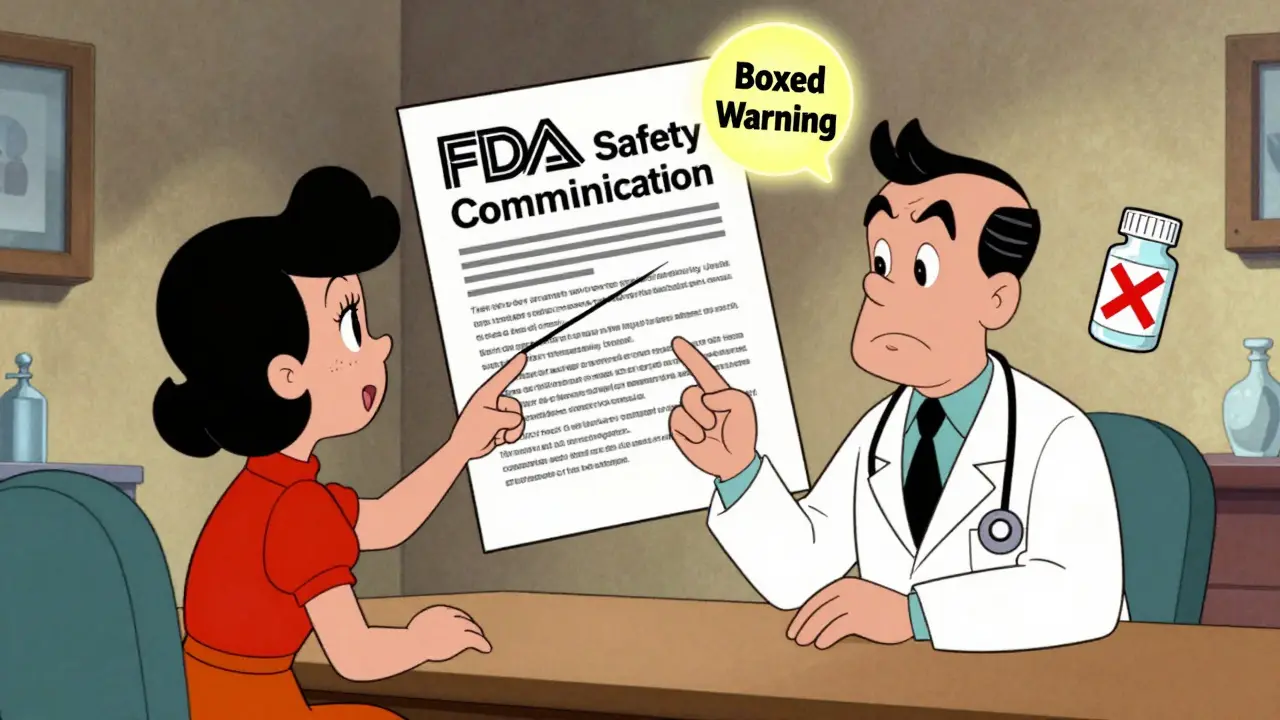
Every year, the U.S. Food and Drug Administration (FDA) issues dozens of FDA Safety Communications-official notices that tell you when a medication you’re taking might have new risks. These aren’t ads. They’re not press releases. They’re legal, science-backed updates that can change how your doctor prescribes your drug-or whether you should keep taking it at all. But if you’ve ever opened one and felt lost, you’re not alone. The language is dense, the structure is technical, and the stakes are high. Here’s how to actually read them, what to look for, and what to do next.
What FDA Safety Communications Actually Are
FDA Safety Communications are not warnings about contaminated batches or manufacturing errors. Those are recalls. These are updates about how a drug affects your body after it’s been on the market for years. Think of it this way: when a drug is approved, the FDA has data from clinical trials. But those trials involve thousands of people-not millions. Once a drug is used by millions, rare side effects, dangerous interactions, or long-term risks start to show up. That’s when the FDA steps in.
