Medication Formulation Side Effect Comparison
How Formulation Affects Side Effects
Different medication forms impact how quickly drugs are absorbed and how side effects manifest. This tool helps you understand potential differences between immediate-release and extended-release formulations.
Side Effect Comparison
When to Consider Each Formulation
Immediate-Release (Tablets/Capsules)
Better for:
- Quick symptom relief (e.g., pain, nausea)
- Patients who can take multiple doses daily
- Cost-sensitive situations (often cheaper)
Extended-Release (ER)
Better for:
- Patients with side effects from peak concentrations
- Stable daily dosing needs
- Improved adherence with once-daily dosing
When you pick up a prescription, you might not think twice about whether it’s a tablet, capsule, or extended-release pill. But the form you’re taking can change how your body reacts - not just to the medicine, but to the side effects too. It’s not just about what’s inside. It’s about how it’s built.
Tablets vs Capsules: Speed, Stability, and What You Feel
Tablets are pressed powders held together by binders. They’re cheap to make, stable for years, and often the go-to for long-term meds. But they take longer to break down. In your stomach, a standard tablet usually dissolves in 30 to 60 minutes. That means the drug starts working in about 1 to 2 hours. Capsules, on the other hand, are shells filled with powder or liquid. They dissolve faster - often in under 20 minutes. That’s why you might feel the effects sooner with a capsule. Studies show capsules can absorb 20-30% faster than tablets. That’s useful if you need quick relief, like with painkillers or anti-nausea meds. But speed comes with trade-offs. Capsules are more sensitive to heat and moisture. Their shelf life is usually 1 to 2 years shorter than tablets. If you live in a humid place like Perth, that matters. A tablet sitting in your bathroom cabinet might still be good after two years. A capsule? Not so much. Side effects? They’re often tied to how fast the drug hits your bloodstream. Faster absorption = higher peak concentration = more chance of nausea, dizziness, or jitteriness. That’s why people on immediate-release capsules often report more side effects than those on extended-release tablets.Extended-Release: How It Works and Why It Matters
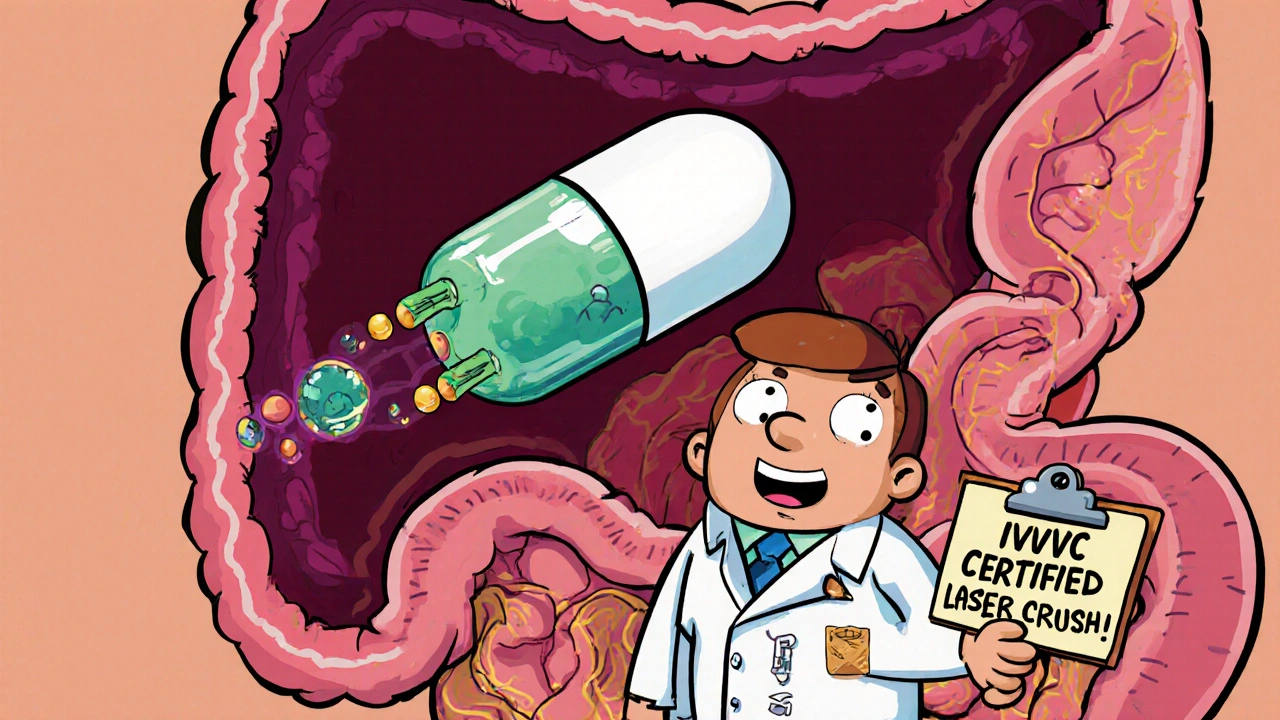
