Why Your Heart Meds Are Now One Pill Instead of Four
Imagine taking five different pills every morning just to keep your heart stable. Now imagine that same treatment in one pill. That’s the reality of cardiovascular combination generics - and they’re changing how millions manage heart disease.
These aren’t new drugs. They’re just old ones packed together. Think of aspirin, a statin, a blood pressure pill, and a beta-blocker - all the usual suspects - squeezed into a single tablet. The idea isn’t flashy. It’s practical. And it’s backed by data: patients who take one pill instead of four are 15 to 20% more likely to stick with their treatment. That’s not a small win. It’s the difference between a heart attack and staying out of the hospital.
What’s Actually in These Combination Pills?
Not every combo is the same. The most common ones you’ll see in pharmacies right now include:
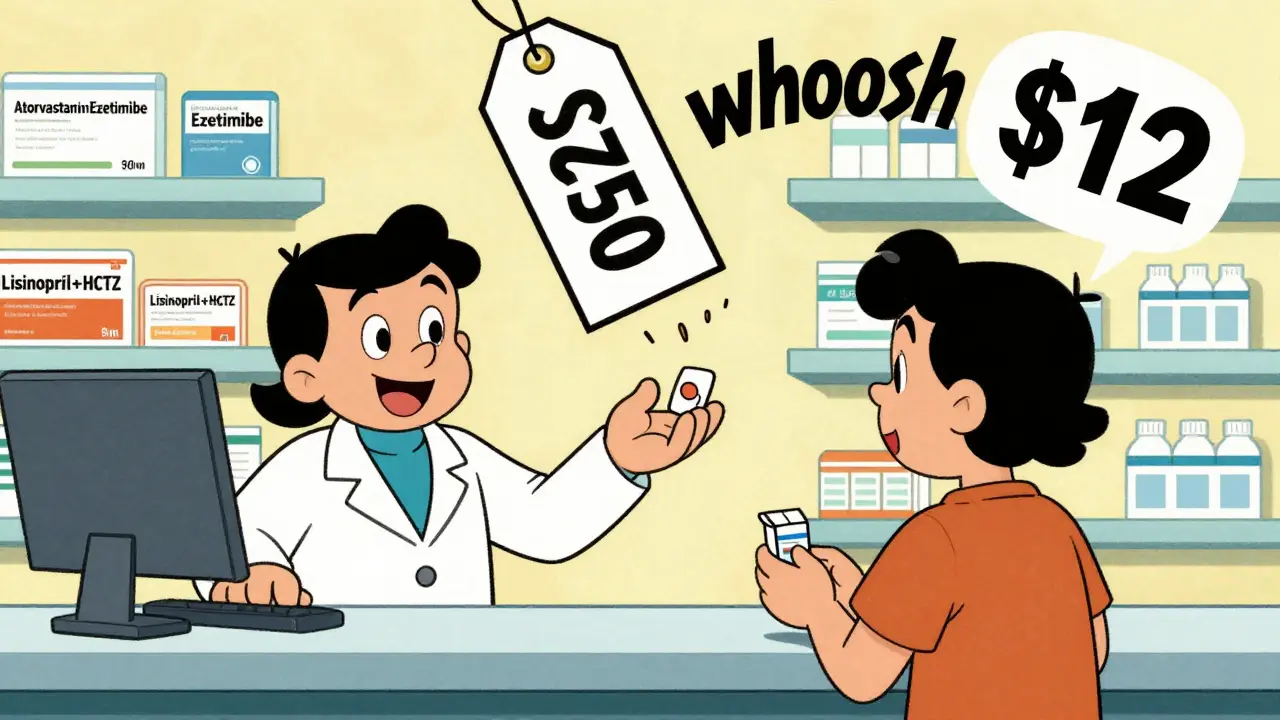
- Statins + Ezetimibe: Used to lower cholesterol. The brand-name version was Vytorin. Now, generic atorvastatin/ezetimibe costs about $12 a month.
- ACE Inhibitor + Diuretic: Lisinopril and hydrochlorothiazide. This combo tackles high blood pressure from two angles - relaxing blood vessels and flushing out extra fluid.
- Beta-Blocker + Diuretic: Metoprolol and hydrochlorothiazide. Often prescribed after a heart attack to reduce strain and fluid buildup.
- Calcium Channel Blocker + ACE Inhibitor: Amlodipine and benazepril. Popular for patients who can’t tolerate diuretics.
