TL;DR:
- Chloroquine is an old antimalarial drug now also used for some autoimmune conditions.
- It works by raising the pH inside parasite‑infected cells, stopping the parasite from growing.
- Common side effects include nausea, headache and retinal toxicity with long‑term use.
- Standard malaria dose: 600mg on day1, then 300mg on days2‑3; dosage differs for rheumatoid arthritis.
- COVID‑19 studies show no clear benefit; major health agencies advise against routine use.
What Is Chloroquine and How Does It Work?
Chloroquine is a synthetic compound first synthesized in the 1930s. It gained fame as a cheap, effective treatment for Plasmodium malaria, especially the strains that were still sensitive to the drug in the 1950s. Over time, doctors discovered it also dampens the immune system, so it earned a second life treating autoimmune diseases like lupus and rheumatoid arthritis.
The magic lies in chemistry: chloroquine is a weak base that piles up in acidic organelles-think lysosomes and the parasite’s food vacuole. By raising the pH, it messes up the parasite’s ability to digest hemoglobin, essentially starving it. In autoimmune conditions, the same pH shift interferes with antigen presentation, reducing inflammation.
"Chloroquine’s dual action-antiparasitic and immunomodulatory-makes it a unique tool in the pharmacological toolbox," notes Dr. Margaret Chan, former WHO Director‑General.
Because the drug accumulates in tissues, especially the retina, clinicians monitor patients closely for eye toxicity.
Approved Uses: From Malaria to Autoimmune Disorders
In 2025, chloroquine is officially approved for two main indications:
- Uncomplicated malaria caused by chloroquine‑sensitive P. vivax and P. ovale.
- Rheumatoid arthritis and systemic lupus erythematosus where it serves as a steroid‑sparing agent.
Off‑label, it sometimes appears in dermatology for severe psoriasis and in certain viral research labs, but those uses lack robust regulatory backing.
For malaria, the World Health Organization (WHO) still lists chloroquine as a first‑line drug only in regions where resistance is absent-namely parts of Central America and Oceania. In Australia, chloroquine is stocked in most hospital pharmacies for travelers returning from endemic zones.
Dosage Guidelines and Administration Tips
Getting the dose right is crucial. Below is a quick‑reference table for the most common regimens.
| Indication | Typical Adult Dose | Duration | Key Monitoring |
|---|---|---|---|
| Uncomplicated malaria (chloroquine‑sensitive) | 600mg (base) on Day1, then 300mg on Days2&3 | 3 days | Blood smear on Day3, liver function |
| Rheumatoid arthritis (maintenance) | 250mg daily (often split 125mg BID) | Indefinite, reassess every 3‑6 months | Retinal exam, CBC, electrolytes |
| Lupus (maintenance) | 250mg daily (adjust for weight) | Long‑term | Eye exam, renal function |
Tips to minimise side effects:
- Take the tablet with food or a full glass of water to reduce stomach upset.
- Never crush or chew extended‑release forms; they’re designed for slow release.
- Schedule a baseline ophthalmology exam before starting long‑term therapy, then annually.
- Stay hydrated-chloroquine can cause mild diuresis.
If you miss a dose, take it as soon as you remember unless it’s within 12hours of the next scheduled dose; then skip and continue as normal.

Safety Profile: Side Effects, Interactions & the COVID‑19 Controversy
Like any drug, chloroquine isn’t risk‑free. Here’s what patients most often report:
| Side Effect | Frequency | Typical Onset |
|---|---|---|
| Nausea / vomiting | 10‑20% | Within 1hour |
| Headache | 5‑15% | First 2days |
| Retinal toxicity (long‑term) | ~1% after >5years | Months‑years |
| Cardiac QT prolongation | Rare (<1%) | Within 48hours, especially with other QT‑prolonging drugs |
Major drug interactions include:
- Antacids (reduce absorption).
- QT‑prolonging agents like azithromycin, hydroxychloroquine, certain anti‑psychotics.
- Cytochrome P450 inhibitors (e.g., erythromycin) can raise plasma levels.
Because of its effect on the heart rhythm, clinicians avoid prescribing chloroquine to patients with known arrhythmias or those on multiple QT‑prolonging meds.
COVID‑19: What the Science Says (2025 Update)
Early 2020 hype made headlines when a small French study suggested chloroquine might cut viral load. That spurred a global scramble, but larger, well‑controlled trials quickly knocked the hype down.
Key findings up to 2025:
- The RECOVERY trial (UK) enrolled >10,000 hospitalised patients and found no mortality benefit.
- The WHO SOLIDARITY trial halted the chloroquine arm early due to lack of efficacy and safety concerns.
- Meta‑analyses published in The Lancet and JAMA conclude that routine chloroquine or hydroxychloroquine use for COVID‑19 is not recommended.
Both the WHO and the U.S. CDC now list chloroquine as “not recommended for COVID‑19 treatment outside clinical trials.” In Australia, the Therapeutic Goods Administration (TGA) issued a reminder in March2024 that prescribing chloroquine for COVID‑19 without trial enrolment may expose patients to unnecessary risk.
