Comorbidities and Drugs: How Multiple Conditions Affect Your Medications
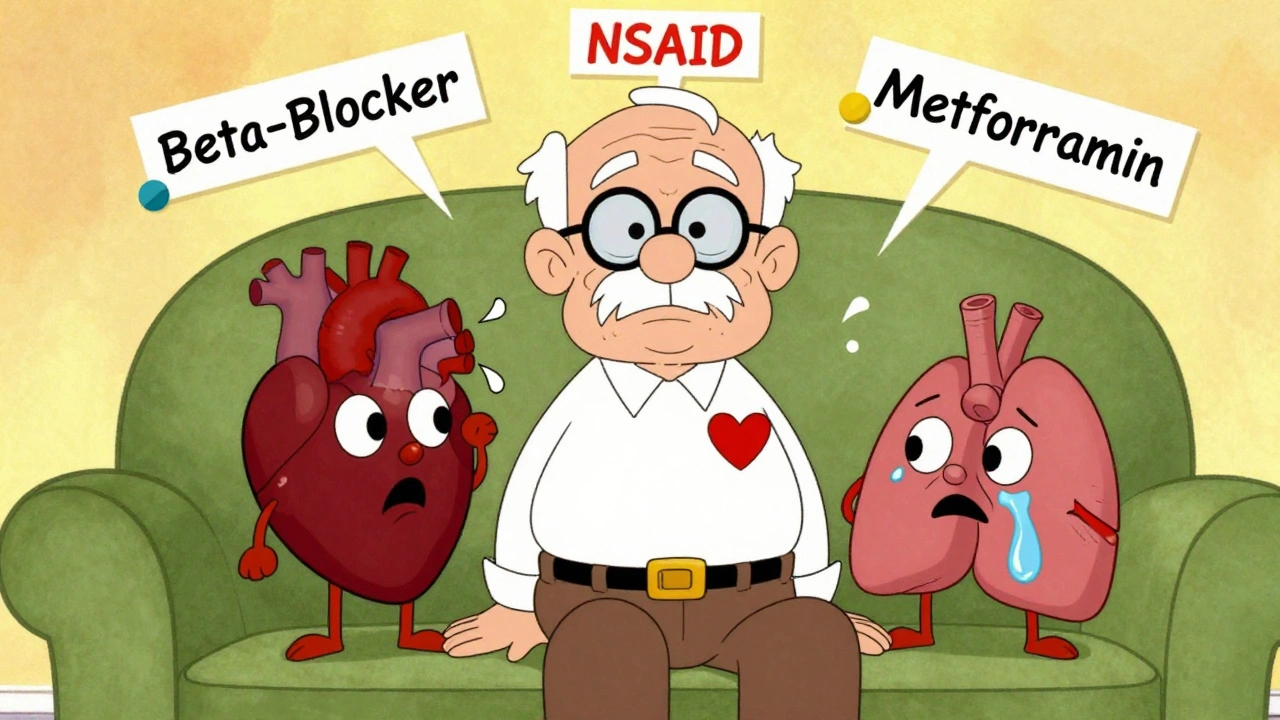
When you’re managing comorbidities and drugs, the presence of two or more chronic health conditions at the same time. Also known as multimorbidity, it’s not rare—it’s the new normal for millions of adults on long-term medication. If you’re taking insulin for diabetes, a beta blocker for high blood pressure, and an SSRI for depression, you’re not just juggling pills—you’re navigating a minefield of hidden risks. These conditions don’t exist in isolation, and neither do the drugs used to treat them.
Take polypharmacy, the use of multiple medications at once, often five or more. Also known as multiple drug therapy, it’s common among older adults and people with chronic conditions, long-lasting illnesses like heart disease, kidney disease, or autoimmune disorders. Also known as long-term health issues, it affects nearly half of adults over 65. The problem isn’t the number of pills—it’s how they interact. For example, combining SSRIs with certain pain meds like tramadol can trigger serotonin syndrome, a life-threatening reaction. Or, taking statins with grapefruit juice can spike drug levels in your blood to dangerous levels. These aren’t edge cases. They happen daily in clinics and homes.
Drug interactions don’t always show up as dramatic side effects. Sometimes they’re quiet—like when a blood pressure med makes your diabetes harder to control, or when an antacid reduces the absorption of your thyroid pill. Your kidneys and liver don’t work the same way when you have both heart failure and kidney disease, so a dose that’s safe for one person could overdose another. That’s why generic substitution isn’t always harmless, even if the FDA says it’s bioequivalent. Your body isn’t a lab test. It’s a living system with overlapping problems.
And it’s not just about the drugs. Your diet, your sleep, your stress levels—all of it changes how your body handles medication. If you have celiac disease and are on immunosuppressants after a transplant, a gluten slip-up can throw your entire regimen off. If you’re on insulin and also trying to lose weight with a GLP-1 agonist, your risk of low blood sugar spikes if you skip meals. These aren’t theoretical concerns. They’re the reason people end up in the ER.
What you’ll find below isn’t a list of abstract medical theories. It’s a collection of real, practical stories and guides from people who’ve been there. You’ll see how to spot dangerous drug combinations, how to talk to your pharmacist about interactions, how to manage refills when you’re traveling with multiple prescriptions, and why reading your drug label isn’t optional. Some posts break down how insulin affects weight, how SSRIs and opioids can collide, and why generic drugs sometimes need extra caution. Others show you how to set up alerts so you never run out of a critical med. This isn’t about guessing. It’s about knowing exactly what’s in your medicine cabinet—and why it matters.