Every year, Australians fill over 270 million prescriptions. Nearly 84% of those are for generic drugs - cheaper versions of brand-name medicines. But how does Australia make these drugs so affordable? The answer lies in the Pharmaceutical Benefits Scheme (PBS), a government program that doesn’t just help people pay for medicine - it reshapes the entire market.
What the PBS Actually Does
The PBS isn’t just a subsidy. It’s a pricing engine. Since 1948, it’s been the backbone of Australia’s medicine access system. The government pays about 90% of the cost for over 5,400 listed medicines. Patients pay the rest - $7.70 if you have a concession card, $31.60 if you don’t. But here’s the catch: that $31.60 hasn’t gone up since July 2024, even though inflation would’ve pushed it to $32.80. That’s because the government froze the price in 2025 to save people money. Starting January 1, 2026, it drops again - to $25. This isn’t charity. It’s strategy. The PBS uses its buying power to force drug companies to lower prices. If a medicine isn’t listed on the PBS, most Australians simply won’t buy it. That gives the government massive leverage. And it works. Generic drugs in Australia cost 30-40% less than in the U.S., according to OECD data.How the PBS Controls Prices
The real magic happens behind the scenes. The Pharmaceutical Benefits Advisory Committee (PBAC) decides what gets listed. They don’t just look at whether a drug works. They ask: Is it worth the cost? Their benchmark? Around $50,000 per quality-adjusted life year (QALY). That’s the cost to extend someone’s life by one year with good health. If a drug costs more than that, it’s unlikely to be approved - unless it’s for a rare disease. That’s where the Highly Specialised Drugs Program (HSDP) comes in. It’s a backdoor for ultra-expensive treatments for conditions like rare cancers or genetic disorders. But even then, there are eight strict criteria. Many patients wait years for approval. Then there’s reference pricing. Since 2007, the PBS groups similar drugs together - say, all statins for cholesterol. The government picks the cheapest one as the “reference price.” If you choose a more expensive version, you pay the difference out of pocket. This forces pharmacies and patients toward generics. The result? 84% of prescriptions by volume are generic. That’s higher than the OECD average.Who Benefits - and Who Gets Left Behind