Bottom line: if you’re looking for a COVID‑19 cure, chloroquine isn’t it. Stick to approved antivirals and supportive care.
Frequently Asked Questions
- Can I take chloroquine with alcohol? Small amounts won’t change the drug’s action, but heavy drinking can worsen liver toxicity.
- Is chloroquine safe in pregnancy? It’s classified as Category C in Australia - only use if benefits outweigh risks, typically under specialist supervision.
- Why do I need an eye exam? Long‑term accumulation in the retina can cause irreversible vision loss; early detection makes a huge difference.
- Is hydroxychloroquine the same? Hydroxychloroquine is a newer analogue with a slightly better safety profile, especially for eye toxicity, but it works the same way.
- Can I store chloroquine at home? Keep it in a cool, dry place, out of reach of children, and never use after the expiry date printed on the label.
Next Steps & Troubleshooting
If you’re starting chloroquine for malaria prophylaxis before a trip:
- Consult your GP 1‑2weeks before departure.
- Get baseline liver function tests.
- Follow the dose schedule (usually 300mg weekly).
- Carry a copy of the prescription in case you need refills abroad.
For chronic users (lupus or arthritis) who develop visual changes:
- Stop the drug immediately.
- Book an urgent ophthalmology appointment.
- Discuss alternative disease‑modifying agents with your rheumatologist.
Experiencing severe nausea or heart palpitations? Call your doctor right away; dose adjustment or a switch to hydroxychloroquine might be needed.
Remember, any medication works best when you pair it with regular monitoring and open communication with your healthcare team.

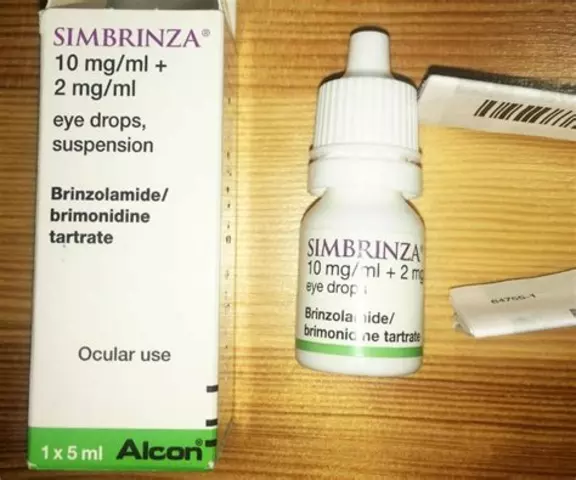 Tips for ensuring proper hygiene while using brimonidine tartrate eye drops
Tips for ensuring proper hygiene while using brimonidine tartrate eye drops
 Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
 Levofloxacin for Anthrax: What You Need to Know
Levofloxacin for Anthrax: What You Need to Know
 Bioavailability Studies for Generics: What They Test and Why It Matters for FDA Approval
Bioavailability Studies for Generics: What They Test and Why It Matters for FDA Approval
 Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
Naomi Ho
September 21, 2025 AT 00:06Chloroquine still works great for malaria in places where the parasite isn’t resistant it’s cheap and you just need the three‑day course
Christine Watson
September 21, 2025 AT 01:46Got a trip coming up? If the destination still has chloroquine‑sensitive malaria you can feel confident that the standard three‑day regimen will protect you. Make sure you book a pre‑travel appointment so you get the right dose and a baseline eye check. Staying hydrated and taking the tablets with food really helps minimize nausea. And remember, the drug is cheap and widely available, which is a huge plus for budget travelers.
Macy Weaver
September 21, 2025 AT 04:00I’ve been following the recent guidelines and what I’ve seen is that chloroquine is still a solid option for uncomplicated malaria when resistance isn’t an issue. For autoimmune patients the low‑dose daily schedule can be effective, but you have to keep an eye on retinal health with regular exams. It’s also worth noting that the drug interacts with some cardiac meds, so a quick medication review is wise. In practice, I’ve found the side‑effect profile tolerable if you start with meals and stay on the recommended dose. If you ever feel persistent headaches or visual changes, reach out to your rheumatologist sooner rather than later.
James McCracken
September 21, 2025 AT 06:13One might argue that the allure of chloroquine lies not merely in its pharmacodynamics but in its symbolic resonance as a relic of colonial medicine. While the molecule dutifully raises lysosomal pH, our collective imagination projects it onto the canvas of pandemics, eager for a panacea. Yet the data, like an inexorable tide, erodes the myth, leaving behind a sober reminder of hubris. The very act of repurposing a drug without rigorous evidence betrays a philosophical laziness. In the grand theatre of therapeutics, chloroquine is but a supporting actor, not the protagonist. Its story cautions us to respect the epistemic boundaries that separate anecdote from science.
Evelyn XCII
September 21, 2025 AT 08:10Oh sure, just pop some chloro‑qine and the virus will vanish – because that’s how meds work, right?
