When you start getting winded climbing stairs, or feel your heart pounding for no clear reason, it’s easy to blame it on being out of shape. But if that shortness of breath keeps getting worse-especially if you’re not active, don’t smoke, and have no asthma-something deeper might be going on. For many people, the real culprit is pulmonary hypertension, a serious condition where blood pressure in the lungs rises so high it starts to damage the heart. Left untreated, it doesn’t just make you tired; it can lead to right heart failure. The good news? We know more now than ever about how to spot it early and treat it effectively.
What Pulmonary Hypertension Really Means
Pulmonary hypertension (PH) isn’t just high blood pressure in the lungs. It’s when the arteries carrying blood from your heart to your lungs become stiff, narrow, or blocked. That forces the right side of your heart to work harder to push blood through. Over time, that extra strain thickens the heart muscle, stretches the chamber, and weakens its ability to pump. The result? A failing right ventricle.
PH isn’t one disease. It’s grouped into five types based on cause. Group 1 is pulmonary arterial hypertension (PAH)-a rare form where the small lung arteries themselves are damaged. Group 2 comes from left heart disease, like heart failure or leaky valves. Group 3 is tied to lung diseases like COPD or pulmonary fibrosis. Group 4 is caused by old blood clots that never cleared. Group 5 includes rare causes like blood disorders or metabolic diseases. Each group needs a different approach, which is why getting the right diagnosis matters more than ever.
Red Flags: Symptoms You Can’t Ignore
Early symptoms of PH are sneaky. They look like normal aging, stress, or being out of shape. But there are patterns. Progressive shortness of breath during light activity-like walking to the mailbox or getting dressed-is the biggest red flag. It’s not just being tired. It’s feeling like you can’t catch your breath even when you’re resting.
Other signs include swelling in the ankles, legs, or abdomen. You might notice your neck veins bulging when you sit up. A racing heartbeat, dizziness, or fainting spells-especially during activity-are serious warnings. Some people feel a sharp chest pain, like their heart is being squeezed. And a loud second heart sound (S2), which doctors hear with a stethoscope, often signals the pulmonary artery is under too much pressure.
Here’s what patients say: “My doctor said I was just anxious. I was walking 300 meters in six minutes and thought that was normal-until I saw my PH specialist and found out I’d lost 40% of my lung capacity in two years.” That delay is common. On average, people wait nearly three years before getting the right diagnosis. Many are first told they have asthma or COPD. But if your lung function tests are normal and you’re still gasping for air, PH needs to be ruled out.
How Right Heart Strain Shows Up on Tests
Right heart strain isn’t something you feel directly-it shows up in measurements. The gold standard for diagnosis is right heart catheterization. This procedure measures the pressure inside your pulmonary arteries directly. The current diagnostic cutoff is a mean pulmonary arterial pressure greater than 20 mmHg at rest. That changed in 2022; it used to be 25 mmHg. This small shift means more people are being diagnosed earlier.
Before catheterization, doctors use echocardiograms. These ultrasound scans of the heart can estimate pulmonary pressure by looking at blood flow speed. If the estimated pressure is above 35-40 mmHg, PH is suspected. But echocardiograms aren’t perfect. They can overestimate pressure by 10-15 mmHg and miss up to 44% of cases. That’s why catheterization is still required for confirmation.
On an echo, right heart strain shows up in three key ways: the right ventricle wall thickens beyond 5 mm, the chamber expands beyond 22 cm², and the tricuspid annular plane systolic excursion (TAPSE) drops below 17 mm. TAPSE measures how far the heart’s valve moves with each beat. If it’s low, the right ventricle isn’t pumping well. Another sign is a right ventricular ejection fraction (RVEF) under 45%. These numbers aren’t just academic-they predict survival. A TAPSE under 15 mm means your risk of death within a year doubles.