Extended-release (ER), also called sustained-release (SR) or extended-duration (XR/XL), is designed to let the drug leak out slowly over 12 to 24 hours. Think of it like a water bottle with a tiny hole - drip, drip, drip - instead of dumping the whole thing at once. There are four main ways this happens:- Hydrophilic matrix: The pill swells in your stomach, forming a gel that slows drug release. HPMC (hydroxypropyl methylcellulose) is the most common material, making up 20-60% of the tablet.
- Hydrophobic matrix: Uses waxy or insoluble polymers like ethylcellulose to trap the drug and control how fast it escapes.
- Reservoir systems: The drug is sealed inside a membrane, like a tiny capsule inside a pill. The membrane controls the flow.
- Osmotic systems: Uses pressure to push the drug out through a laser-drilled hole. These are the most precise - and the most expensive.
Side Effects: Why Formulation Changes Everything
Side effects aren’t random. They’re often tied to concentration spikes. When a drug hits your blood too fast, your brain and gut react. That’s why immediate-release stimulants cause jitteriness. Why SSRIs make you nauseous at first. Why some people can’t tolerate the immediate-release version of their epilepsy drug. A review of 15 studies on antiepileptic drugs found that immediate-release versions caused 25-40% more concentration-related side effects than extended-release ones. That’s not just a preference - it’s a clinical reality. But ER isn’t magic. It has its own risks.- Dose dumping: If the coating fails - maybe because you took it with a high-fat meal - the whole dose can flood your system at once. That’s dangerous with opioids or heart meds.
- Food effects: About 15% of ER drugs behave differently when taken with food. A fatty meal can make the drug release 20-35% faster. That’s why some ER pills say “take on an empty stomach.”
- Swallowing issues: ER tablets are often bigger. Elderly patients or those with swallowing problems struggle. One Mayo Clinic survey found 27% of negative reviews mentioned this.
- Can’t split or crush: Breaking an ER tablet can destroy the slow-release mechanism. You might as well be taking a bomb.
Real People, Real Experiences
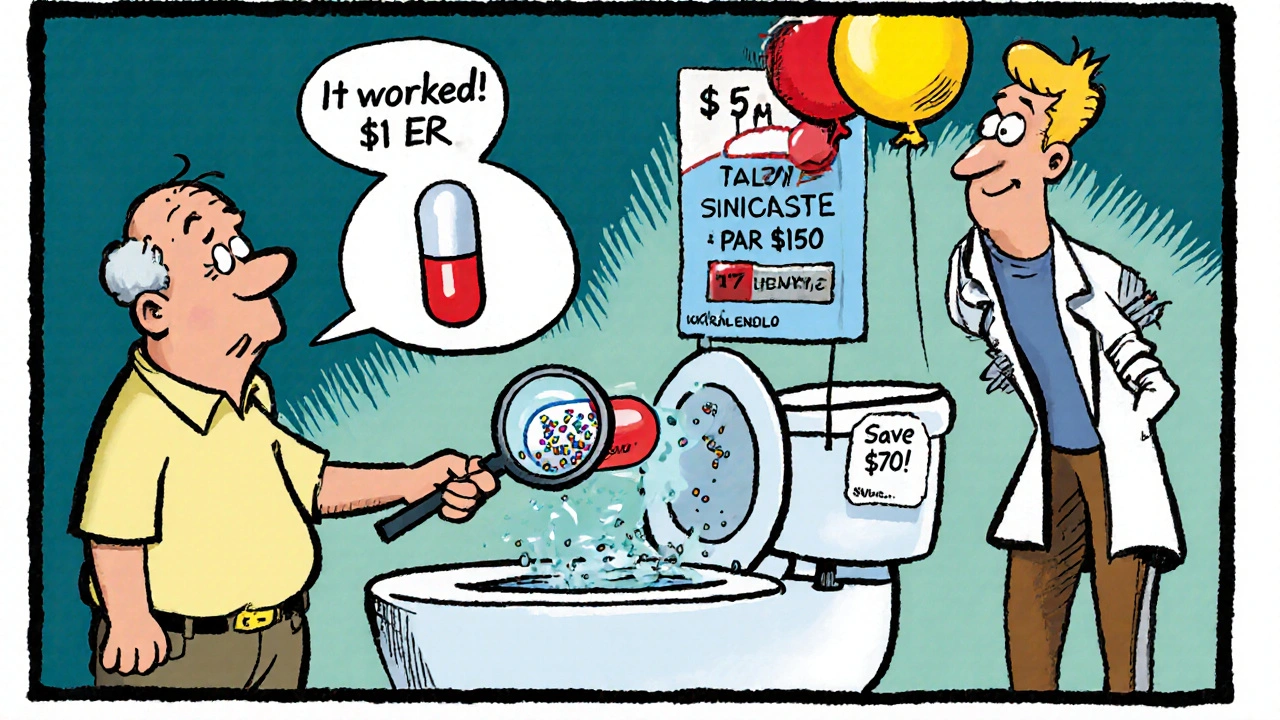
