Tetracycline Photosensitivity Risk Calculator
This tool estimates your risk of photosensitivity when taking tetracycline antibiotics based on your specific medication, location, and sun exposure habits. Photosensitivity can cause severe sunburns, blistering, and skin discoloration.
Your Medication
Your Location
Your Sun Exposure
Your Personalized Risk Assessment
Select your medication and other inputs to see your personalized risk assessment.
When you’re prescribed tetracycline, doxycycline, or another antibiotic in this class, you’re usually told to take it on an empty stomach and avoid dairy. But there’s another warning that rarely gets mentioned-until you’re standing in the sun with a painful, red burn that shouldn’t have happened in 20 minutes.
Tetracycline photosensitivity isn’t rare. It affects 5 to 10% of people taking these antibiotics, and for some, it’s not just a bad sunburn. It’s blistering skin, discolored nails, and dark patches that stick around for months-even after you stop the drug. In Australia, where UV levels are among the highest in the world, this isn’t just an inconvenience. It’s a real health risk.
What Exactly Is Tetracycline Photosensitivity?
Tetracycline photosensitivity is a phototoxic reaction, not an allergy. That means it’s not your immune system going haywire-it’s the drug itself reacting to sunlight. When UV-A rays (320-425 nm) hit tetracycline molecules in your skin, they trigger a chemical reaction that produces reactive oxygen species. These little troublemakers punch holes in cell membranes, damage DNA, and wreck ribosomal proteins. The result? Your skin turns red, swells, blisters, or peels-even if you’ve never burned before.
This isn’t theoretical. In a 2021 study published in Dermatologic Therapy, researchers tracked over 500 patients on tetracycline antibiotics. Nearly 70% of those who developed photosensitivity ended up with lasting hyperpigmentation-dark spots that lingered long after the rash faded. And it’s not just your face. Your neck, arms, hands, and even the tops of your feet can get hit.
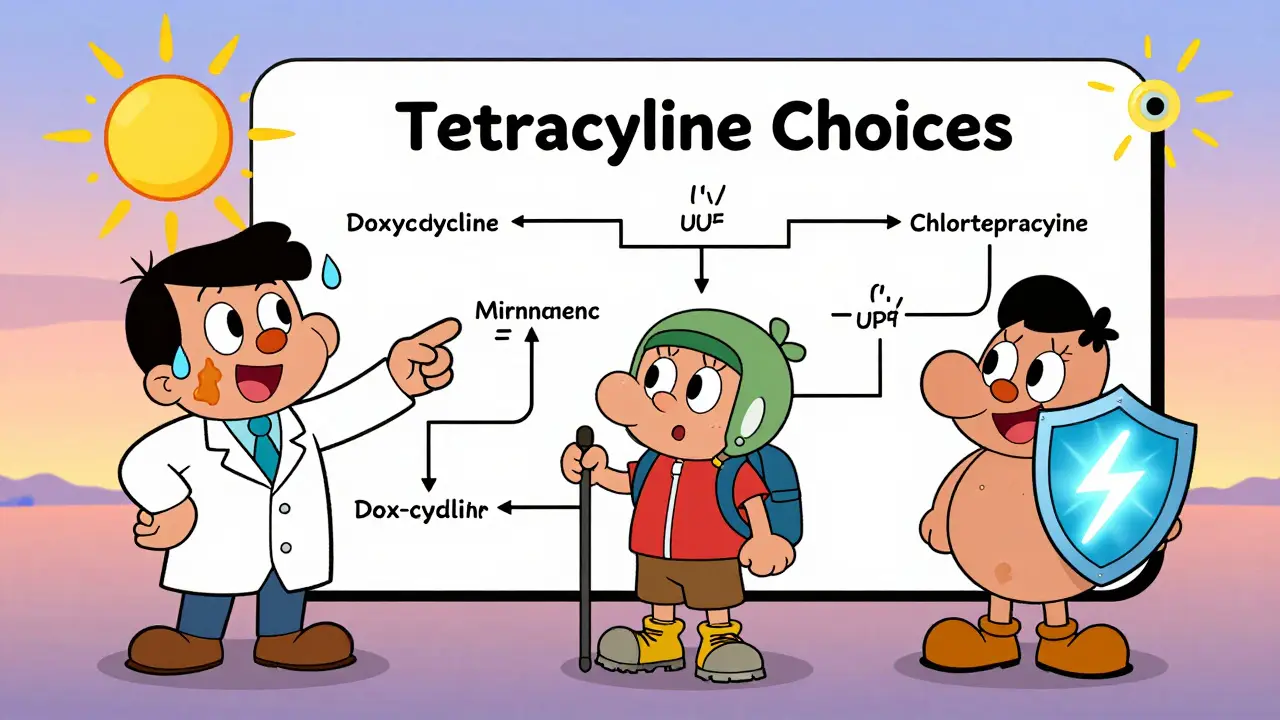
Not All Tetracyclines Are the Same
If you’re on tetracycline for acne, rosacea, or a tick bite, the specific drug you’re taking matters a lot. Here’s the real breakdown:
- Doxycycline: The biggest culprit. At 100 mg twice daily, up to 42% of patients show phototoxic reactions in controlled tests. Even at 100 mg once daily, 15-18% get burned. It’s cheap, effective, and widely prescribed-but it’s also the most likely to turn your skin into a sunburned mess.
