For women with polycystic ovary syndrome (PCOS), losing weight isn’t just about looking different-it’s about resetting your hormones, getting your period back, and lowering your risk of type 2 diabetes. But traditional treatments like metformin often fall short. That’s where GLP-1 receptor agonists come in. These drugs, originally designed for diabetes, are now showing powerful results for PCOS, especially in women carrying extra weight.
What GLP-1s Actually Do in the Body
GLP-1s-like liraglutide and semaglutide-mimic a natural hormone made in your gut after eating. This hormone tells your pancreas to release insulin only when blood sugar is high, slows down how fast food leaves your stomach, and sends a clear signal to your brain: you’re full. That’s why people on these drugs eat less without feeling constantly hungry.
It’s not just about appetite. GLP-1 receptors are also found in fat tissue, the liver, and even the ovaries. This means these drugs don’t just help you lose weight-they improve insulin sensitivity, lower testosterone levels, and reduce inflammation. In PCOS, where insulin resistance drives excess androgen production, that’s a game-changer.
How Much Weight Can You Really Lose?
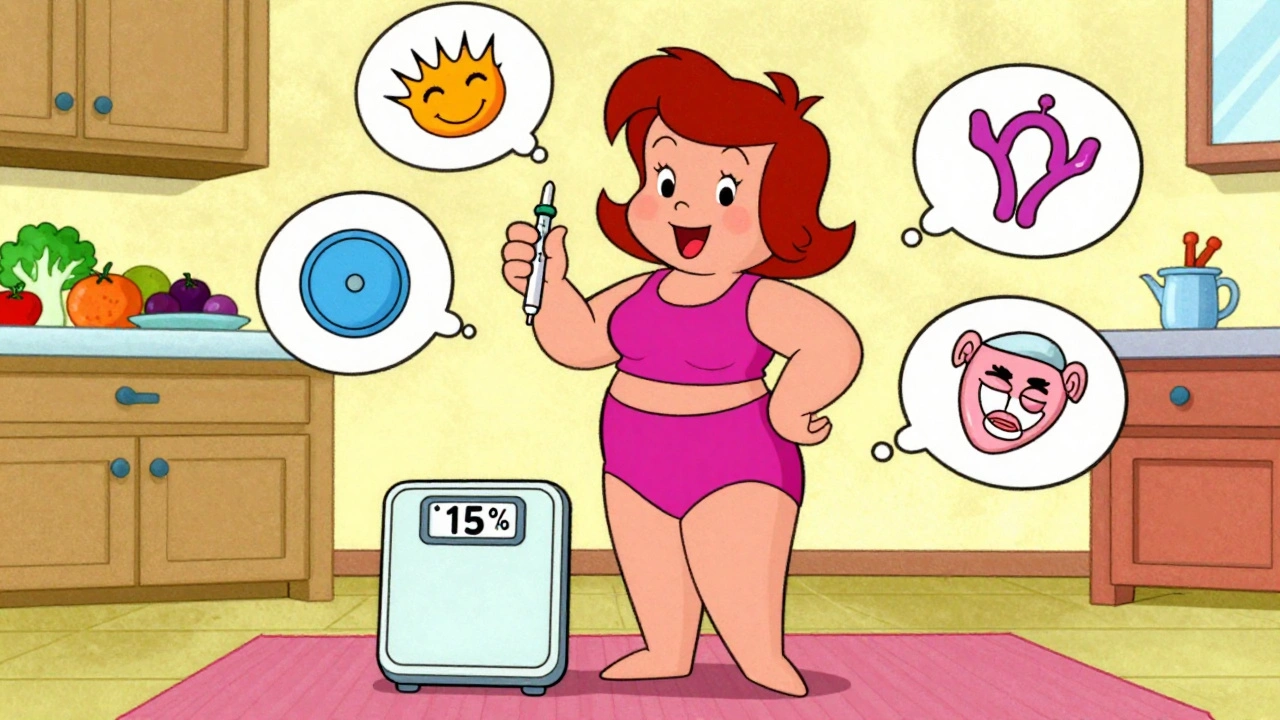
Studies show clear, measurable results. In one trial, women with PCOS using semaglutide (2.4 mg weekly) lost an average of 5.6% of their body weight in just 12 weeks. Another study tracking patients for 68 weeks found weight loss of nearly 15%-that’s over 30 pounds for someone weighing 200 pounds.
Compare that to metformin, the old standard. Metformin might help you lose 2-5% of your weight, but GLP-1s consistently hit 5-10%. And it’s not just the scale. Visceral fat-the dangerous fat around your organs-drops by up to 18%. That’s the kind of change that reduces your risk of heart disease and diabetes long-term.
