PPI-Clopidogrel Interaction Calculator
How PPIs Affect Clopidogrel Effectiveness
Omeprazole and other PPIs can reduce clopidogrel's effectiveness by inhibiting the CYP2C19 enzyme needed to activate it. This calculator estimates the percentage reduction in clopidogrel activity based on your PPI choice and genetic metabolism status.
Estimated Clopidogrel Effectiveness
100% of clopidogrel's antiplatelet activity will be available.
When you take omeprazole and clopidogrel together, something subtle but powerful happens inside your liver. It’s not a side effect you can feel. No nausea, no dizziness. Just a quiet drop in how well clopidogrel works to stop blood clots. And that’s dangerous if you’ve had a heart attack or stent placed.
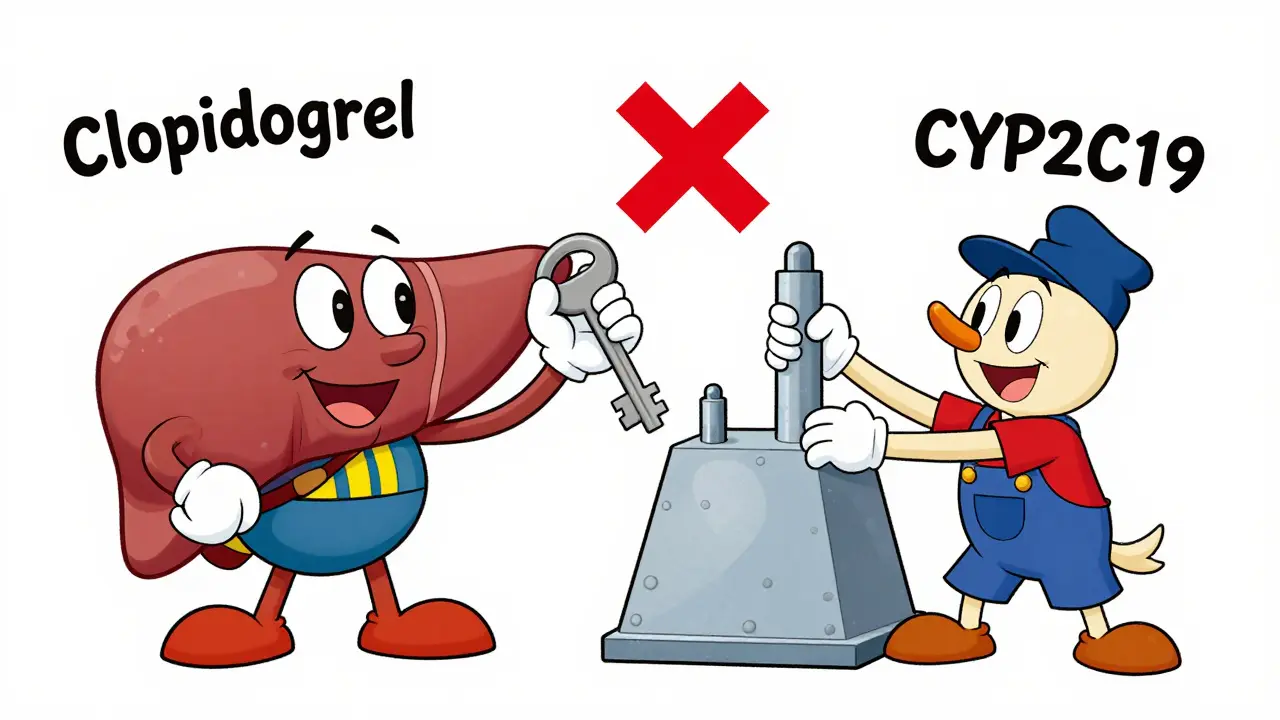
Why Clopidogrel Needs Your Liver
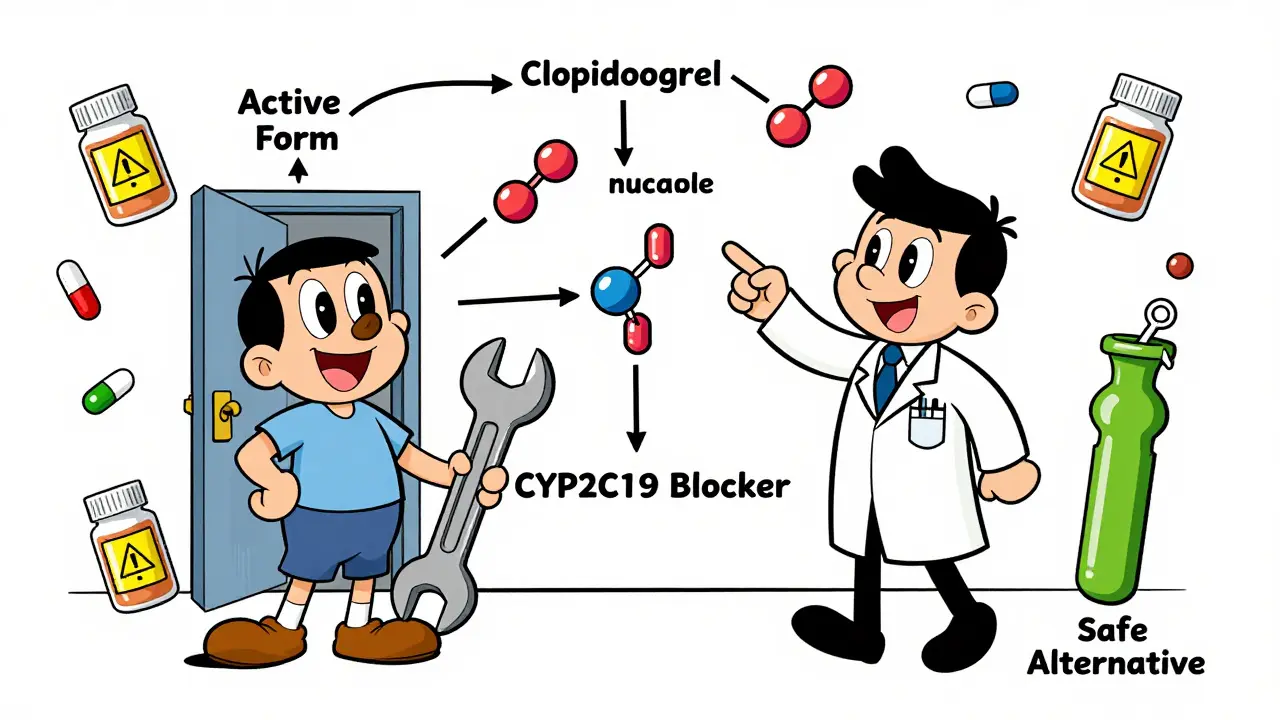
Clopidogrel doesn’t work right away. It’s a prodrug-meaning your body has to turn it into something active. That job falls to an enzyme called CYP2C19. This enzyme does two key steps to unlock clopidogrel’s ability to block platelets. Without it, clopidogrel is basically useless. Think of it like a key that needs to be cut before it can turn a lock. Omeprazole doesn’t just sit beside this process-it steps in and jams the cutting machine.How Omeprazole Sabotages the Process