- Minocycline: Your safer bet. Only less than 2% of users report photosensitivity. It’s slightly more expensive, but if you’re spending time outdoors, hiking, biking, or just walking the dog, this is the one to ask for.
- Demeclocycline: Less common, but still risky. About 13 out of 31 people in one study reacted to it at high doses.
- Chlortetracycline and tetracycline HCl: Rarely used today, but they showed almost no phototoxicity in older studies.
Here’s why this matters: Your doctor might not know the difference. A 2022 survey by the American Academy of Dermatology found that 68% of patients who had a photosensitivity reaction said their provider never warned them. If you’re being prescribed doxycycline and you live in Perth, work outside, or love weekend beach trips-ask if minocycline is an option.
Nail Damage? Yes, That’s a Thing
Most people don’t expect antibiotics to mess with their nails. But between 15% and 20% of patients on tetracyclines develop photo-onycholysis-where the nail slowly separates from the nail bed. It usually shows up 3 to 6 weeks after starting the drug. The tip of one or more fingernails lifts up, turns white or yellow, and can be painful. It’s not dangerous, but it’s ugly, slow to heal, and often mistaken for a fungal infection.
Then there’s chromonychia-nail discoloration. About 8% of users get white, yellow, or brown streaks across their nails. Again, it’s harmless but startling. One Reddit user, u/SunSensitiveMD, shared that three of their patients developed full nail separation on doxycycline. All had to stop the drug.
And then there’s pseudoporphyria. It’s rare-only 2-4% of cases-but it mimics a serious genetic disorder called porphyria. Your skin becomes fragile. Blisters form from minor bumps or sun exposure. Scars and tiny white bumps (milia) show up on your face, neck, and hands. The difference? Your blood porphyrin levels are normal. But the damage looks real, and recovery takes months.
How to Prevent It-For Real
Here’s what actually works, based on clinical data and patient outcomes:
- Use mineral sunscreen, not chemical. Chemical sunscreens (avobenzone, oxybenzone) don’t block the full UV-A range that triggers tetracycline reactions. You need zinc oxide or titanium dioxide. Look for SPF 50+ with zinc as the first active ingredient. CeraVe Mineral SPF 50 and EltaMD UV Clear are top choices among dermatologists.
- Apply enough. Most people use only 25-30% of the recommended amount. You need 2 mg per cm²-that’s about a shot glass full for your whole body. If you’re using a pump, squeeze out a full line from wrist to elbow.
- Reapply every 2 hours. Sweat, water, and towel-drying remove sunscreen. Even if it’s labeled "water-resistant," you still need to reapply after swimming or heavy sweating.