Suzanne Podany
September 21, 2025 AT 10:06Hey folks, if you’re starting chloroquine for lupus or rheumatoid arthritis, remember it’s a team effort. Schedule that baseline eye exam and keep a log of any visual changes – early detection makes a world of difference. Pair the medication with a balanced diet and stay well‑hydrated; it can help with the mild diuretic effect. If nausea hits, taking the pill with a solid meal usually eases it. And don’t hesitate to reach out to your healthcare team; open communication is key to staying safe and effective on long‑term therapy.
Nina Vera
September 21, 2025 AT 12:20The saga of chloroquine reads like a dramatic opera, an underdog rising from the dusty labs of the 1930s to the global stage of modern medicine. It first dazzled the world by crushing malaria parasites with a simple three‑day regimen, saving countless lives in remote villages. Then, like an actor discovering a new role, it slipped onto the autoimmune stage, calming the fierce fires of lupus and rheumatoid arthritis. Doctors marveled at its dual nature, a paradoxical blend of parasite‑killing and immune‑modulating powers. But fame, as always, brings shadows; whispers of retinal toxicity began to echo through ophthalmology clinics. The organ‑preserving eye exams became a ritual, a solemn reminder that even heroes can have hidden flaws. When the COVID‑19 pandemic erupted, the world once again turned its gaze to chloroquine, hoping for a miracle. Headlines shouted, “Cure in a pill!” while scientists rolled up their sleeves for rigorous trials. The trials, however, told a sober tale – no clear benefit, and some concerning cardiac signals. The WHO, CDC, and TGA sounded the alarm, urging restraint and caution. Yet the public imagination held on, fueled by celebrity endorsements and social media hype. In the end, chloroquine returned to its modest niche, respected for what it truly offers and not what fantasies project onto it. Its legacy reminds us that medicine is a balance of hope, evidence, and humility. So let us honor its contributions, learn from its missteps, and keep searching for the next true breakthrough.
Christopher Stanford
September 21, 2025 AT 14:33Reading the latest meta‑analysis makes me wonder if anyone actually read the fine print. The statistical methods were sloppy, confidence intervals overlapped, and yet they still claim “no benefit.” It feels like a classic case of data dredging, where researchers fish for significance while ignoring real‑world toxicity signals. If you’re going to push chloroquine as a COVID‑19 solution, at least present a transparent risk‑benefit analysis. Otherwise, you’re just spouting buzzwords and hoping the public won’t notice the gaps.
Steve Ellis
September 21, 2025 AT 16:30Listen up team, chloroquine isn’t a magic bullet but it’s a solid tool when used correctly. For malaria prophylaxis, stick to the weekly 300 mg dose and you’ll stay ahead of the parasite. If you’re on a chronic regimen for arthritis, keep those eye exams on schedule – think of them as your performance check‑ups. When side effects creep in, adjust the timing or talk to your doctor – never just power through. Remember, consistency and communication are the real champions in any treatment plan.
Jennifer Brenko
September 21, 2025 AT 18:26It is imperative to recognize that the indiscriminate promotion of chloroquine by foreign entities reflects a misguided attempt to undermine our national health protocols. Our regulatory bodies have conducted rigorous evaluations and rightly concluded that routine use for COVID‑19 is unsupported by evidence. Any deviation from these guidelines not only jeopardizes individual safety but also threatens the integrity of our public health strategy. We must remain vigilant against external pressures that seek to dilute scientifically sound practices.
Harold Godínez
September 21, 2025 AT 20:40Good point about the stats – I noticed they didn’t adjust for age or comorbidities either. A quick re‑run with those covariates would probably change the outcome.
Sunil Kamle
September 21, 2025 AT 22:53Indeed, one might contend that adherence to dosing schedules is a trivial concern when the underlying therapeutic premise is fundamentally flawed. Nevertheless, let us not abandon basic pharmacological principles in our quest for novelty.
Michael Weber
September 22, 2025 AT 00:50The narrative you crafted elegantly captures the duality of chloroquine, yet it omits the ethical dimension of prescribing a drug with known retinal risks. A clinician’s duty extends beyond mere efficacy; it encompasses foresight into long‑term sequelae. By integrating vigilant ophthalmologic monitoring, we reconcile therapeutic ambition with moral responsibility.
Blake Marshall
September 22, 2025 AT 02:46actually u should know that chloroqine interacts with antacids so take it with water not milk its also not great if u have heart problems
Shana Shapiro '19
September 22, 2025 AT 05:00I understand the frustration when a drug is highlighted in headlines without clear proof. It can feel like a let‑down for those hoping for a quick solution. Patience and reliance on thorough research remain our best allies.
Jillian Bell
September 22, 2025 AT 07:13Some people think the whole chloroquine debate is a distraction engineered by hidden powers to keep the public confused while larger agendas unfold behind the scenes.
Lindsey Bollig
September 22, 2025 AT 09:26Thanks for the travel tips! I always make sure to get the eye exam before starting a long trip and I keep a water bottle handy to stay hydrated – it really does help with the mild diuretic effect.