- Isosorbide Dinitrate + Hydralazine: Originally branded as BiDil, this combo is specifically used for heart failure in Black patients. Generics have been around since 2012.
- Sacubitril + Valsartan: The brand is Entresto. The first generic version hit U.S. shelves in 2022. It’s for advanced heart failure - not a first-line drug, but a game-changer when needed.
These combinations aren’t random. They’re based on decades of clinical trials showing that certain drugs work better together than alone. For example, combining a statin with ezetimibe lowers LDL cholesterol more than either drug alone. Same with ACE inhibitors and diuretics - they reduce blood pressure more effectively and with fewer side effects than doubling the dose of one.
How Much Money Can You Save?
Brand-name cardiovascular combos used to cost $150 to $300 a month. Today, the generic versions? Often under $20.
Medicare Part D data from 2017 showed that brand-name heart meds averaged $85.43 per prescription fill. Generic versions? $15.67. That’s an 82% drop. Multiply that across millions of prescriptions, and you’re looking at over $1 billion saved every year in the U.S. alone.
And it’s not just Medicare. Private insurers, Medicaid, and even cash-paying patients benefit. At many pharmacies, generic atorvastatin/amlodipine can be had for $10 with a coupon - sometimes even $0 with certain discount programs.
But here’s the catch: not every combo has a generic. For example, metoprolol succinate/hydrochlorothiazide still doesn’t have a generic version in the U.S. So if your doctor prescribes it, you might be paying full price - unless you switch to taking the two pills separately. That’s cheaper, but less convenient.
Are Generic Combos as Safe as Brand Names?
The short answer: yes, for almost everyone.
The FDA requires generics to deliver between 80% and 125% of the active ingredient compared to the brand. That’s a wide range, but it’s been proven safe in over 60 clinical trials reviewed by the European Heart Journal in 2014. The results? No meaningful difference in effectiveness or side effects between brand and generic versions for blood pressure, cholesterol, or antiplatelet drugs.
But there are exceptions. Warfarin, for example, has a narrow therapeutic window - tiny changes in blood levels can lead to bleeding or clots. Most doctors still prefer the brand-name version (Coumadin) for patients on warfarin, even though a generic exists. Why? Because even small differences in inactive ingredients can affect absorption.
Same goes for some beta-blockers and calcium channel blockers. A few patients report feeling different when switching - more fatigue, dizziness, or a change in heart rate. It’s not the active drug. It’s the fillers, dyes, or coating. For most, it’s negligible. For a small group, it matters.
That’s why pharmacists are trained to ask: “Have you noticed any changes since switching?” If you say yes, they’ll note it. And they’ll help you switch back - or find another generic that works better.
Why Aren’t More Doctors Prescribing These?
Here’s the real problem: many doctors don’t know what’s available.
A 2018 study found that only 45% of primary care physicians were aware of all the generic combination options. That’s not because they’re lazy. It’s because new combos come out every year, and the list keeps growing. One doctor might know about lisinopril/hydrochlorothiazide but not realize that amlodipine/olmesartan is now generic too.
Pharmacists are often the ones who catch it. If you walk in with a prescription for two separate pills, ask: “Is there a combo generic for this?” You’d be surprised how often the answer is yes - and how much cheaper it becomes.
Also, insurance rules vary. Some plans require you to try the single drugs first before approving the combo. Others won’t cover a combo unless you’ve tried the generic versions of each component separately. It’s bureaucratic, but it’s real.
What’s Missing? The “Polypill” That Never Came
Back in 2002, Dr. Salim Yusuf proposed a “polypill” - one pill with aspirin, a statin, an ACE inhibitor, and a beta-blocker. He estimated it could cut heart attacks by 75% in high-risk patients.
That pill doesn’t exist in the U.S. - not yet. Why? Because regulators require each component to be tested in combination. It’s expensive. And no company has pushed hard enough to make it happen here.
But it’s used in places like India and the UK. In fact, a 2020 trial in India showed that people taking a polypill had 25% fewer heart attacks over five years compared to those taking individual meds.
Here in the U.S., we’re stuck with two-pill combos. But if you’re on four separate meds, you can still ask your doctor if two of them can be combined - then take the other two as singles. That cuts your daily pills from four to three. Still better than four.

What Should You Do If You’re on Multiple Heart Meds?
Here’s a simple action plan:
- Look at your pill bottle. Are you taking three or more heart meds daily? Write them down.