On paper, the PBS looks perfect. But reality is messier. Concession card holders - pensioners, disability recipients, low-income families - pay $7.70 per script. They rarely skip doses. But general patients? That $31.60 adds up fast. Five medications? $158 a month. For retirees without a card, that’s more than some pay for rent. The Australian Bureau of Statistics found 1.8 million people skipped doses or didn’t fill prescriptions in 2024 because of cost. The safety net helps. Once you spend $1,571.70 on PBS scripts in a year, your co-payment drops to $7.70 - even if you’re not on a concession card. But hitting that threshold takes time. People with chronic illnesses like diabetes or heart disease hit it. People with occasional prescriptions? They don’t. A 2025 report by the Australian Council of Social Service found 28% of low-income households with multiple chronic conditions cut back on food to afford medicine. One Reddit user in Perth wrote: “I’m choosing between insulin and groceries. The PBS helps, but not enough.”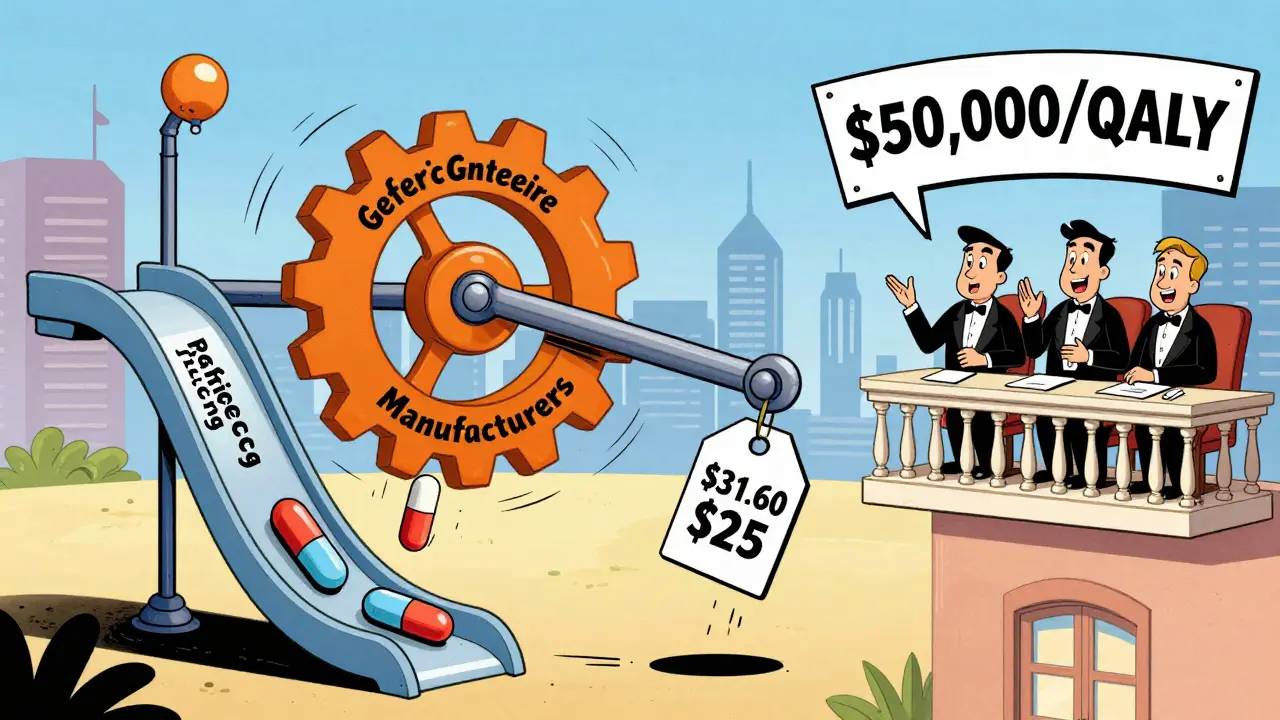
How Generics Dominate the Market
Australia’s generic drug market hit $6.2 billion in 2024. That’s 46% of total PBS spending. But here’s the twist: generics make up 84% of prescriptions by volume, but only 22% of spending. Why? Because they’re cheap - really cheap. The Generic Medicines Pricing Framework, introduced in 2020, forced prices down hard. After six months, the PBS sets the reference price at 60% of the original brand’s price. After a year? Down to 43%. When multiple generics enter the market, prices crash. In cardiovascular drugs, prices drop 74% within a year of generic launch. The top five generic makers - Symbion, Sigma, Mylan, Aspen, and Hospira - control nearly 70% of the market. They’re not just copying drugs. They’re racing to be the cheapest. And the PBS rewards them for it. But not all drugs are created equal. Biologics - complex, injectable medicines for things like rheumatoid arthritis or cancer - are harder to copy. Even after patents expire, generics (called biosimilars) take years to get listed. Only 63% of biologic prescriptions are generic, compared to 95% for statins.The Slow Rollout Problem
The PBS is great at cutting prices. But it’s slow to add new drugs. A drug approved by the Therapeutic Goods Administration (TGA) - Australia’s drug safety regulator - can sit for 14.2 months before it’s listed on the PBS. That’s over a year where patients pay full price. One study found people wait an average of $1,850 out-of-pocket during that gap. Compare that to Germany or Canada. They list new medicines in half the time. Australia’s median time from global launch to PBS listing? 587 days. That’s almost two years. For someone with a rare disease, that delay can be deadly. The 2024 Senate Inquiry into Orphan Drug Access led to changes. Starting November 1, 2025, the HSDP will relax two of its eight criteria. That’s a small win. But the system still moves like molasses.