Why GLP-1s Beat Metformin for PCOS
Metformin helps with insulin resistance, but it doesn’t do much for appetite. Many women stay hungry, keep snacking, and struggle to lose weight. GLP-1s change that. In direct comparisons, liraglutide led to 3-6% more weight loss than metformin in PCOS patients. Semaglutide? Even more.
But it’s not just about pounds. In one study, 42% of women on liraglutide started ovulating spontaneously after 6 months. Their testosterone levels dropped by an average of 25%. Their periods became regular. Their cholesterol improved. These aren’t side effects-they’re core benefits of fixing the metabolic root of PCOS.
Who Benefits the Most-and Who Doesn’t
GLP-1s work best for women with PCOS who also have a BMI over 30 and signs of insulin resistance: high fasting glucose, dark skin patches (acanthosis nigricans), or fatty liver. If you’re lean with PCOS and your hormones are off but your metabolism is fine, these drugs won’t help much.
And they’re not magic. You still need to eat well. Skipping meals or eating ultra-processed foods while on GLP-1s can make nausea worse. These drugs work best when paired with real food, regular movement, and good sleep.
The Side Effects: What No One Tells You
Nausea is the big one. About 44% of people feel it when they start, especially in the first few weeks. Vomiting happens in 24%, dizziness in 15%. Most people get used to it. But for some, it’s too much. Around 1 in 5 people stop taking the drug because of it.
Other issues include constipation, bloating, and injection site reactions. And yes-they’re expensive. A monthly supply of Wegovy or Saxenda can cost $800-$1,400 in the U.S. That’s 50-100 times more than generic metformin, which runs $10-$20.
There are also safety limits. If you or a close family member had medullary thyroid cancer, you shouldn’t use them. And while they’re safe for most, long-term data beyond 2 years in PCOS patients is still limited.
Real Stories: Success and Struggle
One woman on Reddit wrote: “After 6 months on semaglutide, I lost 28 lbs. My testosterone dropped from 68 to 42. I had my first regular period in 3 years.” That’s the dream.
But another shared: “Spent $1,200 a month on Wegovy. Lost 15 lbs. Couldn’t keep food down. Switched back to metformin.”
These aren’t outliers. Clinical trials show similar splits. The drugs work brilliantly for some. For others, the side effects or cost make them unsustainable.

How to Start and What to Expect
You don’t jump straight to the full dose. Doctors start low-0.25 mg of semaglutide weekly-and slowly increase every 4 weeks. It takes 16-20 weeks to reach the full 2.4 mg dose. This slow ramp-up helps your body adjust and cuts down on nausea.
You inject it yourself once a week, under the skin of your belly, thigh, or arm. It’s a tiny needle. Most people get used to it quickly. You’ll need to monitor your blood sugar if you’re prediabetic. And if you’re already on metformin, many doctors recommend staying on it. One 2024 study found that women who kept metformin after stopping semaglutide regained only one-third of the weight they lost. Those who stopped both? They gained back 60-70%.
The Future: What’s Coming Next
In June 2024, the European Medicines Agency accepted Novo Nordisk’s application to officially approve semaglutide 2.4 mg for PCOS with metabolic complications. A final decision is expected in early 2025. That could change everything-making insurance coverage more likely and giving doctors confidence to prescribe it.
Oral versions like Rybelsus are already available for diabetes, and if they get approved for obesity, adherence could improve dramatically. New drugs like retatrutide, which hits three receptors at once, are in trials and may offer even stronger weight loss.
By 2027, experts predict GLP-1s will become standard care for obese PCOS patients. But cost and access will be the biggest barriers. Right now, they’re a tool for those who can afford them-and who are ready to stick with them long-term.
Is It Right for You?
If you have PCOS, are overweight, and have tried diet and metformin without lasting results, GLP-1s might be worth discussing. But ask these questions first:
- Do I have insulin resistance or prediabetes?
- Can I handle potential nausea for the first few months?
- Can I afford this long-term-or does my insurance cover it?
- Am I ready to make lifestyle changes to support the drug’s effects?
They’re not a quick fix. They’re a powerful tool-when used the right way.
Can GLP-1s help with PCOS symptoms like acne and excess hair growth?
Yes. Since GLP-1s lower insulin and testosterone levels, many women see improvements in acne and unwanted hair growth after 4-6 months. The reduction in androgens is a direct result of improved metabolic health, not just weight loss.
How long do you need to take GLP-1s for PCOS?
Most experts recommend staying on them long-term, similar to how people with high blood pressure take medication daily. Stopping often leads to weight regain. The goal isn’t to use them until you reach your target weight-it’s to use them as part of a sustainable management plan.