On Drugs.com, extended-release meds average 4.2 out of 5 stars. Immediate-release? 3.8. Why? People love fewer pills. One user wrote: “I used to take my antidepressant three times a day. Now I take one pill in the morning. My life changed.” But cost is a big barrier. A 30-day supply of generic immediate-release bupropion costs about $15. The ER version? $185. That’s 12 times more. For people on fixed incomes, that’s not an option. Even with insurance, co-pays for ER versions can be $50+. One case study from UPM Pharmaceuticals tracked a bipolar patient who went from 65% adherence on three-times-daily meds to 92% on once-daily quetiapine ER. Over 12 months, their mood episodes dropped by 47%. That’s not just compliance - it’s stability. But not everyone wins. Some users report “ghost pills” - the empty shell of the ER tablet passing through their system intact. That happens in 5-10% of people, especially those with slow gut motility. It’s not a defect. It’s how the system works. But if you see a whole pill in the toilet, don’t assume it didn’t work. It probably did.What Doctors Need to Know
Prescribing ER meds isn’t just about picking the right drug. It’s about understanding the delivery system.- Titration is harder: Most ER pills come in fixed doses. You can’t split them. So if you need to go from 150mg to 175mg, you’re stuck - unless you switch brands or use multiple pills.
- Missed doses are different: With some ER meds like Trokendi XR, you can take the missed dose up to 24 hours later. With immediate-release? You’re out of luck.
- Labeling matters: Confusing SR with ER with DR (delayed-release) leads to errors. A 2021 study found 12% of medication errors involved misreading these labels.
What’s Next? The Future of Drug Delivery
The next wave of ER tech is smarter. Rytary, approved in 2023, releases carbidopa-levodopa in three pulses - mimicking the natural rhythm of dopamine in Parkinson’s patients. It cuts “off” time by over two hours a day. Gastric-retentive systems are in trials - pills that float in your stomach for 24 hours. pH-sensitive coatings are being developed to release drugs only in the colon. That could revolutionize treatments for IBD or Crohn’s. By 2030, nearly half of all oral pills will be extended-release, according to IQVIA. Aging populations want fewer pills. Chronic disease management needs steady levels. The trend is clear. But we can’t ignore the downside. Polymer coatings from ER pills are showing up in wastewater. A 2022 study found them in 78% of samples tested. That’s a hidden environmental cost.What Should You Do?
If you’re on a medication with side effects, ask: Is the form part of the problem?- Are you nauseous after taking your pill? Try switching to an ER version - if available.
