SSRI-Opioid Risk Checker
Check Your Medication Risk
Select your SSRI and opioid medications to see the serotonin syndrome risk level. Always consult your doctor before changing medications.
Select medications to see your risk level
Combining SSRIs and opioids might seem like a harmless move if you're managing both depression and chronic pain. But this common mix can trigger something dangerous: serotonin syndrome. It doesn't happen often, but when it does, it can turn deadly in hours. You might feel fine one day, then wake up shaking, sweating, and heart racing - not from anxiety, but from your own medications pushing serotonin levels too high.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn't a rare side effect - it's a predictable reaction to too much serotonin in your brain and nervous system. SSRIs like sertraline, fluoxetine, and escitalopram work by blocking the reuptake of serotonin, keeping more of it active in your synapses. Opioids like tramadol, methadone, and pethidine also boost serotonin - not just by pain relief, but by directly interfering with how serotonin is cleared from nerve connections. When these two types of drugs meet, serotonin builds up fast. Your body can't handle it.The symptoms don’t sneak up slowly. They hit hard and fast - often within hours of taking a new dose or increasing one. Mild cases mean shivering, diarrhea, a fast heartbeat, or sweating you can’t control. Severe cases? Core body temperature over 41°C (106°F), muscle rigidity, seizures, and organ failure. Around 10% of untreated severe cases end in death.
Doctors use the Hunter criteria to diagnose it - not guesswork. If you have spontaneous clonus (involuntary muscle jerks), or inducible clonus with agitation and sweating, or tremor with hyperreflexia, it’s serotonin syndrome. No lab test confirms it. It’s all in the symptoms and what you’re taking.
Not All Opioids Are Created Equal
Here’s the critical part: not every opioid is risky with SSRIs. Some barely touch serotonin at all. Others? They’re ticking time bombs.High-risk opioids: Tramadol, methadone, pethidine (meperidine). These directly block the serotonin transporter (SERT), the same mechanism SSRIs use. Tramadol is especially dangerous - studies show it’s 30 times more potent at blocking SERT than morphine. In FDA reports from 2018-2022, tramadol was involved in nearly 4 out of 10 serotonin syndrome cases linked to opioids.
Low-risk opioids: Morphine, oxycodone, buprenorphine, hydromorphone, codeine. These don’t significantly inhibit SERT or activate serotonin receptors. That doesn’t mean they’re 100% safe - there are rare case reports of codeine causing serotonin syndrome when combined with other serotonergic drugs - but the risk is far lower.
Even fentanyl is tricky. Lab tests say it doesn’t block SERT. Yet there are over 120 documented cases of serotonin syndrome with fentanyl. Why? It likely binds directly to serotonin receptors (5-HT1A and 5-HT2A), bypassing the usual pathway. In real life, lab results don’t always match what happens in a patient’s body.
Which SSRIs Are Most Dangerous?
Not all antidepressants carry the same risk. Fluoxetine (Prozac) stands out because of its long half-life. Its active metabolite, norfluoxetine, sticks around for up to 16 days. So even if you stop taking it, the risk lingers. That’s why experts recommend waiting five weeks before switching to another serotonergic drug.Sertraline (Zoloft) clears faster - about 26 hours. That makes it slightly safer in transitions. But don’t assume short half-life = no risk. Any SSRI combined with a high-risk opioid can still cause serotonin syndrome. The real danger is in the combination, not just the drug itself.
SNRIs like venlafaxine (Effexor) and duloxetine (Cymbalta) are even more potent at raising serotonin than SSRIs. If you’re on one of these and an opioid like tramadol, your risk jumps again.

Who’s Most at Risk?
It’s not just about the drugs. Your body matters too.Older adults are at higher risk. People over 65 take an average of 31% more medications than younger people. More drugs = more chances for interaction. That’s why the American Geriatrics Society lists tramadol as potentially inappropriate for seniors already on SSRIs.
People with liver or kidney problems are also vulnerable. If your body can’t break down drugs properly, they build up. A standard dose of tramadol might be fine for a healthy 40-year-old, but toxic for someone with cirrhosis or kidney disease.
Genetics play a role too. About 7% of people are poor metabolizers of CYP2D6, the enzyme that breaks down tramadol and some other opioids. These people convert tramadol into its active form slower - but when they do, serotonin levels spike unpredictably. Studies show they’re over three times more likely to develop serotonin syndrome.