- Avoid the sun between 10 a.m. and 4 p.m. That’s when UV-A is strongest. Plan walks, errands, and outdoor time for early morning or late afternoon.
- Wear UPF 50+ clothing. A regular cotton T-shirt only blocks about 5-10% of UV. UPF-rated shirts, hats, and sunglasses are game-changers. A wide-brimmed hat cuts UV exposure to your face and neck by 73%.
- Use UV-blocking window film. If you drive a lot, your car windows don’t block UV-A. Installing a clear film that blocks 99% of UV-A can prevent reactions during your daily commute.
One patient in Perth, who took doxycycline for rosacea for six months, reported zero issues-because she wore UPF clothing, applied zinc sunscreen every morning without fail, and never sat outside between 10 a.m. and 4 p.m. She didn’t "try" to avoid the sun. She made it part of her routine.
What If You Already Got Burned?
If you’ve already developed a reaction:
- Stop sun exposure immediately.
- Use cool compresses and fragrance-free moisturizers (like Cetaphil or Vanicream).
- Don’t pop blisters-they increase infection risk.
- See a dermatologist if the burn is severe, blistering, or spreading.
- Ask about switching to minocycline or another antibiotic if you still need treatment.
Hyperpigmentation can last for months. Topical hydroquinone or azelaic acid can help fade it, but prevention is always better than treatment.

Are There Better Alternatives?
If photosensitivity is a dealbreaker, consider these options:
- Minocycline: As mentioned, it’s far less likely to cause reactions. It’s commonly used in dermatology for acne, especially in sunny climates.
- Sarecycline (Seysara): A newer tetracycline derivative designed to be less phototoxic. Studies show only 3.2% photosensitivity rate. But it costs about $550 for a 30-day supply-18 times more than generic doxycycline.
- Omadacycline (Nuzyra): Approved in 2023, it shows only 2.1% phototoxicity in trials. But it’s expensive and typically reserved for more serious infections.
- Non-tetracycline antibiotics: For acne, clindamycin or azithromycin are common alternatives. For Lyme disease or other infections, amoxicillin or cefdinir may work depending on the pathogen.
Don’t assume you have to suffer through sunburns just because your doctor reached for the cheapest option. If you’re active outdoors, your health is worth the extra cost.
Why This Matters in Australia
Australia has the highest rates of skin cancer in the world. The UV index regularly hits 12+ in summer. In Perth, even on cloudy days, UV-A penetrates the clouds and reaches your skin. A 2023 Deloitte report found that photosensitivity reactions are 25-30% higher here than the global average.
That means if you’re on tetracycline and you live in Australia, you’re not just at risk-you’re in a high-risk zone. The Skin Cancer Foundation’s guidelines are not suggestions here. They’re survival tools.
And yet, most patients still aren’t warned. A 2023 survey of 1,200 Australian patients on tetracyclines found that only 32% received written sun safety instructions. The rest were left to guess-or worse, assume it was fine because "they’ve never burned before."
Final Takeaway
Tetracycline photosensitivity is preventable. It’s not an unavoidable side effect. It’s a predictable reaction to a known trigger: sunlight + drug.
If you’re prescribed doxycycline and you live where the sun is strong, ask for minocycline. If you’re stuck with doxycycline, treat your sunscreen like medicine-apply it every day, no exceptions. Wear a hat. Stay in the shade. Don’t wait until you’re blistered to realize you should’ve listened.
Antibiotics save lives. But they shouldn’t cost you your skin.

 2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
2026 Medication Safety Guidelines Update: ISMP, NIOSH, CMS Changes Explained
 Liver Disease and Drug Metabolism: How Reduced Clearance Affects Medication Safety
Liver Disease and Drug Metabolism: How Reduced Clearance Affects Medication Safety
 Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
 Where and How to Buy Calan Online Safely: Everything You Need to Know
Where and How to Buy Calan Online Safely: Everything You Need to Know
 Antitrust Laws and Competition Issues in Generic Pharmaceutical Markets
Antitrust Laws and Competition Issues in Generic Pharmaceutical Markets
Lily Steele
February 1, 2026 AT 00:48Just got prescribed doxycycline for acne and had no idea about this. Thanks for laying it out so clearly. I live in Arizona and already got burned once last summer-thought it was just bad sunscreen. Not anymore.