Omeprazole is designed to be broken down by CYP2C19. But while it’s being processed, it latches onto the enzyme so tightly that clopidogrel can’t get a turn. Studies show that a daily 80mg dose of omeprazole cuts the active form of clopidogrel in your blood by nearly half. Even the standard 20mg dose knocks it down by 32%. This isn’t theoretical-it’s measured in plasma levels, platelet function tests, and real-world outcomes.The problem isn’t just omeprazole. Its close relative, esomeprazole (the S-isomer), does almost the same thing. Both are strong inhibitors. But not all PPIs are equal. Pantoprazole barely touches CYP2C19. Rabeprazole has a mild effect. And ilaprazole? It barely registers. This isn’t just about brand names-it’s about chemistry. Omeprazole has a Ki,u value of 1.5-2.3 μM, meaning it binds with high affinity. Pantoprazole’s is over 10 times weaker. That’s why guidelines now treat them differently.
The Clinical Debate: Does It Actually Hurt Patients?
Here’s where things get messy. Lab tests clearly show reduced clopidogrel activity. But do those changes lead to more heart attacks or strokes? Some studies say yes. A 2014 meta-analysis of over 270,000 patients found a 27% higher risk of cardiovascular events with PPI use-mostly driven by omeprazole. The risk jumped to 33% with omeprazole alone.But then came the COGENT trial. This was a randomized, controlled study of nearly 4,000 patients. Half took omeprazole with clopidogrel. Half didn’t. After a year, there was no difference in heart attacks, strokes, or death. The same was true in the FAST-MI registry, which tracked over 2,700 patients. No increased risk.