Real Cases, Real Consequences
This isn’t theoretical. In a 68-year-old woman taking sertraline, doctors prescribed tramadol after surgery. Twelve hours later, she was running a fever of 40.2°C, her blood pressure was 180/100, and she had spontaneous muscle spasms. She was admitted to ICU. She survived - but only because the staff recognized it quickly.Another case: a patient on paroxetine was given codeine for pain. Doctors thought codeine was safe. She developed serotonin syndrome. That case changed how some hospitals view even "low-risk" opioids.
Hospital pharmacists in the U.S. report seeing 2-3 cases a month - mostly in post-op patients on SSRIs who got tramadol for pain. And here’s the scary part: 44% of these cases were initially misdiagnosed as neuroleptic malignant syndrome or anticholinergic toxicity. That delay costs lives.
How to Prevent It
Prevention is simple - if you follow the rules.1. Avoid high-risk combos entirely. If you’re on an SSRI or SNRI, don’t take tramadol, methadone, or pethidine. Period. There are safer alternatives.
2. Choose safer opioids. Morphine, oxycodone, hydromorphone, or buprenorphine are far less likely to trigger serotonin syndrome. Ask your doctor: "Is there a painkiller that won’t interact with my antidepressant?"
3. Watch for early signs. If you start feeling unusually shaky, sweaty, or your heart races after starting a new pain med - stop it and call your doctor. Don’t wait. Muscle twitching, diarrhea, confusion - these aren’t "just side effects." They’re red flags.
4. Give your body time to clear old drugs. If you’re switching from an SSRI to another antidepressant, or stopping one to start an opioid, wait at least two weeks. For fluoxetine, wait five weeks. Your pharmacist can help you map this out.
5. Use technology. Hospitals like Kaiser Permanente cut dangerous prescriptions by 87% after their electronic systems blocked tramadol-SSRI combos automatically. Ask if your doctor’s system has these alerts. If not, bring this info to them.
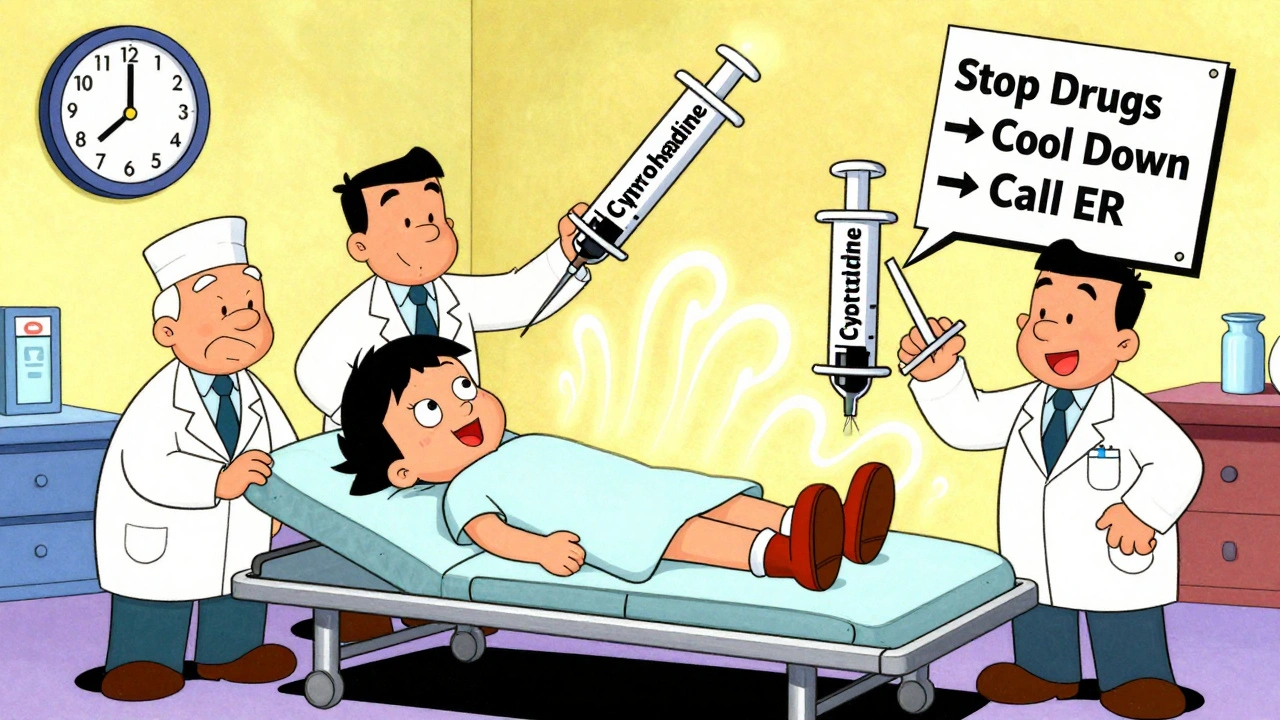
What If It Happens?