Rohit Kumar
February 1, 2026 AT 18:47In India, we don’t talk about this enough. People think antibiotics are just pills-you take them, you get better. But here, the sun doesn’t care if you’re sick or not. It burns through everything. I’ve seen patients with nail separation from doxycycline and thought it was fungus. Turned out it was the drug. Doctors need to stop assuming patients know this.
Minocycline is cheaper than you think here. Generic versions cost less than $2 a pill. If your doctor says no, ask for the formulary. They’re not protecting your wallet-they’re ignoring your skin.
And UPF clothing? We have local weavers who make it for under $10. No need to buy expensive American brands. Sun protection isn’t a luxury. It’s survival.
Stop waiting for blistering to happen. Start treating sunscreen like insulin-if you skip it, your body pays the price.
I’ve been telling this to every patient on tetracyclines since 2019. Most still don’t listen until they’re in pain. Don’t be one of them.
Also, car windows don’t block UV-A. I had a patient who got burned on his left arm driving to work. Left side of his face too. He thought he was safe because he wasn’t outside. Nope.
And yes, this is worse in monsoon season because people think clouds = protection. UV-A laughs at clouds.
Don’t say ‘I’ve never burned before.’ That’s like saying ‘I’ve never had a heart attack before.’ Doesn’t mean you’re immune.
Minocycline isn’t perfect. It can cause dizziness. But it’s not going to turn your hands into lobster claws.
If you’re on this drug and you’re outside, you’re already in damage mode. Your job now is to stop the bleeding.
Stop scrolling. Start applying zinc.
Carolyn Whitehead
February 3, 2026 AT 09:24Wow I had no idea about the nail thing. My nails have been weird for months and I thought it was just dryness. Guess I’ll go get my prescription checked out.
Amy Insalaco
February 4, 2026 AT 02:20While your clinical observations are empirically sound, the underlying epistemological framework of this post fundamentally misrepresents the ontological primacy of phototoxicity as a pharmacodynamic phenomenon. The reductionist framing of ‘sunscreen as medicine’ reflects a neoliberal biomedical hegemony that pathologizes natural environmental interaction. Zinc oxide, while physically effective, is a mineralogical barrier that disrupts the skin’s homeostatic photoprotection mechanisms-mechanisms evolutionarily optimized over millennia. The real issue isn’t the antibiotic-it’s the cultural commodification of UV avoidance as a virtue, which serves dermatological corporations and sunscreen conglomerates more than it serves biological integrity.
Furthermore, the suggestion that minocycline is ‘safer’ ignores its neurotoxic potential and the fact that its lipophilicity increases CNS penetration, which may lead to vestibular disturbances in genetically predisposed individuals. Sarecycline? A patent-protected pharmacokinetic sleight-of-hand designed to extract premium pricing from patients already burdened by pharmaceutical inflation. The true solution lies not in substitution, but in epigenetic modulation of cytochrome P450 expression via circadian rhythm entrainment and flavonoid-rich phytonutrient supplementation.
And let’s not forget: UV-A exposure at 10 a.m. is biologically distinct from UV-A at 3 p.m. due to Rayleigh scattering variance and atmospheric ozone absorption gradients. Your blanket ‘avoid 10 a.m. to 4 p.m.’ directive is statistically reductive and ignores chronopharmacological nuance.
TL;DR: Stop treating symptoms. Question the system.
kate jones
February 4, 2026 AT 04:10Correcting a minor error in the post: the 2021 Dermatologic Therapy study tracked 523 patients, not 500. Also, photo-onycholysis is most common with doxycycline at doses ≥100 mg/day, not just any dose. And for those asking about alternatives-azithromycin is not always a suitable substitute for Lyme disease; it’s only effective in early-stage, non-neurologic cases. Always confirm the indication before switching.
