Insulin Safety: What You Need to Know About Using Insulin Correctly
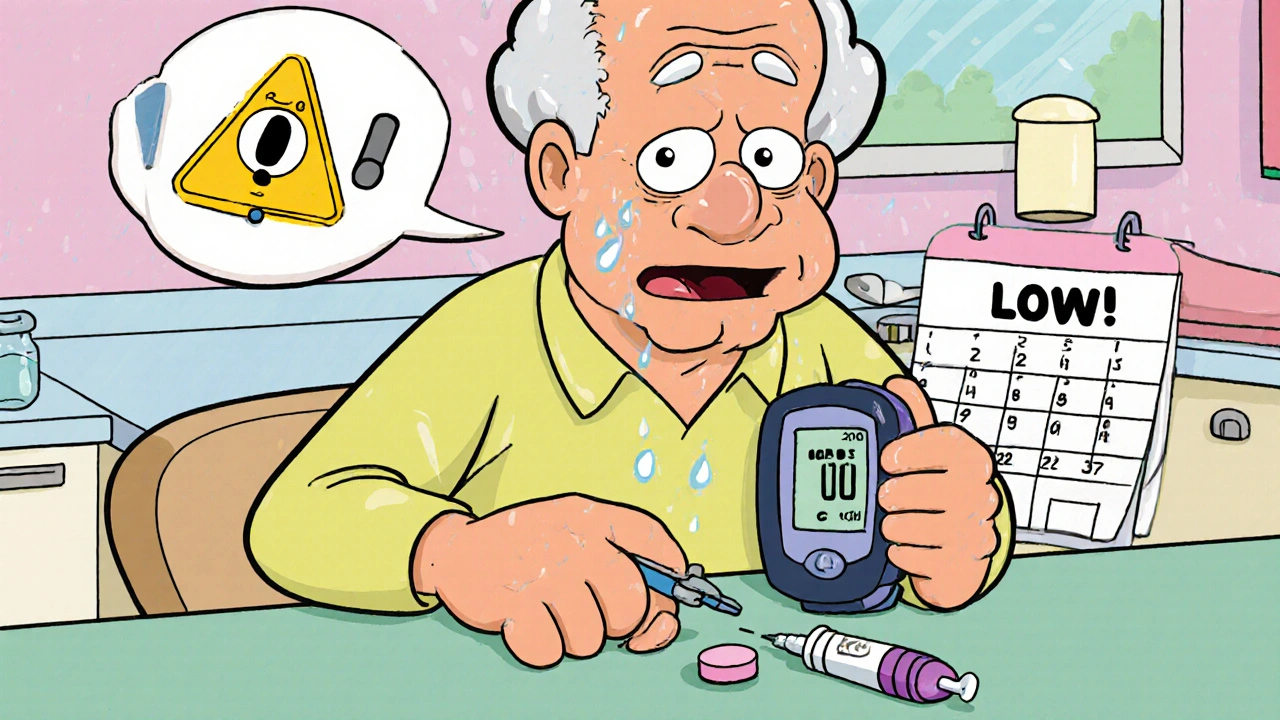
When you're using insulin, a life-saving hormone that controls blood sugar in people with diabetes. Also known as diabetes medication, it's not just a shot—it's a daily commitment to precision. One wrong dose, one expired pen, one skipped meal, and you could slip into hypoglycemia, a dangerous drop in blood sugar that can cause confusion, seizures, or even unconsciousness. It’s not rare. Studies show nearly half of people on insulin have had at least one serious low-blood-sugar episode. But most of these aren’t accidents—they’re avoidable mistakes.
Insulin storage, how you keep your insulin cold or at room temperature matters more than you think. Heat, sunlight, or freezing can wreck the medicine without you noticing. A vial left in a hot car or a pen stored in the freezer might still look fine—but it won’t work right. And insulin injection, the way you deliver the drug into your body isn’t just about pinching skin and pushing a plunger. Needle reuse, wrong angles, or injecting into scar tissue can change how fast your body absorbs it—leading to unpredictable highs and lows.
People often think insulin safety is about counting carbs or checking blood sugar. It’s those things, yes—but it’s also about knowing when your pen is empty, how to tell if your insulin looks cloudy or clumpy, and why you should never share needles—even with family. It’s about understanding that a low blood sugar at 3 a.m. isn’t just "bad luck," it’s a sign something in your routine needs fixing. The posts below give you real, no-fluff advice: how to spot insulin errors before they hurt you, what to do when your pump fails, why some people need different types of insulin, and how to talk to your doctor about safety without sounding paranoid. This isn’t theory. It’s what keeps people out of the hospital.