If serotonin syndrome is suspected, stop all serotonergic drugs immediately. That’s step one.For mild cases: supportive care - fluids, cooling, benzodiazepines for agitation. Symptoms usually resolve in 24-72 hours.
For severe cases: you need cyproheptadine, a serotonin blocker. Dose: 12 mg initially, then 2 mg every two hours until symptoms improve. Aggressive cooling, IV fluids, and ICU monitoring are critical. Delayed treatment increases death risk.
Don’t try to tough it out. Don’t assume it’s "just anxiety" or "a bad reaction to pain meds." If you’re on an SSRI and take tramadol - and then feel like you’re burning up from the inside - get help now.
The Bigger Picture
Between 2017 and 2022, serotonin syndrome cases rose by over 34%. Why? More people are on antidepressants. More people are on opioids. And too many prescribers still don’t connect the dots.Regulators are catching up. The FDA now requires opioid medication guides to include serotonin syndrome warnings. The EMA updated tramadol labels in 2021. Epic Systems is building new tools for 2024 that will flag 17 specific drug-gene interactions tied to serotonin metabolism.
But the real fix? Better communication. You need to tell every doctor you see - including dentists and ER staff - what you’re taking. Write it down. Carry a list. Don’t assume they’ll check your records.
There’s no shame in asking: "Is this painkiller safe with my antidepressant?" If your doctor says yes without hesitation - ask for proof. Look up the drug interaction yourself. You’re not being difficult. You’re protecting your life.
Can I take oxycodone with an SSRI?
Yes, oxycodone is considered low-risk for serotonin syndrome because it doesn’t significantly block serotonin reuptake or activate serotonin receptors. It’s often recommended as a safer alternative to tramadol or methadone when you’re on an SSRI. Still, monitor for symptoms like shivering, rapid heartbeat, or confusion - especially when starting or increasing the dose.
How long does it take for serotonin syndrome to go away?
Mild cases usually resolve within 24 to 72 hours after stopping the offending drugs. Severe cases require hospitalization and can take days to weeks, depending on how long the drugs stay in your system. Fluoxetine and its metabolites can linger for up to 16 days, so symptoms may return if you restart a serotonergic drug too soon.
Is tramadol ever safe with SSRIs?
No - not reliably. Tramadol has a 4.4 times higher risk of causing serotonin syndrome than morphine when combined with SSRIs. Even "low doses" can trigger it, especially in older adults or those with liver/kidney issues. Experts and guidelines strongly advise avoiding this combination entirely. Safer painkillers exist.
Can codeine cause serotonin syndrome?
Yes - though it’s rare. Earlier studies thought codeine was safe, but case reports now show it can trigger serotonin syndrome, especially when combined with other serotonergic drugs like SSRIs or SNRIs. Don’t assume it’s harmless just because it’s "mild."
What should I do if I think I have serotonin syndrome?
Stop taking all serotonergic drugs immediately. Call emergency services or go to the nearest ER. Don’t wait. Tell them you’re on an SSRI and took an opioid recently. Symptoms like uncontrollable shaking, high fever, or muscle stiffness need urgent treatment. Delaying care increases the risk of death.