Are GLP-1s safe if I want to get pregnant?
They’re not approved during pregnancy. If you’re planning to conceive, you’ll need to stop them at least 2 months before trying. But many women successfully get pregnant after losing weight on GLP-1s-often naturally, without fertility drugs.
Do GLP-1s cause muscle loss?
Unlike extreme dieting, GLP-1s don’t typically cause major muscle loss when combined with protein intake and resistance training. Studies show most weight lost is fat, especially visceral fat. Still, staying active and eating enough protein helps preserve muscle.
Can I take GLP-1s with birth control pills?
Yes. There are no known dangerous interactions between GLP-1s and hormonal birth control. In fact, many women with PCOS stay on birth control to manage periods while using GLP-1s for weight and metabolic benefits.
 Boost Your Immunity and Energy with Bee Pollen: Nature's Miracle Dietary Supplement
Boost Your Immunity and Energy with Bee Pollen: Nature's Miracle Dietary Supplement
 How to Buy Cheap Generic Crestor Online Safely
How to Buy Cheap Generic Crestor Online Safely
 The connection between azelastine and throat infections
The connection between azelastine and throat infections
 How Medications Enter Breast Milk and What It Means for Your Baby
How Medications Enter Breast Milk and What It Means for Your Baby
 The science behind cefixime: how it works to fight bacterial infections
The science behind cefixime: how it works to fight bacterial infections
dan koz
December 2, 2025 AT 14:33GLP-1s ain’t magic, but they’re the closest thing we got for PCOS weight loss. I’ve seen patients go from insulin resistant to ovulating on semaglutide. Just don’t expect it to work if you’re still chowing down on donuts.
Katey Korzenietz
December 3, 2025 AT 15:11Ugh another person thinkin’ drugs solve everything. Metformin’s been workin’ for decades. Now we got rich folks payin’ $1000/mo for nausea? Pathetic.
Mindy Bilotta
December 4, 2025 AT 23:59Hey, I’m a nurse who’s helped 12 PCOS patients start GLP-1s. Nausea sucks at first but it fades. One girl lost 40 lbs, got her period back, and stopped needing insulin. It’s not perfect but it’s life-changing for the right person.
Josh Bilskemper
December 6, 2025 AT 17:07Let’s be real-GLP-1s are just a fancy version of calorie restriction with a side of pharmaceutical ego. The real issue is our food system and sedentary lifestyles. You don’t need a $1400 injection to eat less. You need discipline. Or a better job.
Kevin Estrada
December 7, 2025 AT 11:08OMG I JUST GOT MY FIRST WEGOVY PRESCRIPTION AND I’M CRYING. AFTER 12 YEARS OF PCOS I’M LOSING WEIGHT AND MY ACNE IS CLEARING. MY HUSBAND SAID I LOOK LIKE MY 22-YEAR-OLD SELF. THIS IS A MIRACLE. THANK YOU SCIENCE.
Cyndy Gregoria
December 9, 2025 AT 06:07For anyone scared of the side effects: start low, go slow. I went from 0.25mg to 1.7mg over 5 months. Nausea was bad for 2 weeks, then gone. I walk 30 mins a day and eat protein at every meal. It’s not about the drug-it’s about the habits you build around it.
Colin Mitchell
December 9, 2025 AT 09:29My cousin in Nigeria just got access to semaglutide through a clinical trial. She lost 35 lbs, her periods came back, and her family stopped calling her ‘fat’. It’s not just medicine-it’s dignity. We need these drugs to be affordable everywhere, not just in the US.
Susan Haboustak
December 9, 2025 AT 11:45Anyone who says GLP-1s are safe hasn’t read the FDA’s black box warnings. Thyroid cancer risk, pancreatitis, gallbladder disease. And the weight regain after stopping? It’s worse than before. This is a corporate scam disguised as medicine. Big Pharma doesn’t care if you’re healthy-they care if you’re dependent.
Chris Jahmil Ignacio
December 9, 2025 AT 23:49GLP-1s are just the tip of the iceberg. The real agenda? Making women feel broken so they’ll pay for expensive drugs instead of fixing the root causes: endocrine disruptors in plastics, processed food subsidies, and the medical system that ignores metabolic health. They don’t want you cured-they want you subscribed.
Storz Vonderheide
December 10, 2025 AT 13:17I’ve been on liraglutide for 10 months. Lost 22 lbs. My testosterone dropped from 85 to 48. My period’s regular. I still take metformin. I eat clean. I lift weights. I sleep 7 hours. The drug helped me get over the hump-but it didn’t do it alone. If you’re thinking about it, do the work. It’s not a magic pill. It’s a tool. Use it wisely.