, like certain types of kidney damage from NSAIDs or bone loss from long-term steroid use, develop slowly over years. Others, like tardive dyskinesia from antipsychotics, may not appear until after months or even years of use. That’s why ongoing monitoring-even when you feel fine-is critical. Just because you haven’t had a problem yet doesn’t mean you won’t.
Do over-the-counter drugs and supplements need monitoring too?
Absolutely. Many people think OTC meds are harmless, but that’s not true. Regular use of ibuprofen or naproxen can damage your kidneys and raise blood pressure. High-dose vitamin D can cause calcium buildup in your blood. St. John’s Wort can interfere with antidepressants, birth control, and blood thinners. Always tell your doctor what you’re taking-even if you bought it at the grocery store.
What if my doctor says I don’t need regular tests?
Ask why. For some low-risk medications, like certain antihistamines or topical creams, frequent testing isn’t needed. But for most oral drugs-especially those affecting the liver, kidneys, or blood-regular monitoring is standard. If your doctor dismisses your concern without explaining the reasoning, get a second opinion. Your safety isn’t up for debate.
How do I know if a symptom is from my medication or something else?
Track it. Note when the symptom started relative to when you began the drug. Did it get worse after a dose increase? Does it go away when you skip a dose? Does it happen only after eating certain foods? This pattern helps your doctor separate drug-related issues from other causes like infections, stress, or aging. Don’t guess-document.
Are there apps or tools to help track side effects?
Yes. Apps like Medisafe, MyTherapy, and even simple note-taking tools on your phone work well. Some let you set reminders for tests and log symptoms with severity scales. The key isn’t the app-it’s consistency. Whether you use paper, phone, or spreadsheet, the goal is to record details accurately and regularly.
Can routine monitoring prevent hospitalizations?
Yes. Studies show that patients who stick to recommended monitoring schedules have up to 40% fewer hospitalizations due to drug-related problems. Catching a rising creatinine level or a dropping white blood cell count early lets doctors adjust your treatment before you get sick enough to need emergency care. Monitoring isn’t just about safety-it’s about avoiding costly, avoidable crises.
 Multiple Myeloma Hope Stories: Survival, Treatments & Resilience
Multiple Myeloma Hope Stories: Survival, Treatments & Resilience
 Compare Inderal (Propranolol) with Alternatives: What Works Best for Anxiety, Heart Conditions, and Migraines
Compare Inderal (Propranolol) with Alternatives: What Works Best for Anxiety, Heart Conditions, and Migraines
 Insulin Therapy Side Effects: Managing Hypoglycemia and Weight Gain
Insulin Therapy Side Effects: Managing Hypoglycemia and Weight Gain
 Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
 Renal Diet Guide: How to Manage Sodium, Potassium, and Phosphorus with Chronic Kidney Disease
Renal Diet Guide: How to Manage Sodium, Potassium, and Phosphorus with Chronic Kidney Disease
mike swinchoski
January 13, 2026 AT 12:03People don't get it. If you're on more than 3 meds, you're already playing Russian roulette. No one tells you this until you're in the ER with a potassium level of 6.2.
Priyanka Kumari
January 14, 2026 AT 21:57This is exactly why I started keeping a digital log after my mom had a bad reaction to a new blood pressure med. Tracking symptoms and timing helped her doctor catch a dangerous interaction before it got worse. Small habits save lives.
Scottie Baker
January 15, 2026 AT 21:17I had a doc tell me I didn't need liver tests on statins because I 'felt fine.' Two months later I was in the hospital with rhabdo. Don't trust 'feelings.' Trust labs. Period.
Gregory Parschauer
January 16, 2026 AT 11:49Let me be crystal clear: if your provider isn't proactively ordering baseline and follow-up labs for any systemic medication, they're not practicing medicine-they're gambling with your organs. This isn't 'health advice,' it's basic pharmacology. The fact that this even needs explaining is a national disgrace. You think your doctor is looking out for you? They're probably too busy chasing productivity quotas to even open your chart. Your body isn't a suggestion box. Test. Track. Demand. Or die quietly.
Adam Vella
January 18, 2026 AT 02:49One must consider the epistemological framework underpinning pharmaceutical surveillance. The clinical paradigm, rooted in reductionist biomedicine, fails to account for emergent systemic dysregulation arising from polypharmacological interactions. Empirical data, while useful, remains inherently limited by its reliance on post-hoc observation rather than predictive modeling. The true solution lies not in reactive testing, but in the integration of systems biology into routine care-a paradigm shift currently hindered by institutional inertia and profit-driven healthcare architecture.
vishnu priyanka
January 19, 2026 AT 21:27In India, we call this 'dawa ka dhamaal'-the medicine circus. Everyone's on 8 pills, no one checks anything, and grandmas just keep taking whatever the pharmacist hands them. My uncle took NSAIDs for 10 years and never got a kidney test. Now he's on dialysis. This post? It's a lifeline. Share it with your auntie.
Angel Tiestos lopez
January 20, 2026 AT 21:46bro this is so real 🙏 i started tracking my symptoms after my anxiety med made me feel like a zombie. now i know it’s the 10mg dose + coffee = brain fog. saved me a trip to the doc. apps are fire 🔥
Pankaj Singh
January 22, 2026 AT 10:52Stop pretending this is about safety. It's about liability. Hospitals don't want you to get sick-they want you to sign a waiver saying you were warned. That's why they 'recommend' tests. If you don't get them and crash? It's your fault. This whole system is designed to absolve doctors, not protect patients. Don't be fooled.
Robin Williams
January 23, 2026 AT 16:05we’re all just trying to survive the pharmacological circus. the body’s not broken-it’s just overwhelmed. listen to it. write it down. don’t let the system gaslight you into thinking you’re ‘overreacting.’ you’re not. you’re awake.
Anny Kaettano
January 23, 2026 AT 23:23As someone who works in patient advocacy, I see this daily. One woman came in with severe fatigue-her doctor said it was 'just stress.' Turns out, her lithium level was 2.8 (toxic). She was 12 hours from seizures. We got her tested because she kept pushing. Never underestimate the power of saying, 'I need this test.' You're not being difficult. You're being alive.
Kimberly Mitchell
January 25, 2026 AT 18:18Why are we normalizing the idea that you need to be your own medical detective? This shouldn’t be a burden. It’s a systemic failure. The fact that patients have to log symptoms, track labs, and demand tests is evidence that medicine has abandoned its duty. I’m tired of being told to 'advocate for myself' when the system was never designed to care.
Angel Molano
January 26, 2026 AT 18:51Stop. Just stop. If you're on a statin, check your liver. If you're on diuretics, check your potassium. That's it. No philosophy. No apps. No logs. Just do the damn test. You're not special. You're not immune. Test. Now.
Nelly Oruko
January 27, 2026 AT 16:17i’ve been on metformin for 5 years. my doc said i dont need kidney tests bc i’m ‘young and healthy.’ i got one anyway. creatinine was rising. they adjusted my dose. saved my kidneys. never trust ‘you’re fine.’ i’m not a doctor, but i know when to ask.