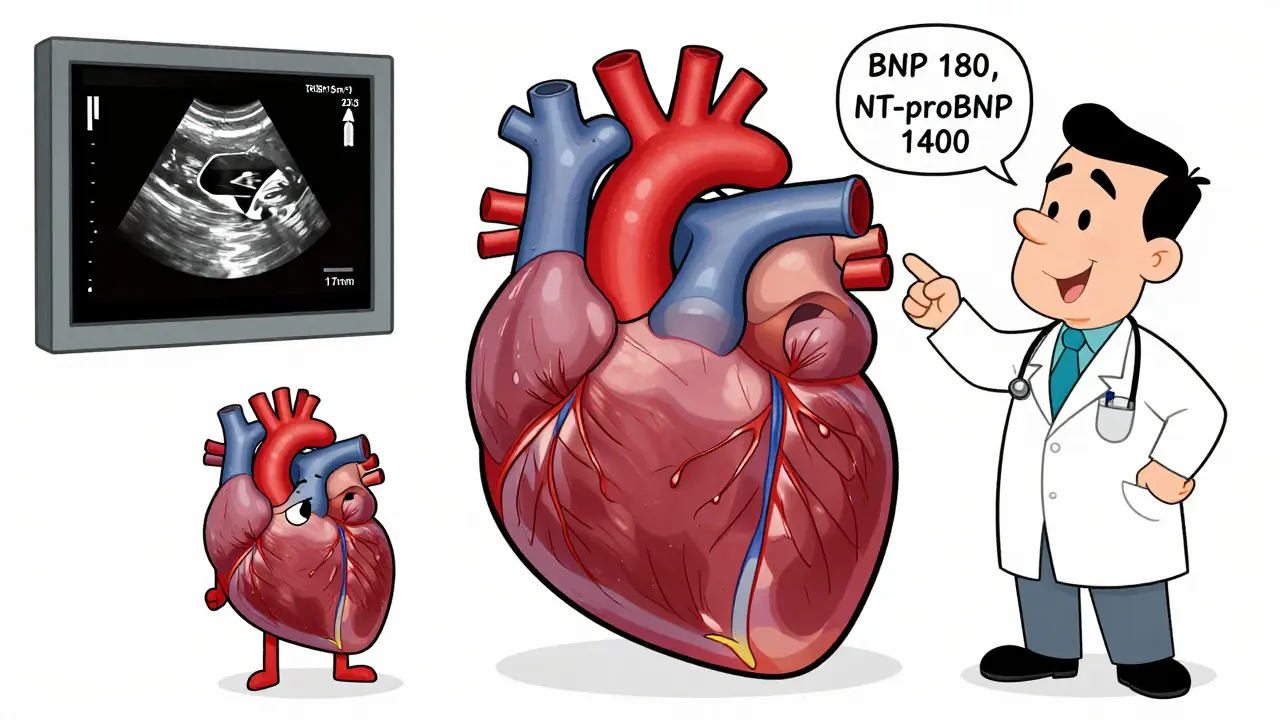
Biomarkers help too. BNP levels above 180 pg/mL or NT-proBNP above 1,400 pg/mL signal severe strain. These proteins leak from the heart when it’s stretched. High levels mean the right side is under heavy stress. A 6-minute walk test is also critical. Walking less than 380 meters predicts a worse outcome. One study showed people who walked under 300 meters had more than twice the risk of death compared to those who walked farther.
Modern Therapy: It’s Not Just One Drug Anymore
Twenty years ago, PH treatment was limited. Most patients got one drug, and survival was under three years. Today, combination therapy is standard. The goal isn’t just to ease symptoms-it’s to slow or even reverse damage to the heart and lungs.
There are now 14 FDA-approved drugs for PH, grouped into five classes. They work in different ways: some relax lung arteries (like endothelin receptor antagonists), others boost natural vasodilators (like phosphodiesterase-5 inhibitors), and some mimic prostacyclin, a powerful artery-opening molecule. Prostacyclin analogs-given through IV, inhalation, or under the skin-are often used in advanced cases.
The biggest breakthrough came in 2021 with sotatercept. It’s the first therapy that targets the root cause of vessel damage in PAH, not just the symptoms. In the STELLAR trial, it cut the risk of death or clinical worsening by 44%. Patients saw improved exercise capacity and lower pulmonary pressure within months. It’s now being used for moderate to severe PAH, often alongside other drugs.
Most patients with PAH now get two or three drugs from different classes right away. A 2023 REVEAL Registry study showed 68% of PAH patients are on combination therapy at diagnosis-up from under 20% in 2010. This shift has pushed 5-year survival rates to 61.8%. That’s not a cure, but it’s a massive improvement.
Why Specialized Care Makes All the Difference
PH is too complex for general doctors to manage alone. Patients treated at specialized PH centers live longer and are hospitalized less. These centers have teams: pulmonologists, cardiologists, pharmacists, nurses, and social workers who know the drugs, the tests, and the pitfalls.
For example, a PH nurse coordinator can catch early signs of decline before you feel worse. They track your walk distance, BNP levels, and echo results over time. One study found patients with coordinated care had 27% fewer hospital visits. These centers also handle complex treatments like IV prostacyclin, which requires central lines and 24/7 infusion pumps. Getting this wrong can mean infection, pump failure, or overdose.
And access matters. In the U.S., only 35 centers treat 75% of PH patients. Many people wait months to get in. Insurance often delays approval for expensive drugs-sometimes over 30 days. That’s dangerous. Every week without the right medication lets the heart weaken further.
There’s also a big equity gap. A 2023 report found minority patients wait 47% longer for diagnosis and have 32% higher death rates. This isn’t about biology-it’s about access. Primary care providers need better training to recognize the red flags: unexplained breathlessness, right heart changes on EKG, and swelling without heart failure.