 Antabuse Online Prescription: A Comprehensive Guide
Antabuse Online Prescription: A Comprehensive Guide
 Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
Calcipotriol for Psoriasis in Skin of Color: Benefits, Risks & Usage
 Hemophilia and Alcohol: Essential Facts and Safe Practices
Hemophilia and Alcohol: Essential Facts and Safe Practices
 Prophylaxis for Orthodontic Patients: Keeping Your Braces Clean and Effective
Prophylaxis for Orthodontic Patients: Keeping Your Braces Clean and Effective
 Finding Pharmacies and Medication Help Abroad: A Traveler’s Guide
Finding Pharmacies and Medication Help Abroad: A Traveler’s Guide
Rashmin Patel
December 3, 2025 AT 08:40Wow, this is one of the most thorough breakdowns I’ve ever seen on serotonin syndrome. I’m a nurse in Mumbai and we’ve had two ICU admissions in the last year from tramadol + sertraline combos - both elderly patients. One guy thought tramadol was just a "stronger painkiller" because his friend took it. No one warned him. I printed out this exact article and gave copies to every junior doc on my floor. 🙏 If you’re on an SSRI, please, please, please ask your pharmacist before taking ANY new pain med. Not your doctor. Not your buddy. The pharmacist. They’re the unsung heroes here.
sagar bhute
December 3, 2025 AT 13:26This is just pharma fearmongering. People have been mixing tramadol and SSRIs for decades and nobody died. Your "10% death rate" is cherry-picked from worst-case ER reports. If you’re paranoid about serotonin syndrome, maybe don’t take antidepressants at all. Or better yet - stop blaming opioids and fix your mental health first. This article reads like a drug company’s liability pamphlet.
Cindy Lopez
December 4, 2025 AT 00:06There’s a grammatical error in the second paragraph: "keeping more of it active in your synapses. Opioids like tramadol, methadone, and pethidine also boost serotonin - not just by pain relief, but by directly interfering with how serotonin is cleared from nerve connections. When these two types of drugs meet, serotonin builds up fast. Your body can't handle it." The period after "synapses" should be a comma, since the next clause is a continuation, not a new sentence. Also, "nerve connections" is imprecise - it’s synaptic clefts. Minor, but it undermines credibility.
James Kerr
December 5, 2025 AT 12:29Big thanks for laying this out so clearly. I’m on escitalopram and had a knee surgery last year - my doc almost gave me tramadol until I showed him this. He switched me to oxycodone and I’m fine. No weird shaking, no panic attacks. Just pain relief. Seriously, if you’re reading this and you’re on an SSRI, just ask: "What’s the safest painkiller for me?" It’s not weird. It’s smart. 💪
shalini vaishnav
December 6, 2025 AT 03:32Of course Americans are panicking over this. In India, we’ve been managing pain with tramadol for 30 years. Our doctors know what they’re doing. You think your FDA guidelines are superior? Please. We have over a billion people. We don’t have time for your overcautious, over-medicated, over-analyzed Western nonsense. Tramadol is cheap. It works. Stop scaring people with your lab reports.
vinoth kumar
December 7, 2025 AT 20:36Just wanted to add - I’m on sertraline and take oxycodone for chronic back pain. Been doing it for 3 years. No issues. But I check in with my pharmacist every time I refill. He uses this free drug interaction checker called Lexicomp. It’s free on their app. I screenshot the green light every time and show my doctor. Simple. No drama. And I’ve told 3 friends to do the same. Knowledge is power, not fear.
bobby chandra
December 8, 2025 AT 07:10This isn’t just medical advice - it’s a survival guide. Imagine your brain as a serotonin party. SSRIs are the bouncers letting more people in. Opioids like tramadol? They’re the guy who brings a keg of pure serotonin juice and starts pouring it into everyone’s cup. Now imagine that party in a tiny closet. That’s serotonin syndrome. Not a glitch. Not a side effect. A full-blown neurological riot. And the worst part? The ER docs don’t even know what they’re looking at half the time. This post is the fire alarm. Listen to it.
Archie singh
December 9, 2025 AT 11:51Tramadol is a controlled substance for a reason. SSRIs are not toys. The fact that this is even a debate shows how broken our healthcare system is. Doctors prescribe like they’re ordering coffee. No follow-up. No education. Just scribble and send. If you’re on an SSRI and your pain doc gives you tramadol without checking your med list - fire them. No exceptions. This isn’t opinion. It’s negligence.
Gene Linetsky
December 10, 2025 AT 13:34They’re hiding something. Why does the FDA only warn about tramadol and not fentanyl? Because the opioid manufacturers pay off the regulators. Look at the 120+ fentanyl cases - all ignored. Why does fluoxetine have a 5-week waiting period but other SSRIs don’t? Because they’re testing on poor people in India and Africa. This isn’t science. It’s corporate control. Your antidepressant is a leash. Your painkiller? A trap. Wake up.