Extended-Release Tablets: How They Work and Why They Matter
When you take an extended-release tablet, a type of medication designed to release its active ingredient slowly over many hours. Also known as controlled-release or slow-release pills, these tablets help keep drug levels steady in your bloodstream instead of spiking and crashing like regular pills do. This isn’t just convenience—it’s science that reduces side effects, cuts down on daily doses, and helps people stick to their treatment.
Think of it like this: a regular pill might last 4 to 6 hours, so you need to take it three times a day. An extended-release tablet can last 12 to 24 hours, meaning you take it once. That’s why they’re common for blood pressure meds like verapamil, antidepressants like trazodone, or even pain relievers. For someone managing chronic conditions—like high blood pressure, diabetes, or anxiety—fewer pills mean fewer missed doses and better control. But they’re not for everyone. If your body processes drugs differently, or if you have gut issues, the slow release might not work right. That’s why doctors often compare them to immediate-release versions before switching.
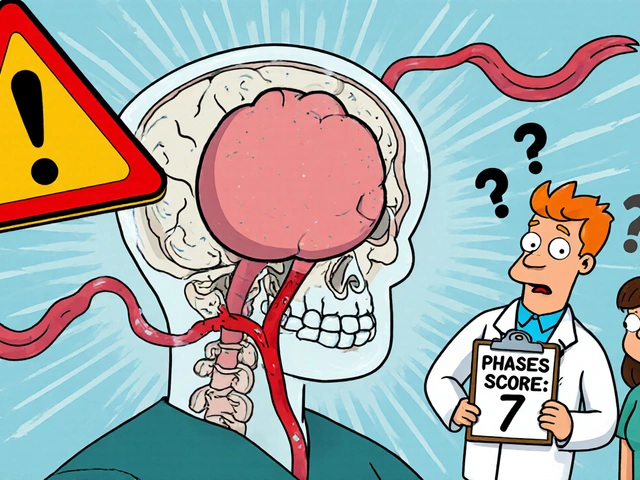
These tablets rely on smart coatings or matrix systems—sometimes wax, sometimes polymers—to control how fast the drug leaks out. That’s different from capsules that dissolve fast or injections that hit hard and quick. The design matters. A poorly made extended-release pill can dump all its drug at once, which is dangerous. That’s why the FDA and other agencies watch these closely. You’ll see them in many of the guides below, like comparisons of Isoptin (Verapamil), a calcium channel blocker often prescribed in extended-release form for heart rhythm and high blood pressure, or Amaryl (Glimepiride), a diabetes drug where steady release helps avoid blood sugar crashes. Even Trazodone, a sleep and depression aid, comes in extended-release versions to reduce next-day drowsiness. These aren’t just labels—they’re functional choices that affect how you feel all day.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll see real comparisons between extended-release versions and their quick-acting cousins, tips on when to ask your doctor about switching, and how to spot if your pill isn’t working right. Some posts break down how these pills interact with food, others show you how to handle them safely if you have trouble swallowing, and a few even explain why some generics behave differently than others. No fluff. Just clear, real-world info from people who’ve been there—whether you’re managing your own meds or helping someone else.