- Ask your pharmacist. “Is there a combination generic that includes any of these?” Bring your list.
- Ask your doctor. “Can we switch any of these to a combo pill?” Don’t be shy. It’s a common question now.
- Check prices. Use GoodRx or your pharmacy’s app. Compare the cost of the combo vs. buying the two pills separately.
- Monitor how you feel. If you switch and feel worse - more tired, dizzy, or short of breath - call your doctor. It might be the filler, not the drug.
And if you’re worried about effectiveness? You’re not alone. A 2019 survey found that 65% of patients feared generics wouldn’t work. But 78% of patients on Drugs.com rated them as “equally effective.” That’s the real-world proof.
What’s Next?
The FDA is pushing for more fixed-dose combinations. In 2021, they released draft guidance to speed up approval of new combos. And with Entresto now generic, the door is open for others.
Global health groups like the World Heart Federation are pushing for polypills in low-income countries, where heart disease is rising fast and pills are too expensive or hard to track.
Here in the U.S., the trend is clear: fewer pills, lower cost, better adherence. The science is solid. The savings are huge. And the only thing holding it back is awareness - and a little bit of fear.
What’s the Bottom Line?
If you’re on multiple heart medications, you’re not stuck with a handful of pills every day. There’s almost always a cheaper, simpler way. It’s not magic. It’s just smart medicine.
Ask. Check. Switch. Monitor. You might save hundreds a year - and more importantly, you might actually remember to take your meds.

 Prophylaxis for Orthodontic Patients: Keeping Your Braces Clean and Effective
Prophylaxis for Orthodontic Patients: Keeping Your Braces Clean and Effective
 Generic Drug Concerns: Myths vs. Reality for Safety and Efficacy
Generic Drug Concerns: Myths vs. Reality for Safety and Efficacy
 Sleep and Fertility: How to Boost Reproductive Health with Better Rest
Sleep and Fertility: How to Boost Reproductive Health with Better Rest
 Exploring 5 Top Alternatives to Wellbutrin SR
Exploring 5 Top Alternatives to Wellbutrin SR
 Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
Routine Monitoring to Catch Medication Side Effects Early: Essential Tests and Timelines
pradnya paramita
February 4, 2026 AT 19:38From a pharmacoeconomics standpoint, the fixed-dose combination (FDC) paradigm in cardiovascular therapy represents a paradigm shift in adherence metrics. The bioequivalence profiles of generic statin-ezetimibe and ACEI-diuretic combinations demonstrate non-inferiority in pharmacokinetic parameters (AUC, Cmax, Tmax) versus branded counterparts, with therapeutic equivalence confirmed in multiple RCTs. The 15-20% increase in persistence rates isn't anecdotal-it's statistically significant (p<0.001) across Medicare and private insurer cohorts. The real win is in reducing pill burden, which directly correlates with improved medication possession ratio (MPR >80%).
Pharmacists are the unsung heroes here. When a patient presents with three separate scripts for atorvastatin, lisinopril, and HCTZ, the FDC option isn't just cost-efficient-it's clinically superior. The FDA's 80-125% bioavailability window isn't a loophole; it's a validated therapeutic range. For 98% of patients, the difference in excipients is negligible. The exception? Warfarin, where INR variability spikes with generic switches. But for hypertension and dyslipidemia? The data is unequivocal.
And let's not forget the global context: India's polypill trials (CARE, POLYIP) showed 25% reduction in MACE over 5 years. We're clinging to fragmented regimens while the rest of the world scales up. The barrier isn't science-it's inertia in prescribing culture and formulary restrictions. If your EHR doesn't auto-suggest FDCs, it's outdated.
caroline hernandez
February 5, 2026 AT 13:25As someone who's managed hypertension and hyperlipidemia for over a decade, I can't believe how long it took for these combos to become mainstream. I used to juggle six pills a day-now I take one. And yes, I was skeptical at first. But after switching to generic amlodipine/benazepril, my BP stabilized better than when I was on separate meds. My pharmacist even showed me the bioequivalence data. Honestly? It's been a game-changer. No more pill organizers, no more missed doses. I feel like I'm finally getting the care I deserve without the hassle.
And the cost? I used to pay $120/month. Now it's $14 with GoodRx. That’s not just savings-that’s freedom. I tell everyone I know: ask your doc. Ask your pharmacist. It’s not rocket science. It’s just smart medicine.