- Do you forget doses? ER might help you stick with it.
- Do you have trouble swallowing? Talk to your pharmacist about liquid alternatives or smaller pills.
- Is cost a barrier? Ask about generic immediate-release options. Sometimes the savings outweigh the side effects.
Can I crush an extended-release tablet if I can’t swallow it?
No. Crushing an extended-release tablet destroys the slow-release mechanism. You could end up taking the full dose all at once, which can be dangerous - especially with opioids, stimulants, or heart medications. If swallowing is a problem, ask your doctor or pharmacist about liquid forms, sprinkle capsules, or smaller immediate-release options.
Why do some extended-release pills come out whole in my stool?
It’s normal. The outer shell of many ER pills is designed to pass through your system intact after releasing the drug. You’re not seeing the medicine - you’re seeing the empty carrier. That doesn’t mean it didn’t work. If you’re concerned, check your blood levels with your doctor or ask for a different formulation.
Are extended-release medications more expensive?
Yes, often significantly. Generic immediate-release versions can cost as little as $15 for a month’s supply. The ER version of the same drug might cost $150-$200. Insurance often covers both, but co-pays can be much higher for ER. If cost is an issue, ask your doctor if a generic immediate-release version is safe and effective for you.
Can food affect how extended-release pills work?
Yes. About 15% of extended-release drugs are affected by food - especially high-fat meals. A fatty meal can speed up drug release by 20-35%, leading to unexpected side effects or reduced effectiveness. Always check the label: if it says “take on an empty stomach,” follow it. If unsure, ask your pharmacist.
Do extended-release medications have fewer side effects?
Generally, yes - especially for side effects tied to high peak drug levels, like nausea, dizziness, or jitteriness. Studies show extended-release versions of antidepressants, antiepileptics, and ADHD meds reduce these side effects by 18-40% compared to immediate-release. But they’re not side-effect-free. Some people experience constipation, dry mouth, or delayed onset of action.
What’s the difference between SR, ER, XR, and XL?
SR (sustained-release), ER (extended-release), XR (extended-release), and XL (extended-release, extended duration) are mostly used interchangeably. They all mean the drug is released slowly over time. DR (delayed-release) is different - it means the pill doesn’t dissolve until it reaches the intestine, like enteric-coated aspirin. Always check the drug name and dosage instructions - the suffix matters.
If you’re managing a chronic condition, the form of your medication isn’t just a detail - it’s a tool. Choosing the right one can mean the difference between feeling okay and feeling like you’re fighting your own body. Talk to your pharmacist. Ask questions. Your health depends on it.
 When to Call 911 vs Contact Your Doctor About Medication Reactions
When to Call 911 vs Contact Your Doctor About Medication Reactions
 Fall Risk Medications for Seniors: Which Drugs Increase Injury Risk?
Fall Risk Medications for Seniors: Which Drugs Increase Injury Risk?
 How to Manage Interactions When Starting a New Medication
How to Manage Interactions When Starting a New Medication
 How Medications Enter Breast Milk and What It Means for Your Baby
How Medications Enter Breast Milk and What It Means for Your Baby
Andrew Baggley
November 18, 2025 AT 16:03Man, I never realized how much the pill form actually mattered until I switched from immediate-release Wellbutrin to the XL version. My anxiety spiked so bad I thought I was having a panic attack every morning. Turned out it was just the drug hitting me like a freight train. Now I take one pill at breakfast and I’m fine. No jitteriness, no nausea, just steady vibes. Seriously, if you’re struggling with side effects, ask your doc about ER options - it’s not just placebo, it’s pharmacology.
Also, don’t let cost scare you off. Generic ERs are getting cheaper every year. I got mine for $40 with a coupon. Worth every penny.
Frank Dahlmeyer
November 20, 2025 AT 02:07Let me tell you something - this whole discussion about formulation is one of the most underappreciated topics in modern medicine. We’re so obsessed with the active ingredient that we forget the delivery system is literally the difference between healing and suffering. Think about it: two pills with identical chemistry, but one dissolves in 20 minutes and the other in 12 hours. One makes you feel like a nervous wreck, the other lets you sleep, work, laugh, live. That’s not science - that’s art. And the companies that design these systems? They’re unsung heroes. HPMC matrices, osmotic pumps, hydrophobic barriers - these aren’t just buzzwords. They’re lifelines. I’ve seen patients go from suicidal to stable just by switching from a tablet to an XR capsule. The system matters. The form matters. The timing matters. And if your doctor doesn’t get that, find a new one.