Since 2007, the FDA has had legal power to require updates to drug labels based on real-world use. These updates are published as Drug Safety Communications. In 2023 alone, the FDA issued 62 major communications. Many of them changed how doctors prescribe opioids, blood thinners, or diabetes drugs. Some led to boxed warnings-the strongest warning the FDA can issue.
The Structure: What Each Communication Contains
Every FDA Safety Communication follows the same format. You don’t need to read every word. Here’s what matters:
- What Safety Concern Is FDA Announcing? This is the headline. It tells you the core issue-like "increased risk of severe liver injury" or "dangerous interaction with grapefruit juice." Read this first. If it doesn’t apply to your drug, you can stop.
- Highlights of Prescribing Information This section summarizes the biggest changes. It’s written in plain language and often includes bold text for new warnings. Look for the phrase "Boxed Warning"-that’s the FDA’s highest alert level. If your drug has one, pay close attention.
- Section Former Labeling Language Changes This is where it gets technical. The FDA shows you exactly what was changed in the official prescribing label. Old text is struck through. New text is bolded and underlined. For example: "Do not abruptly discontinue" becomes "Do not rapidly reduce or abruptly discontinue." This tells you the exact wording doctors must now use.
- For Health Care Professionals This section gives clinical guidance: when to test, when to stop, what alternatives exist. It’s meant for doctors, but if you’re a patient who reads medical literature, this is gold.
- For Patients This is the part you need. It tells you what to do. It might say: "Talk to your doctor before stopping your medication," or "Read the Medication Guide every time you get a refill." It’s written at an 8th-grade reading level by law.
What to Look For: The Four Critical Red Flags
Not every change matters to you. But four things should make you pause:
- Boxed Warning Updates This is the FDA’s strongest warning. It appears at the top of the drug’s prescribing information. If this changes, it means a serious risk-like heart failure, liver damage, or death-has been confirmed. If your drug has a boxed warning, you should discuss it with your doctor.
- Changes to Dosage or Administration If the FDA says "Do not take more than 50 mg daily" or "Must be taken with food," that’s not optional. These changes are based on real patient data showing harm at higher doses or on an empty stomach.
- New Contraindications This means you should not take the drug at all under certain conditions. For example: "Do not use if you have severe kidney disease" or "Avoid if you are pregnant." If this applies to you, your doctor needs to know.
- Class-Wide Changes Sometimes, the FDA updates safety info for an entire class of drugs. For instance, if all opioid painkillers get a new warning about addiction risk, then your specific brand is affected too. Check the communication for phrases like "all drugs in this class" or "all opioid analgesics."