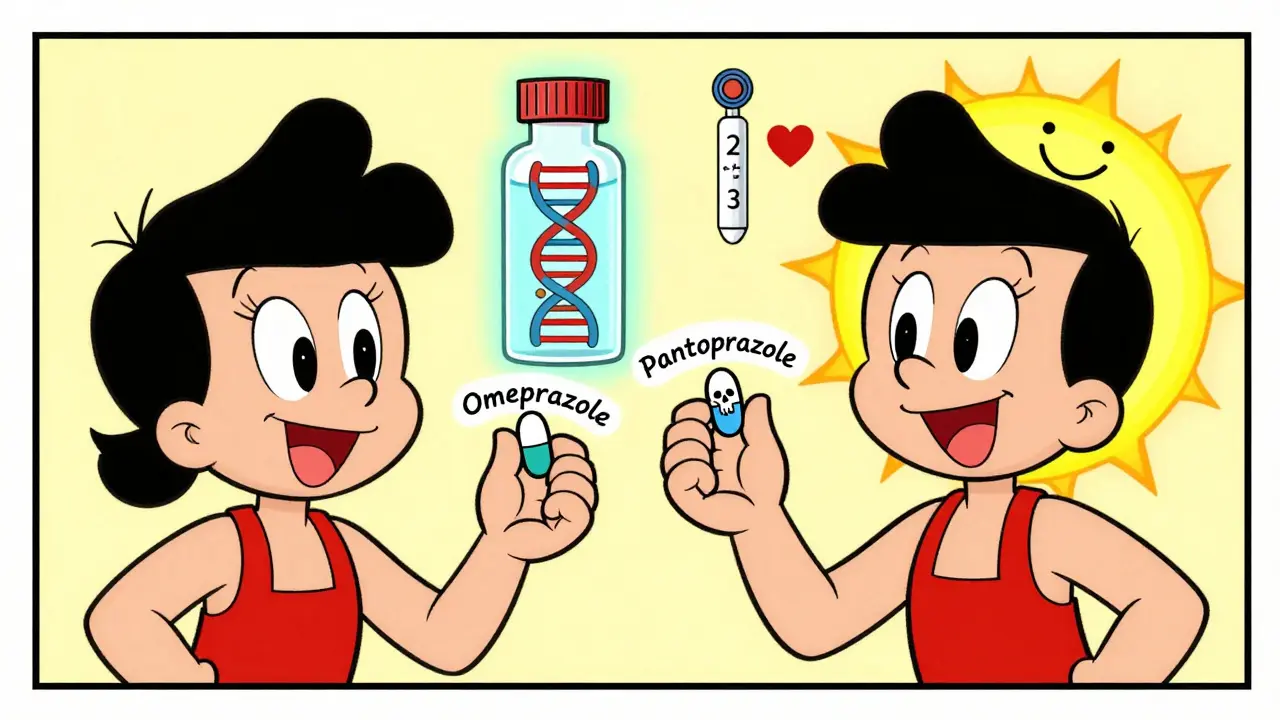
So why the contradiction? One big clue: genetics. About 30% of East Asians and 20-25% of Caucasians carry a genetic variant (CYP2C19*2 or *3) that already reduces enzyme activity. In these people, adding omeprazole doesn’t just reduce clopidogrel’s effect-it can nearly eliminate it. A Korean study found that in normal metabolizers, omeprazole cut clopidogrel response by 32%. In intermediate metabolizers? It dropped by 54%. That’s not a minor tweak-it’s a treatment failure.
What the Guidelines Actually Say
The American Heart Association, European Society of Cardiology, and FDA all agree: avoid omeprazole and esomeprazole with clopidogrel. The FDA’s 2009 safety warning was blunt. The EMA’s 2023 label says: “Concomitant use is not recommended.”But they don’t say avoid all PPIs. Pantoprazole is the go-to alternative. At 40mg daily, it reduces clopidogrel exposure by only 14%-a level most experts consider clinically insignificant. Rabeprazole is a second option. H2 blockers like famotidine can also be used if you need acid protection but want to avoid PPIs entirely.
And here’s something most patients don’t know: timing doesn’t help. Taking clopidogrel in the morning and omeprazole at night? Doesn’t matter. The inhibition happens in the liver, not the gut. The enzyme doesn’t care when the drugs arrive-it’s busy either way.
What Should You Do?
If you’re on clopidogrel and need a PPI, here’s what works:- Avoid omeprazole and esomeprazole completely.
- Switch to pantoprazole 40mg daily. It’s the safest choice.
- If pantoprazole isn’t available, rabeprazole 20mg daily is acceptable.
- Ask about famotidine (H2 blocker) if your stomach issues aren’t severe.
- If you’ve had a stent or heart attack and have a family history of clotting issues, ask for CYP2C19 genotyping.
Genotyping isn’t routine everywhere-but it’s becoming more common. According to the ACC’s 2023 data, 74% of U.S. cardiology practices now offer some form of pharmacogenetic testing. If you’re a poor or intermediate metabolizer, you’re better off switching to prasugrel or ticagrelor entirely. These drugs don’t rely on CYP2C19. They’re more expensive, yes-but they’re not easily blocked by PPIs.
The Bigger Picture
Since the FDA warning in 2009, prescriptions for omeprazole with clopidogrel dropped by 65% in the U.S. Pantoprazole use jumped 42%. That’s real-world impact. The pharmaceutical industry noticed. Newer antiplatelet drugs like ticagrelor and prasugrel were designed to avoid this exact problem. And now, researchers are testing next-gen PPIs like ilaprazole that barely touch CYP2C19 at all.This isn’t just about two drugs. It’s about how we think about medication safety. We used to assume if a drug was approved, it was safe with everything else. Now we know: metabolism matters. Genetics matter. Enzyme competition matters. The future of medicine isn’t just prescribing pills-it’s understanding how your body processes them.