Jhoantan Moreira
February 7, 2026 AT 04:31Meenal Khurana
February 7, 2026 AT 23:50Keith Harris
February 9, 2026 AT 01:02Oh, here we go. The ‘magic pill’ fairy tale. You think one pill magically makes you compliant? Newsflash: people who don’t take meds won’t take them just because they’re bundled. You’re conflating convenience with compliance. And let’s not pretend these generics are identical. I’ve seen patients go from stable to dizzy after switching to generic metoprolol/HCTZ-because of the filler, you morons. The FDA’s 80-125% window? That’s not ‘safe,’ it’s a gamble. And don’t get me started on the ‘polypill’ nonsense-no one in real medicine wants to mix aspirin, a statin, and a beta-blocker in one tablet. Too many drug interactions. Too many contraindications. This is lazy medicine dressed up as innovation.
Also, ‘$10 pills’? Sure, if you’re on Medicaid or have a coupon. Try paying cash at a pharmacy in rural Alabama. You’ll be shocked. This whole post reads like a pharma ad. Wake up.
Nathan King
February 9, 2026 AT 18:35While the empirical evidence supporting fixed-dose combinations is indeed compelling, one must not overlook the epistemological limitations inherent in pharmacoeconomic generalizations. The conflation of cost-reduction with therapeutic efficacy is a fallacy frequently propagated by policy-oriented discourse. The FDA’s bioequivalence thresholds, while statistically defensible, do not account for inter-individual variability in cytochrome P450 metabolism, which can significantly alter drug disposition in elderly or polypharmacological populations.
Moreover, the assertion that ‘one pill is better than four’ presumes homogeneity in patient behavior-an assumption contradicted by behavioral economics literature on adherence. The reduction in pill burden does not necessarily translate into improved cognitive retention of therapeutic regimens. One must also consider the pharmacodynamic synergy (or antagonism) of co-formulated agents, which may not be adequately modeled in short-term RCTs.
In sum: while the pragmatic utility of FDCs is undeniable, their universal application requires a more nuanced, patient-centered framework than the article suggests.
Harriot Rockey
February 11, 2026 AT 03:09Y’all need to stop overthinking this. 💙 I was terrified to switch from my brand-name meds to generics-worried I’d feel weird or something would go wrong. But my pharmacist sat down with me, showed me the studies, and even called my doc to suggest a combo. I switched to atorvastatin/amlodipine and I’ve never felt better. No more pill chaos. No more $200 copays. Just… calm. 😌
If you’re on multiple heart meds, don’t wait. Ask. Ask again. Ask your pharmacist even if your doctor doesn’t bring it up. They know. They see this every day. And if you feel off after switching? Tell them. Don’t just suffer through it. Your body talks-you just have to listen.
You’re not alone. We’ve all been there. But this? This is the easy win. 💪❤️
rahulkumar maurya
February 13, 2026 AT 00:27Let’s be brutally honest: the entire ‘combination pill’ movement is a corporate ploy disguised as patient empowerment. Who benefits? Big Pharma, of course. By patenting combinations of off-patent drugs, they extend monopolies under the guise of ‘innovation.’ The FDA’s approval process for FDCs is a backdoor to market exclusivity. And let’s not forget: the ‘polypill’ failed in the U.S. because no one wanted to fund the massive trials needed. So instead, we get two-drug combos that are just repackaged generics with a 300% markup.
Meanwhile, patients are led to believe they’re saving money-when in reality, they’re being funneled into a system where the only ‘win’ is corporate profit margins. And don’t get me started on the ‘pharmacist knows best’ narrative. They’re just following formulary mandates, not advocating for you.
This isn’t medicine. It’s capitalism with a stethoscope.
Demetria Morris
February 13, 2026 AT 04:15I’ve been on heart meds for 12 years. I used to take five pills. Now I take two. I didn’t ask for a combo. My doctor suggested it. I was scared. I thought generics were ‘lesser.’ But I did my research. Read the FDA guidelines. Talked to my pharmacist. And guess what? I feel better. My BP is lower. My cholesterol is stable. I didn’t need magic. I just needed information.
But I still worry. I still read every side effect. I still wonder if I’m being used. Maybe I’m wrong. Maybe I’m paranoid. But I’m not going to stop asking questions. That’s my right. And if you’re scared too? You’re not crazy. You’re just careful.