How to Use This Information
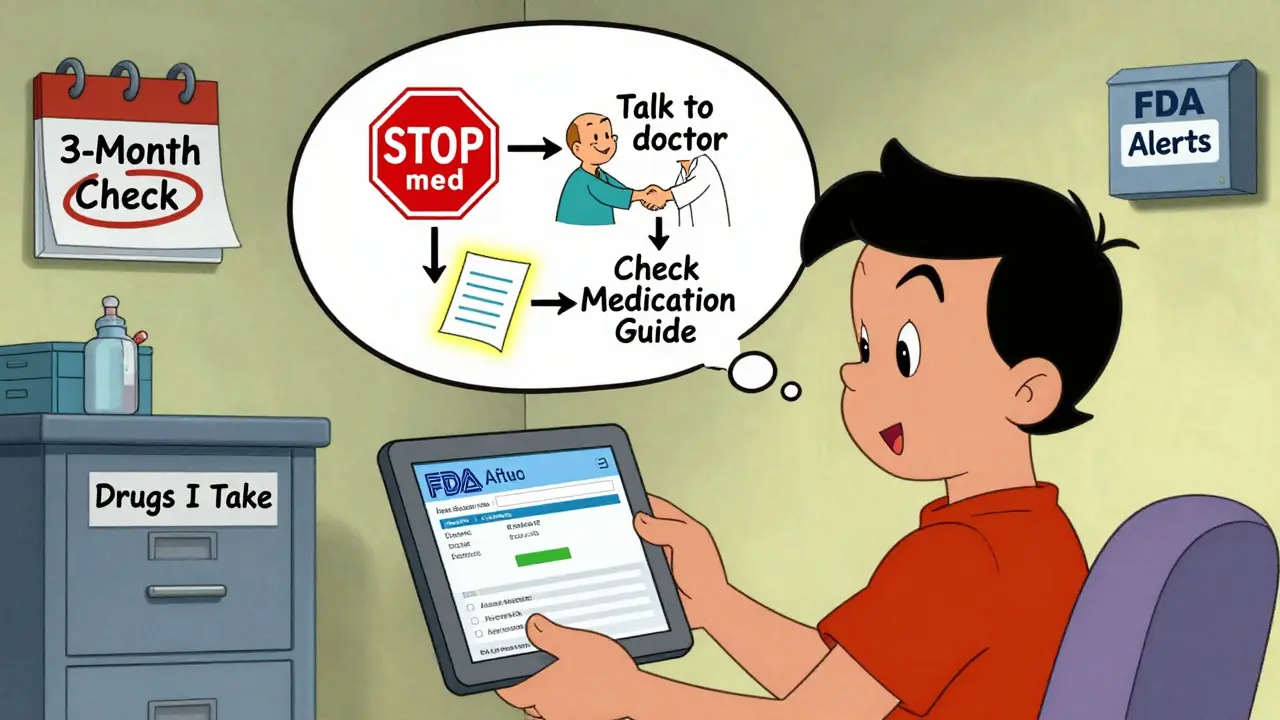
Don’t panic. Don’t stop your medication on your own. Here’s what to do:
- Check your drug’s name Make sure the communication applies to the exact brand or generic you take. Sometimes, only one version of a drug is affected.
- Find the Medication Guide Every prescription comes with a Medication Guide. It’s a small paper insert. The FDA requires it to explain risks in simple language. If the safety communication mentions it, read it again. It’s updated when new risks are found.
- Write down your questions Before your next appointment, write: "Did my drug get a new safety warning?" and "Should I change how I take it?" Bring the communication with you-or just the drug name and date of the alert.
- Sign up for email alerts Go to fda.gov/drugs/drug-safety-and-availability and sign up for alerts by drug class. You can choose to get updates only for your medications, like "anticoagulants" or "SSRIs."
What Doesn’t Matter
Not every change is urgent. The FDA issues communications for many reasons:
- Some are informational-just letting you know a risk exists, but not changing how you take the drug.
- Some are about rare side effects seen in only 1 in 10,000 patients.
- Some are about how the drug should be stored-not how it affects your body.
If the communication says "Consider this information when prescribing," that’s not a command. It’s a note. But if it says "STOP using this medication immediately," that’s different. Look for action words.
Why These Warnings Take So Long
You might wonder: Why does it take years for the FDA to act? The answer is science. Drug companies report side effects. Doctors report them. Patients report them. The FDA collects thousands of reports every year. But to confirm a real risk, they need to rule out coincidence. Was the liver injury caused by the drug-or by alcohol? By another medication? By an undiagnosed condition?
Studies show it takes an average of 4.2 years from the first safety signal to a major labeling change. That’s frustrating. But rushing to change a label without solid evidence can cause more harm. The FDA waits until the evidence is strong enough to act.
What’s Changing in 2025 and Beyond
The FDA is making efforts to improve how these warnings reach you:
- Plain-language summaries are now available for high-risk drugs.
- Some alerts are being translated into Spanish.
- By 2025, the FDA plans to send personalized safety alerts directly through patient portals linked to your electronic health record.
- They’re testing visual aids-charts, icons, and color-coded risk levels-to make the information easier to understand.
But until then, the best tool you have is your own awareness. If you take medication, check your prescriptions. Know your drug’s name. Keep the Medication Guide. And talk to your doctor-not Google.
Are FDA Safety Communications the same as drug recalls?
