Managing diabetes isn’t just about taking pills or injecting insulin-it’s about staying safe while doing it. Every year, thousands of people end up in the emergency room because of a simple mistake: taking the wrong dose, mixing medications that shouldn’t be combined, or not realizing their blood sugar has dropped too low. The truth is, diabetes medications can save your life-but they can also put it at risk if you don’t understand how they work and what to watch for.
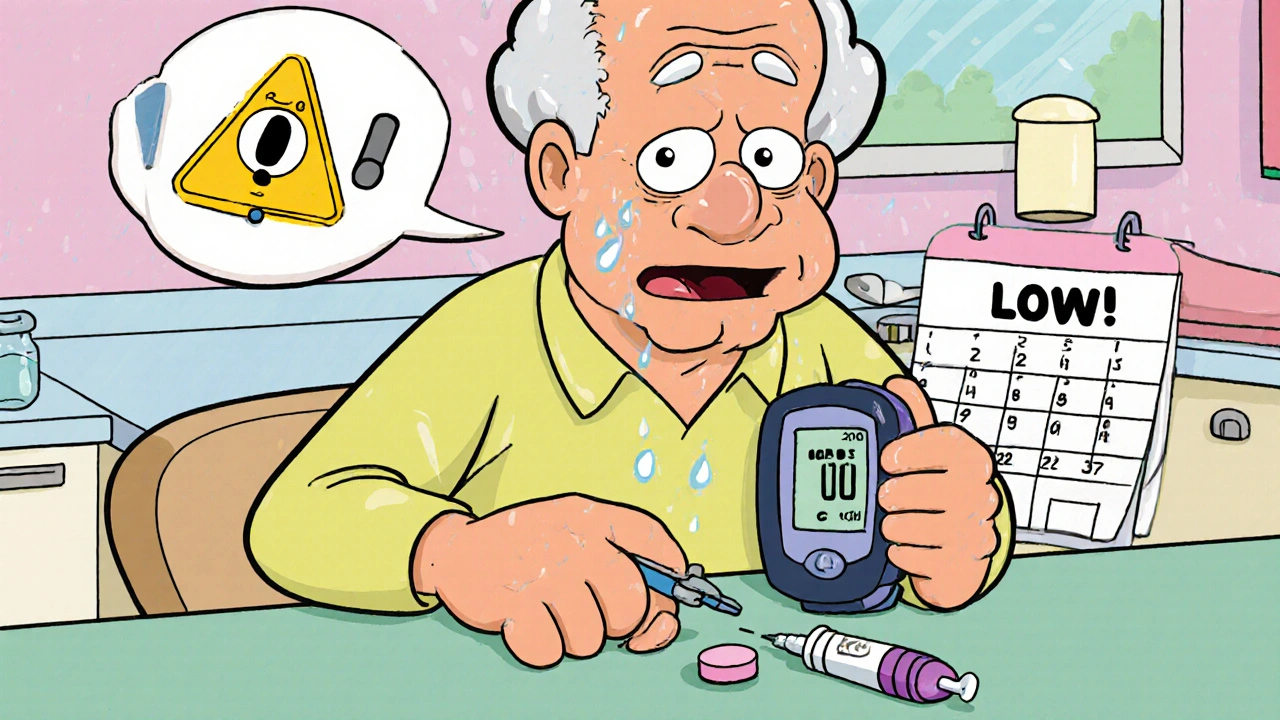
What Happens When Blood Sugar Drops Too Low?
Hypoglycemia is the most dangerous side effect of diabetes treatment. It’s not rare. About 20-40% of people on sulfonylureas like glipizide or glyburide will have at least one low blood sugar episode in a year. For some, it’s severe enough that they need help from someone else-maybe a family member or paramedic. And here’s the scary part: up to 30% of people with type 2 diabetes who seem to be doing well on these meds still get silent nighttime lows. They don’t feel dizzy or sweaty. Their body doesn’t warn them. They just wake up with a headache, confused, or worse.
Insulin is the biggest culprit. Even the newest long-acting types can cause low blood sugar if you skip a meal, exercise more than usual, or drink alcohol. And if you’re using concentrated insulin like Humulin R U-500, a single mistake in dosing can lead to a life-threatening overdose. There are videos online showing people mixing up U-500 with regular U-100 insulin-thinking they’re the same-and ending up in the hospital.