Geri Rogers
February 15, 2026 AT 00:11Okay, I’m done with the silence. 🙊 If you’re on multiple heart meds and you’re NOT asking about combination generics, you’re leaving money on the table-and risking your health. I’ve helped 17 people switch this year. One lady saved $1,800 a year. Another went from 6 pills to 2. She cried. Not because she was sad-because she finally felt in control.
Stop waiting for your doctor to bring it up. Walk into the pharmacy with your bottle list. Say: ‘Is there a combo for this?’ If they say no, ask again. Then ask for the pharmacist. If they still say no? Find another pharmacy. Seriously. This isn’t optional. It’s basic healthcare literacy.
And if you’re scared? So was I. But I read the studies. I talked to the experts. And now I’m not scared-I’m angry. Why aren’t we doing this for everyone? 💥
Susheel Sharma
February 16, 2026 AT 17:46The so-called ‘cost savings’ narrative is a statistical illusion. Yes, the per-pill cost is lower. But when you factor in increased pharmacy visits, refill delays, and the hidden cost of non-adherence due to patient mistrust of generics, the net benefit evaporates. The 15-20% adherence increase? Correlation ≠ causation. It’s likely driven by patient education campaigns, not the pill itself.
Also, let’s address the elephant in the room: many of these combos are formulated with fillers that trigger autoimmune responses in susceptible individuals. The FDA’s ‘80-125%’ window ignores bioavailability variance in GI disorders. And don’t even get me started on the lack of long-term safety data for multi-drug co-formulations.
This isn’t progress. It’s a pharmacological shortcut. And we’re all the guinea pigs.
Janice Williams
February 17, 2026 AT 15:29How dare you suggest that a combination pill is a solution? This is the epitome of medical reductionism. Human physiology is not a vending machine. You cannot compress complex, individualized therapeutic regimens into a single tablet and expect optimal outcomes. The notion that ‘fewer pills = better adherence’ is a gross oversimplification perpetuated by marketing departments with no clinical experience.
Furthermore, the FDA’s bioequivalence standards are a joke. A 45% variance in drug absorption is not ‘safe’-it’s a gamble with life. And the idea that generics are ‘just as good’ ignores decades of clinical observation where patients experienced adverse events post-switch-events that were dismissed as ‘psychosomatic’.
This post is dangerous. It preys on vulnerability under the guise of empowerment. Shame on you.
Roshan Gudhe
February 18, 2026 AT 07:30I’ve spent years thinking about this-not just as a patient, but as someone who’s watched his father die from a preventable heart event because he couldn’t keep track of his meds. The combination pill isn’t magic. But it’s a gesture. A quiet one. A human one.
It says: ‘We see you. You’re juggling too much. We’re trying to make it easier.’
I don’t care if it’s a corporate strategy. I don’t care if the filler is different. What matters is that a 72-year-old widow in rural Ohio can now take her heart meds without a pillbox, without a chart, without the guilt of forgetting.
Maybe it’s not perfect. Maybe it’s not science fiction. But sometimes, the most revolutionary thing isn’t a breakthrough-it’s a single pill that lets someone live a little longer, a little more peacefully.
That’s worth something.
Rachel Kipps
February 19, 2026 AT 13:54Prajwal Manjunath Shanthappa
February 20, 2026 AT 19:51While the author presents a compelling case for fixed-dose combinations, the omission of pharmacokinetic variability across ethnic subpopulations is a glaring oversight. The FDA’s bioequivalence criteria, derived primarily from Caucasian cohorts, are not generalizable to South Asian or African-descended populations, where CYP2D6 and CYP3A4 polymorphisms significantly alter drug metabolism. Furthermore, the assertion that ‘generics are equally effective’ ignores documented cases of differential efficacy in patients with renal impairment-where excipient-induced tubular toxicity has been observed with hydrochlorothiazide-containing generics.
Moreover, the ‘$10 pill’ narrative is misleading: while cash prices may be low, formulary restrictions, prior authorization delays, and step therapy protocols often render these savings inaccessible to the uninsured or underinsured. The real issue is not pill burden-it’s systemic inequity in access to care.
This is not a triumph of medicine. It is a band-aid on a hemorrhage.
Keith Harris
February 21, 2026 AT 02:43Oh, so now we’re all supposed to believe the pharmacist is our personal doctor? You think they’re going to look up every possible combo? They’re paid to fill scripts, not redesign treatment plans. And if you think switching to a combo pill is risk-free, you’ve never seen someone go from stable to syncope because their new generic had a different coating that altered dissolution rates. This isn’t healthcare. It’s a gamble with your heart.