No. A drug recall means the product is contaminated, mislabeled, or defective and should be removed from shelves. FDA Safety Communications are about new safety risks discovered after the drug has been used by millions of people. You don’t need to return your pills, but you may need to change how you take them.
Can I stop my medication if I see a safety alert?
Never stop a medication without talking to your doctor first. Some safety alerts warn about risks that only happen if you stop suddenly-like seizures from stopping antidepressants too fast. The FDA will always say "Do not stop without consulting your doctor" if that’s the case. If the alert says "STOP immediately," then act right away. But those are rare.
Do I need to read every FDA Safety Communication?
No. Only pay attention to alerts for drugs you’re currently taking. You can sign up for email alerts from the FDA filtered by drug class-like "antidepressants" or "blood pressure meds." That way, you only get updates that matter to you.
What if my doctor hasn’t mentioned a safety alert?
Doctors get hundreds of updates each month. Some miss them. If you see a safety alert for your drug, bring it to your next appointment. Say: "I read this alert and wanted to make sure we’re still on the same page." Most doctors will appreciate you being informed.
Where can I find the full prescribing information?
Go to Drugs@FDA ([email protected]) and search for your drug’s brand or generic name. The full prescribing information includes every warning, dosage, and interaction. The FDA Safety Communication will reference specific sections like "2.x" or "5.x"-those numbers point you directly to the right part of the full document.
Next Steps for Patients
- Find the Medication Guide for every prescription you take. Keep it in a folder.
- Set a calendar reminder to check for new FDA alerts every three months.
- Ask your pharmacist if your drug has had any recent safety updates.
- Sign up for FDA email alerts at fda.gov/drugs/drug-safety-and-availability.
The goal isn’t to scare you. It’s to give you power. You’re not just a patient-you’re a partner in your care. Knowing how to read these alerts means you’re no longer waiting for someone else to tell you what’s happening. You’re reading it yourself.
 Why Generic Drug Prices Vary So Much Between States
Why Generic Drug Prices Vary So Much Between States
 Where and How to Buy Calan Online Safely: Everything You Need to Know
Where and How to Buy Calan Online Safely: Everything You Need to Know
 How Clavulanic Acid Revolutionizes Antibiotic Treatments for Resistant Infections
How Clavulanic Acid Revolutionizes Antibiotic Treatments for Resistant Infections
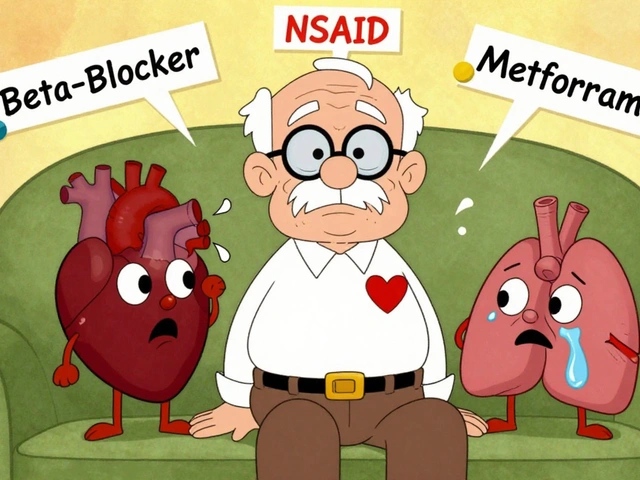 Drug-Disease Interactions: How Your Health Conditions Can Change How Medications Work
Drug-Disease Interactions: How Your Health Conditions Can Change How Medications Work
 Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
Cardiovascular Combination Generics: What Works, What Doesn’t, and What You Can Save
Neha Motiwala
February 13, 2026 AT 18:39athmaja biju
February 14, 2026 AT 06:42Robert Petersen
February 16, 2026 AT 00:01alex clo
February 17, 2026 AT 00:41Alyssa Williams
February 18, 2026 AT 23:34Ernie Simsek
February 19, 2026 AT 20:07Joanne Tan
February 20, 2026 AT 09:28Jack Havard
February 21, 2026 AT 17:24