Oral Medications: Not All Are Created Equal
Metformin is still the first choice for most people with type 2 diabetes. Why? Because it doesn’t cause low blood sugar on its own. It also helps with weight and has been shown to reduce heart disease risk. But it’s not harmless. If your kidneys aren’t working well, metformin can build up in your body and cause lactic acidosis-a rare but deadly condition. That’s why doctors check your eGFR before starting it and again every year. If your eGFR falls below 30, you stop it. Between 30 and 45, you use it with caution. Between 45 and 60, you cut the dose.
Then there are the newer drugs-SGLT2 inhibitors like empagliflozin and dapagliflozin. They help your kidneys flush out sugar through urine. That lowers blood sugar, helps with weight loss, and protects your heart and kidneys. But they come with a hidden risk: diabetic ketoacidosis (DKA). You don’t need to be hyperglycemic to get it. Some people develop DKA with blood sugar levels that are only slightly elevated-or even normal. That’s called euglycemic DKA. It’s easy to miss because you don’t feel like you’re in a diabetic crisis. But it can turn deadly fast. That’s why doctors tell you to stop these drugs at least 24 hours before surgery and avoid very low-carb or ketogenic diets while on them.
GLP-1 receptor agonists like semaglutide and tirzepatide are great for weight loss and heart protection. But up to half the people who start them get nausea, vomiting, or diarrhea. It usually fades after a few weeks, but some people can’t tolerate it. And if you’re older or have stomach issues, this can lead to dehydration, which increases your risk of kidney problems and DKA.
Drug Interactions You Can’t Ignore
Diabetes meds don’t live in a vacuum. They interact with other drugs you might be taking-and those interactions can be deadly.
Antibiotics like sulfamethoxazole/trimethoprim (Bactrim) can make insulin and sulfonylureas work too hard, causing severe hypoglycemia. That’s why people on Reddit share stories of going low after a simple UTI treatment. Quinine (used for leg cramps), sunitinib (a cancer drug), and somatostatin analogues (used for hormonal disorders) all raise the same risk. Even over-the-counter meds like certain cold remedies with pseudoephedrine can spike blood sugar, making your diabetes harder to control.
If you’re on insulin or sulfonylureas, always tell your pharmacist and doctor about every new prescription, supplement, or herb you start. Don’t assume it’s safe just because it’s “natural.” St. John’s wort, for example, can interfere with how your body processes metformin and other drugs.
Special Risks for Older Adults
One in four hospital stays for diabetes complications involves someone over 65. Why? Because aging changes how your body handles medicine.
Older adults are more likely to have kidney problems, eat less, move slower, and forget doses. They’re also more likely to have hypoglycemia unawareness-meaning their body stops sending warning signs. A dizzy spell might seem like just getting old. But it could be a low blood sugar. And that dizzy spell? It can lead to a fall, a broken hip, or a head injury. Banner Health reports that dizziness from diabetes meds is one of the top reasons older adults end up in the ER.
Doctors now recommend starting sulfonylureas at half the usual dose for people over 65. And they avoid long-acting ones like glyburide, which stick around in the body longer and increase the risk of prolonged lows. Glipizide is often preferred because it’s cleared by the liver, not the kidneys, making it safer for older patients with reduced kidney function.
Insulin: How to Use It Without Putting Yourself at Risk
Using insulin correctly isn’t just about timing. It’s about technique.
Always rotate your injection sites-abdomen, thighs, arms, buttocks. Injecting in the same spot over and over can cause lumps under the skin (lipohypertrophy). These lumps absorb insulin unpredictably, leading to wild swings in blood sugar. Don’t inject into muscle unless your doctor tells you to-muscle absorbs insulin faster than fat, which can cause sudden drops.
Store your insulin properly. If it’s too hot or too cold, it breaks down and doesn’t work right. Never leave it in a car in summer or in the freezer. Check the color and clarity. If it looks cloudy when it shouldn’t, or has particles in it, throw it out.
And never share your insulin pen or syringe-not even with family members. It’s not just about infection risk. Different people need different doses. One mistake can kill.