Also, the ghost pill thing? Totally normal. I used to freak out every time I saw a whole capsule in the toilet. Turns out it’s just the shell. Like a snake shedding its skin. The medicine’s already gone. Your gut’s just doing its job.
Reema Al-Zaheri
November 21, 2025 AT 06:26While the article presents a compelling overview of pharmaceutical formulations, it is imperative to note that the clinical data cited - particularly the 22% reduction in dizziness and 18% reduction in nausea with extended-release venlafaxine - must be contextualized within the parameters of the original studies. The sample sizes, control groups, and duration of observation are not referenced here, which limits the generalizability of the conclusions. Furthermore, the environmental impact of polymer coatings in wastewater, while mentioned, requires further citation of peer-reviewed environmental toxicology studies to substantiate the claim of 78% detection rates. Without these, the argument risks becoming anecdotal rather than evidence-based. Finally, the distinction between SR, ER, XR, and XL is correctly noted as largely interchangeable; however, regulatory agencies such as the FDA and EMA have specific definitions for each, and prescribers must adhere to these distinctions to avoid therapeutic missteps.
Andrew Montandon
November 21, 2025 AT 19:37Hey everyone - if you’ve ever taken an ER pill and seen the shell in the toilet, don’t panic. I used to think my meds weren’t working, so I’d double up. Bad idea. Turns out, it’s just the shell. The drug’s already out. I learned this from my pharmacist after a panic attack over a ‘whole pill’ in the bowl.
Also, if you’re on a tight budget, ask for the generic immediate-release version. It’s not always the enemy. For some people, the side effects are manageable, and the cost savings let them afford food, rent, therapy - stuff that matters more than a fancy coating. Don’t let marketing scare you into spending $185 a month when $15 does the job. Talk to your pharmacist. They’re not just there to hand out pills. They’re your secret weapon.
Sam Reicks
November 22, 2025 AT 18:55Chuck Coffer
November 24, 2025 AT 04:10So you’re telling me the reason I can’t sleep, feel dizzy, or gag every morning is because my pill is too fast? Not because I’m just a weak, sensitive person? Interesting. I guess my body’s just not cut out for modern medicine. Maybe I should’ve been born in 1950 with aspirin and a prayer.
Also, ghost pills? That’s the excuse they give when the drug doesn’t work? Cool. So I’m supposed to trust a shell? That’s not science. That’s magic. And I don’t believe in magic. I believe in cash registers.
Marjorie Antoniou
November 25, 2025 AT 20:57I’m so glad someone finally wrote this. I’ve been telling my friends for years: it’s not just the drug, it’s the delivery. My sister was on immediate-release lamotrigine and couldn’t leave the house because of the dizziness. Switched to XR - now she teaches yoga. No joke.
And to the person who said crushing ER pills is dangerous - YES. Please don’t do it. I’ve seen people do it because they can’t swallow, then end up in the ER. It’s not worth it. Ask for liquid, ask for sprinkle capsules, ask for anything else. There are options. You’re not broken. The pill just doesn’t fit your body - and that’s okay. Talk to your pharmacist. They’ll help.
Codie Wagers
November 26, 2025 AT 05:00There’s a deeper truth here, one that escapes most of the clinical chatter: the entire pharmaceutical model is predicated on control - control of release, control of perception, control of compliance. We are conditioned to believe that a pill must be swallowed whole, that time is linear, that our bodies are machines to be calibrated. But what if the body doesn’t want to be controlled? What if the ghost pill is not a failure of the drug, but a whisper from our gut saying, ‘I don’t need your slow drip. I need my rhythm.’
Perhaps the real side effect isn’t nausea or dizziness - it’s the surrender of autonomy to a system that profits from our dependence. We don’t just take pills. We perform rituals for capitalism. And the coating? It’s not just polymer. It’s a metaphor.
Paige Lund
November 27, 2025 AT 23:05