What’s Changing in 2025 and Beyond
The government is trying to fix the gaps. The National Health Amendment (Cheaper Medicines) Bill 2025 is the biggest shift in a decade. It cuts the general co-payment to $25 in January 2026. That’s a $784 million saving for patients over four years - but it costs the government $689 million more. It’s a trade-off: less pain for patients, more pressure on the budget. Budget 2025-26 added $1.2 billion for new PBS listings. Drugs like Talazoparib (for prostate cancer) and Relugolix (for endometriosis) are now covered. That means 150,000 more Australians get access. The Department of Health is also rolling out AI tools to flag inappropriate prescriptions. In 2024, the Auditor-General found $1.2 billion in PBS spending was potentially wasteful - duplicate scripts, unnecessary antibiotics, drugs with no proven benefit. AI could cut that. The future? PBS spending will hit $18.7 billion by 2029-30. Why? More older Australians. More expensive cancer drugs. More biologics. The system is under strain.What This Means for You
If you’re on a concession card: you’re in the best position. Your co-payment is low. Use 60-day scripts to save even more. If you’re a general patient: track your spending. Use the PBS app. Know when you’re approaching the safety net. Ask your pharmacist: “Is there a cheaper generic?” If you’re a prescriber: the authority-required listings are a nightmare. 43% of GPs say they waste hours filling out forms. Use the online PBS Tools portal. Submit electronically. Paper takes over a week. If you’re a patient with a rare disease: don’t give up. The HSDP is changing. Talk to your specialist. Ask about the new criteria. Advocate. The system is slow, but it’s not broken.Final Thoughts
The PBS isn’t perfect. It’s bureaucratic. It’s slow. It leaves some people behind. But it’s also one of the most effective public health systems in the world. It saves Australians billions every year. It keeps generics cheap. It stops drug companies from overcharging. The real question isn’t whether the PBS works. It’s whether we’re willing to pay - in taxes, in time, in patience - to keep it that way.How much do Australians pay for PBS medicines in 2025?
As of July 2024, general patients pay $31.60 per prescription, and concession card holders pay $7.70. These amounts were frozen in 2025 to prevent inflation increases. Starting January 1, 2026, the general co-payment will drop to $25.00 under the new Cheaper Medicines Bill.
What is the PBS safety net and how does it work?
The PBS safety net is a cap on out-of-pocket costs. Once a general patient spends $1,571.70 on PBS medicines in a calendar year, their co-payment drops to $7.70 for the rest of the year - even if they don’t have a concession card. Concession card holders already pay $7.70, so their safety net is triggered after spending $1,571.70, after which they pay nothing extra.
Why are generic medicines so much cheaper in Australia than in the U.S.?
Australia’s PBS negotiates drug prices directly with manufacturers and uses reference pricing - grouping similar drugs and paying only for the cheapest one. This creates intense competition among generics. In the U.S., drug prices are set by private insurers and pharmaceutical companies with no government price controls, leading to significantly higher costs.
How long does it take for a new drug to be listed on the PBS?
On average, it takes 587 days from a drug’s global launch to PBS listing in Australia. After a drug is approved by the Therapeutic Goods Administration (TGA), it can take up to 14.2 months to be added to the PBS, during which patients pay full price. This is much slower than countries like Germany or Canada.
What percentage of prescriptions in Australia are for generic medicines?
As of 2025, 84% of all prescriptions dispensed in Australia are for generic medicines by volume. However, because generics are so much cheaper, they account for only 22% of total PBS spending. The PBS’s reference pricing system drives this high adoption rate.
Who qualifies for PBS subsidies in Australia?
All Australian citizens and permanent residents with a Medicare card qualify. Overseas visitors from 11 countries with reciprocal health agreements - including the UK, New Zealand, Sweden, and Belgium - also qualify. Approximately 26.5 million people are covered under the PBS as of 2025.