What You Can Do Right Now to Stay Safe
Here’s a simple checklist to follow every day:
- Know your meds. Write down every drug you take, including dose and time. Keep a copy in your wallet and on your phone.
- Check your blood sugar. If you’re on insulin or sulfonylureas, test before meals, at bedtime, and if you feel off-even if you think it’s just stress or tiredness.
- Carry fast-acting sugar. Glucose tablets, juice boxes, or candy. Don’t wait until you feel bad. Keep them with you at all times.
- Wear a medical ID. A bracelet or necklace that says “Diabetic-Insulin Dependent” or “On Sulfonylureas.” In an emergency, it tells responders what’s going on before you can speak.
- Get your kidneys checked. Ask for an eGFR test at least once a year. If you’re on metformin or SGLT2 inhibitors, this is non-negotiable.
- Talk to your pharmacist. They see all your prescriptions. They’ll catch interactions your doctor might miss.
What’s Changing in 2025?
Technology is making diabetes safer. Automated insulin delivery (AID) systems-sometimes called “artificial pancreas” devices-are now widely available. These systems use real-time glucose readings to adjust insulin doses automatically. Studies show they increase time in the target range by 20% and cut hypoglycemia by up to 40% compared to older pump systems.
New drugs are also emerging. Tirzepatide (Mounjaro), a dual GLP-1/GIP agonist approved in 2022, is now being used more often because it lowers blood sugar and weight better than older GLP-1 drugs. But it still carries the same GI side effects and DKA warnings.
The American Diabetes Association and the American Association of Clinical Endocrinologists now stress that treatment should be personalized-not just based on blood sugar numbers, but on your age, kidney health, heart risk, lifestyle, and ability to manage complex regimens.
When to Call for Help
Call 911 or go to the ER if you experience:
- Confusion, seizures, or loss of consciousness
- Severe nausea, vomiting, and abdominal pain (possible DKA)
- Difficulty breathing or fruity-smelling breath
- Low blood sugar that doesn’t improve after three doses of glucose
And if you’re ever unsure whether a symptom is “just diabetes” or something worse-err on the side of caution. Better to be checked than to wait.
Can I stop my diabetes medication if my blood sugar is normal?
No. Even if your blood sugar looks good, stopping your meds can cause a dangerous rebound. Type 2 diabetes is a progressive condition. What works today might not be enough next year. Always talk to your doctor before making changes. Stopping insulin suddenly can lead to diabetic ketoacidosis-even in type 2 patients.
Are natural supplements safe to take with diabetes drugs?
Some can be dangerous. Berberine, cinnamon, and bitter melon may lower blood sugar, which can push you into hypoglycemia when combined with insulin or sulfonylureas. Others, like licorice root, can raise blood pressure and interfere with kidney function. Always tell your doctor about any supplement you’re taking-even if you think it’s harmless.
Why do I get yeast infections with SGLT2 inhibitors?
SGLT2 inhibitors make your kidneys dump sugar into your urine. That sugar feeds yeast, especially in warm, moist areas like the genitals. About 4-5% of users get infections-more than double the rate of people on placebo. It’s treatable with antifungal creams or pills, but if you keep getting them, talk to your doctor about switching meds.
Is metformin safe if I have mild kidney disease?
It can be, but only with caution. If your eGFR is between 45 and 60, your doctor will lower your dose. If it’s between 30 and 45, they might still prescribe it but monitor you closely. Below 30, it’s not safe. Always get your kidney function tested before starting and at least once a year after.
What should I do if I miss a dose of insulin?
Don’t double up. If you miss a mealtime insulin dose, check your blood sugar. If it’s high, you might need a small correction dose-but only if your doctor gave you a plan for this. If you miss long-acting insulin, call your provider. Never guess. Missing insulin can lead to high blood sugar, DKA, or long-term damage.
Can alcohol affect my diabetes meds?
Yes, and it’s risky. Alcohol can block your liver from releasing glucose, which increases the chance of hypoglycemia-especially if you’re on insulin or sulfonylureas. It can also mask the symptoms of low blood sugar. If you drink, do it with food, limit it to one drink, and always check your blood sugar before bed.