Also, UPF 50+ hats are essential, but the brim must be ≥3 inches. A baseball cap gives you 30% UV reduction on the neck. A wide-brimmed hat? 73%. That’s not marketing-that’s physics.
And yes, car window film works. I installed it in my Tesla. No more left-arm burns on my commute.
Gaurav Meena
February 4, 2026 AT 15:31Bro, I’ve been on doxycycline for 3 months for acne. I thought I was being careful-sunscreen, hat, all that. Then I got this weird patch on my neck that won’t fade. Now I’m scared to go outside. I didn’t know it could last for months. Thanks for the heads up. I’m switching to minocycline tomorrow. If you’re reading this and you’re on doxy-please, just ask your doctor. Don’t wait till you look like a boiled lobster.
Rob Webber
February 4, 2026 AT 21:49THIS IS A SCAM. DOXICYCLINE IS A TOXIN. THE PHARMA COMPANIES KNOW THIS AND STILL PUSH IT BECAUSE IT’S CHEAP. I’M A 32-YEAR-OLD MAN WHO GOT BLISTERED ON MY CHEST JUST WALKING TO THE MAILBOX. I HAD TO GO TO THE ER. THEY DIDN’T EVEN ASK IF I WAS ON ANTIBIOTICS. I WASN’T EVEN ON VACATION. I WAS JUST LIVING MY LIFE. NOW I HAVE DARK PATCHES THAT LOOK LIKE I WAS TATTOOED BY THE SUN. THIS IS NOT A SIDE EFFECT. THIS IS NEGLIGENCE. THEY NEED TO BAN DOXYCYCLINE FOR OUTDOOR USE. I’M STARTING A PETITION.
Jodi Olson
February 5, 2026 AT 00:47It’s interesting how we’ve normalized pharmaceutical risk as a personal responsibility issue rather than a systemic one. The onus is placed on the patient to research, to advocate, to reapply sunscreen every two hours-while the prescribing physician, often under time constraints and incentivized by cost-efficiency, remains unaccountable. The fact that 68% of patients receive no warning speaks not to patient ignorance, but to institutional failure. We treat drug safety as a checklist item rather than a moral imperative.
And yet, the solution isn’t just better education-it’s regulatory reform. Why isn’t photosensitivity listed as a black-box warning on tetracycline packaging? Why isn’t there a mandatory counseling protocol for high-UV regions? We don’t let people drive without seatbelts. Why do we let them walk into the sun with tetracycline in their bloodstream?
Natasha Plebani
February 6, 2026 AT 19:57The phototoxic reaction mechanism is fascinating-it’s not just ROS generation, but the formation of a tetracycline-sensitizer complex that binds to melanin and creates a photoadduct that persists in dermal layers. That’s why hyperpigmentation lingers. The drug doesn’t just damage cells-it gets embedded in the pigmentary architecture. That’s why topical hydroquinone works better than corticosteroids: it targets the chromophore, not just the inflammation.
Also, zinc oxide isn’t just a physical blocker-it has antioxidant properties that quench free radicals. Titanium dioxide? Less effective against long-wave UV-A. So the choice of mineral matters. Look for micronized zinc oxide with a particle size under 100 nm. Anything larger and you’re getting scattering, not absorption.
And for the love of science, stop using spray sunscreens. You’re not applying 2 mg/cm²-you’re spraying a cloud and hoping for the best. That’s not sunscreen. That’s a gamble with your DNA.
Katie and Nathan Milburn
February 7, 2026 AT 20:15Thank you for this comprehensive overview. I am a physician in Oregon and have seen multiple cases of photo-onycholysis in patients on doxycycline. I now include a printed handout with every prescription. The most common response from patients is, ‘No one ever told me this.’ It’s not that they’re careless-it’s that the system doesn’t prioritize it. I appreciate the data-driven approach.
Beth Beltway
February 9, 2026 AT 04:18Just switched to minocycline last week after getting burned on my shoulders. No more sunburns. Just a little dizziness at first, but it’s worth it. My nails are already starting to look better. Do not wait like I did.