What’s Next: New Tools and Hope on the Horizon
Research is moving fast. The LIBERTY trial is testing let-7 microRNA as a blood biomarker to detect right heart strain before symptoms appear. That could mean catching PH before the heart is damaged. Other studies are looking at dichloroacetate, a drug that helps the heart use energy more efficiently. Early results show improved right ventricular function in Phase 2 trials.
Diagnostic criteria are evolving too. The lower pressure threshold (20 mmHg) means more people are being diagnosed earlier. But it also means more people need monitoring. The REVEAL 2.0 risk score now uses 19 factors-like your walk distance, BNP level, and functional class-to predict your one-year survival with 85% accuracy. That helps doctors decide who needs aggressive therapy and who can be monitored.
The future isn’t just about better drugs. It’s about earlier detection, better tools, and fairer access. If you’ve been told you’re just “out of shape” but still struggle to breathe, push for a referral. Ask for an echocardiogram. If your doctor says no, ask why. Your heart is trying to tell you something.
Can pulmonary hypertension be cured?
There is no cure for pulmonary hypertension yet, but modern therapies can significantly slow its progression and improve quality of life. Some patients, especially those with chronic thromboembolic PH (Group 4), may be cured with surgery to remove old blood clots. For others, combination drug therapy can stabilize the condition for years. Early diagnosis and treatment at a specialized center are the best ways to extend survival and reduce complications.
How is pulmonary hypertension different from regular high blood pressure?
Regular high blood pressure (hypertension) affects the arteries throughout the body and is measured in the arm. Pulmonary hypertension specifically raises pressure in the arteries that carry blood from the right side of the heart to the lungs. It doesn’t show up on a standard blood pressure cuff. The heart strain, symptoms, and treatments are completely different. You can have normal arm blood pressure and still have severe pulmonary hypertension.
Can exercise help with pulmonary hypertension?
Yes-under supervision. Studies show that carefully monitored, low-to-moderate aerobic exercise like walking or cycling improves walking distance, heart function, and quality of life in PH patients. But intense exercise or heavy lifting can be dangerous. Always work with a PH specialist or cardiac rehab team. They’ll design a safe program based on your 6-minute walk test results and heart function.
What happens if pulmonary hypertension is left untreated?
Untreated pulmonary hypertension leads to progressive right heart failure. The right ventricle thickens, then stretches and weakens until it can’t pump enough blood to the lungs. This causes fluid buildup in the abdomen and legs, severe shortness of breath even at rest, irregular heart rhythms, and eventually, death. Median survival without treatment was under three years in the 1980s. Today, early treatment can extend life by decades.
Are there any lifestyle changes that help manage pulmonary hypertension?
Yes. Avoid smoking and secondhand smoke-both damage lung arteries. Stay away from high altitudes, where oxygen is lower and pressure rises. Get vaccinated for flu and pneumonia to avoid lung infections. Avoid pregnancy-it’s extremely dangerous with PH. Maintain a healthy weight and eat a low-salt diet to reduce fluid retention. Emotional stress and extreme heat can worsen symptoms, so manage them carefully. Always take your medications exactly as prescribed.
How do I know if my treatment is working?
Your care team tracks several markers. If your 6-minute walk distance increases, your BNP or NT-proBNP levels drop, your right heart function improves on echo, and you feel less tired and short of breath, your treatment is working. Regular follow-ups every 3-6 months are essential. If your symptoms worsen or your walk distance drops, your therapy may need adjustment. Don’t wait until you’re struggling to speak-call your PH clinic early.
What to Do Next
If you’ve been told you have asthma or COPD but your symptoms don’t match your lung tests-if you’re still out of breath, swollen, or dizzy-ask for a referral to a pulmonary hypertension specialist. Request an echocardiogram. If your doctor refuses, ask for a second opinion. Time is critical. The earlier you’re diagnosed, the more treatment options you have, and the better your chances of living a full, active life.
 Methimazole Allergy: Symptoms and Management
Methimazole Allergy: Symptoms and Management
 Methoxsalen and Collagen Production: What It Does to Your Skin
Methoxsalen and Collagen Production: What It Does to Your Skin
 Why the First Generic Filer Gets 180 Days of Market Exclusivity
Why the First Generic Filer Gets 180 Days of Market Exclusivity
 How to Buy Online Cheap Generic Claritin Safely in Australia
How to Buy Online Cheap Generic Claritin Safely in Australia
Laia Freeman
January 28, 2026 AT 18:19Andy Steenberge
January 29, 2026 AT 02:27Laura Arnal
January 30, 2026 AT 13:53rajaneesh s rajan
February 1, 2026 AT 09:21paul walker
February 3, 2026 AT 03:27Kristie Horst
February 3, 2026 AT 16:44Jasneet Minhas
February 3, 2026 AT 23:31Eli In
February 5, 2026 AT 21:13Megan Brooks
February 7, 2026 AT 16:40