 Chloroquine: Uses, Side Effects, Dosage & the Latest COVID‑19 Findings
Chloroquine: Uses, Side Effects, Dosage & the Latest COVID‑19 Findings
 Why Acetaminophen Helps with Social Pain: Surprising Research Insights
Why Acetaminophen Helps with Social Pain: Surprising Research Insights
 Multiple Myeloma Hope Stories: Survival, Treatments & Resilience
Multiple Myeloma Hope Stories: Survival, Treatments & Resilience
 Generic Drug Prices: Why Americans Pay Less Than Europeans
Generic Drug Prices: Why Americans Pay Less Than Europeans
 Buy Cheap Generic Amoxicillin Online - Australian Guide 2025
Buy Cheap Generic Amoxicillin Online - Australian Guide 2025
Deepa Lakshminarasimhan
November 13, 2025 AT 10:25they’re lying about insulin safety. i’ve seen the videos. the FDA knows U-500 gets mixed up all the time but they won’t change the labeling because big pharma owns them. my uncle died from a dose error and they called it ‘user error’ - like he was dumb for trusting the pen. same thing with metformin. they push it because it’s cheap, not because it’s safe. check the whistleblower docs. they’re hiding the lactic acidosis rates.
Erica Cruz
November 15, 2025 AT 08:56Wow. So much text. And zero actual data on mortality rates. Where’s the CDC study comparing these drugs’ real-world death rates? Also, ‘euglycemic DKA’ is just a buzzword pharma invented to scare people into buying more monitors. If you’re not hyperglycemic, it’s not DKA. It’s just ketoacidosis. Stop the fearmongering.
Johnson Abraham
November 16, 2025 AT 19:46lol so now we gotta worry about yeast infections from sugar in pee? 🤦♂️ next they’ll say walking causes diabetes. just stop taking the meds if you don’t like the side effects. also st john’s wort? yeah right. i take it with my metformin and my sugar’s perfect. 😎
Shante Ajadeen
November 17, 2025 AT 15:47thank you for this. i’m 68 and on glipizide and i was scared to ask my doc about switching because i thought i was just ‘getting old.’ this checklist? i printed it. my daughter’s keeping a copy in her phone now. you just saved me from a fall.
dace yates
November 18, 2025 AT 22:47how common is it for people on SGLT2 inhibitors to get euglycemic DKA? like, actual stats? the post says it’s ‘easy to miss’ but doesn’t say how often it happens. is it 1 in 100? 1 in 1000? i need numbers before i panic.
Danae Miley
November 19, 2025 AT 01:24The article incorrectly conflates ‘risk’ with ‘prevalence.’ Hypoglycemia rates in sulfonylurea users are not ‘20–40%’ because that’s cumulative over years, not annual incidence. Also, ‘silent nighttime lows’ aren’t ‘scary’-they’re clinically documented. Precision matters. Fix the language before you scare people.
Mark Rutkowski
November 20, 2025 AT 22:13Medicine isn’t a checklist. It’s a conversation between your body and your choices. The real danger isn’t the drug-it’s the belief that someone else’s algorithm knows what your soul needs. I’ve seen people die from fear of their own insulin. And I’ve seen others thrive because they listened-not to a blog, but to their heartbeat when it skipped after a walk. Trust yourself. But keep the juice box handy.
Ryan Everhart
November 20, 2025 AT 23:29so you're telling me if i drink a beer and forget to test i might die? wow. thanks for the emergency manual. next time i'll just skip the beer and the diabetes. easier. 🤷♂️
David Barry
November 21, 2025 AT 22:35Insulin isn’t the problem. The problem is people treating it like aspirin. You don’t inject a drug you don’t understand and expect miracles. I’ve worked ER in Sydney. Saw three U-500 mix-ups last year. All from patients who trusted the pen label. No one taught them the difference between U-100 and U-500. That’s not a med failure. That’s a system failure.
Alyssa Lopez
November 22, 2025 AT 12:13THIS is why america’s healthcare is broken. You people are scared of everything. Metformin? It’s been used for 60 years. SGLT2? It’s cutting heart failure hospitalizations. You want to live longer? Take the meds. Stop reading Reddit doom threads. And for god’s sake, stop with the ‘natural supplements’ nonsense. If it’s not FDA-approved, it’s not medicine. It’s snake oil. 🇺🇸