 Compare Atorlip 5 (Atorvastatin) with Alternatives: What Works Best for Cholesterol
Compare Atorlip 5 (Atorvastatin) with Alternatives: What Works Best for Cholesterol
 Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
 How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
 Syphilis Global Health Impact - Worldwide Perspective
Syphilis Global Health Impact - Worldwide Perspective
 Buy Generic Prilosec (Omeprazole) Online in Australia: Cheap, Safe Options for 2025
Buy Generic Prilosec (Omeprazole) Online in Australia: Cheap, Safe Options for 2025
Brady K.
January 1, 2026 AT 07:37The PBS is basically a state-sponsored price cartel disguised as social welfare. You think you’re getting a deal? Nah. You’re just getting the government’s version of ‘take it or leave it’ - and the drug companies know it. They’re not losing money; they’re just playing the long game, knowing the PBS will eventually cave and list their drug at 43% of original price after a year. It’s not healthcare reform - it’s corporate coercion with a Medicare card.
Kayla Kliphardt
January 2, 2026 AT 09:03I’m curious how this system affects people who need biologics but can’t afford the out-of-pocket costs before they’re listed. It’s one thing to save on statins, but when you’re waiting 18 months for a life-changing drug… that’s not efficiency, that’s a waiting game with someone’s health on the line.
John Chapman
January 2, 2026 AT 17:5184% generics?! YES!! 🙌 Australia’s doing it right. Meanwhile in the US, I’m paying $400 for a pill that costs $3 here. The PBS is a masterclass in how to use collective power to crush corporate greed. More countries need to copy this. 💪💊 #HealthcareForThePeople
Emma Hooper
January 3, 2026 AT 10:04Let’s be real - this whole system is built on the backs of people who can’t afford to be sick. $31.60 might sound like pocket change until you’re choosing between insulin and your kid’s school lunch. And don’t even get me started on the safety net - it’s like a finish line you have to sprint to before you get any mercy. The government’s not helping the poor - they’re just making sure the poor don’t die *too* fast.
Robb Rice
January 3, 2026 AT 17:48While the PBS model is commendable in theory, its implementation suffers from structural delays that undermine its efficacy. The median 587-day lag between global approval and PBS listing represents a significant therapeutic gap, particularly for patients with progressive conditions. Furthermore, the administrative burden on prescribers, as noted in the 43% GP survey data, introduces inefficiencies that offset cost savings. A more agile, technology-integrated approval pipeline is urgently required.
Retha Dungga
January 5, 2026 AT 12:08you know what’s wild? they make you pay 31 bucks then suddenly drop it to 25 like its no big deal but what about all the people who died waiting? the system moves like a snail on sedatives and we call it progress? 🤷♀️💊
Jenny Salmingo
January 6, 2026 AT 09:47I love how Australia makes medicine affordable without turning it into a profit war. I wish my country could do this. People shouldn’t have to choose between medicine and food. Simple. Human. Right.
Lawver Stanton
January 6, 2026 AT 13:46Let me tell you something - this PBS thing sounds great on paper until you’re the one sitting in a doctor’s office with a prescription in your hand and no way to pay for it. I’ve got diabetes. Five scripts a month. That’s $158. That’s more than my internet bill. That’s half my rent. And you want me to be grateful because the government’s gonna drop it to $25 in 2026? What about 2025? What about now? My neighbor died last year because she skipped her heart meds to pay for groceries. And now you’re giving me a PowerPoint slide on reference pricing? Nah. This isn’t policy. This is cruelty with a spreadsheet.
Sara Stinnett
January 7, 2026 AT 19:19Oh, so now the government gets to play God with medicine? ‘Is it worth $50k per QALY?’ Who the hell are you to decide whose life is worth extending? This isn’t healthcare - it’s actuarial eugenics wrapped in a Medicare card. And don’t pretend the safety net is a solution. It’s a trap. You have to spend $1,571.70 before you get relief? That’s not compassion - that’s a financial hazing ritual. The PBS doesn’t make medicine affordable. It just makes the poor suffer more quietly.