What If You’re Already Taking Both?
Don’t stop clopidogrel. That’s dangerous. Don’t stop omeprazole cold turkey if you’re on it for ulcers or GERD-sudden rebound acid can cause real harm. Talk to your doctor. Ask:- Can I switch to pantoprazole?
- Should I get tested for CYP2C19 variants?
- Is there a non-PPI option for my stomach?
If you’re on clopidogrel because of a stent or recent heart attack, this conversation isn’t optional. It’s essential.
Can I take omeprazole with clopidogrel if I take them at different times of day?
No. Taking clopidogrel in the morning and omeprazole at night doesn’t prevent the interaction. Both drugs are processed by the same liver enzyme, CYP2C19. The inhibition happens at the metabolic level, not the gut level. Timing doses apart has no meaningful effect on reducing the interaction.
Is pantoprazole really safer than omeprazole with clopidogrel?
Yes. Studies show pantoprazole reduces clopidogrel’s active metabolite by only about 14%, compared to 32-49% with omeprazole. Its inhibition of CYP2C19 is weak, and its Cmax,u/Ki,u ratio is below the FDA’s threshold for clinical concern. It’s the recommended alternative in guidelines from the American College of Gastroenterology and the American Heart Association.
Do all PPIs interfere with clopidogrel the same way?
No. PPIs vary widely in how strongly they inhibit CYP2C19. Omeprazole and esomeprazole are the strongest. Lansoprazole has moderate inhibition at high doses. Rabeprazole is mild. Pantoprazole is very weak. Ilaprazole, a newer PPI, shows almost no inhibition. The difference isn’t just small-it’s clinically decisive.
Should I get tested for CYP2C19 gene variants?
If you’re on clopidogrel after a heart attack, stent, or stroke-and especially if you’re of East Asian descent-it’s worth asking. About 30% of East Asians and 20-25% of Caucasians carry loss-of-function alleles (*2 or *3) that reduce clopidogrel’s effectiveness. If you’re one of them, adding omeprazole can push your antiplatelet response into dangerous territory. Testing helps guide safer choices like prasugrel, ticagrelor, or pantoprazole.
What are my alternatives to clopidogrel if I need a PPI?
Prasugrel and ticagrelor are the two main alternatives. Neither relies on CYP2C19 to become active, so they’re not affected by omeprazole or other PPIs. Ticagrelor is taken twice daily and has a faster onset. Prasugrel is once daily but carries a higher bleeding risk. Both are more expensive than clopidogrel, but they’re more reliable when you need to take acid-reducing medication.
 Buy Cheap Generic Amoxicillin Online - Australian Guide 2025
Buy Cheap Generic Amoxicillin Online - Australian Guide 2025
 Clotting Disorders and Anticoagulation: Understanding INR, DOACs, and Safety
Clotting Disorders and Anticoagulation: Understanding INR, DOACs, and Safety
 Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
Compare Isoptin (Verapamil) with Alternatives: What Works Best for Heart Conditions
 Ventolin vs. Levalbuterol: A Detailed Clinical Comparison of Modern Inhalers
Ventolin vs. Levalbuterol: A Detailed Clinical Comparison of Modern Inhalers
 Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Lee M
January 2, 2026 AT 08:00They say metabolism is destiny, but really it's just biochemistry playing chess with your life. You take a pill thinking it's helping, but deep in your liver, enzymes are getting mugged by proton pumps. And the worst part? You feel fine. No warning lights. Just a silent, creeping failure of your own biology to protect you. This isn't conspiracy-it's pharmacokinetics with consequences.
Austin Mac-Anabraba
January 4, 2026 AT 01:48Let’s be precise: omeprazole’s Ki,u of 1.5–2.3 μM against CYP2C19 is not merely ‘strong’-it’s competitive inhibition at its most insidious. The FDA’s 2009 warning wasn’t a suggestion; it was a pharmacological red flag. Pantoprazole’s Cmax,u/Ki,u ratio of <0.1 satisfies the threshold for negligible interaction. Any clinician who ignores this is either negligent or misinformed. No ambiguity. No ‘maybe.’ This is textbook drug-drug interaction.
Phoebe McKenzie
January 4, 2026 AT 15:48THIS IS WHY PEOPLE ARE DYING IN THEIR KITCHENS. You think your heart attack came from stress? Nah. It came from your doctor handing you omeprazole like it was aspirin while you were on clopidogrel. I’ve seen it. My uncle. 62. Stent. Prescribed omeprazole for ‘heartburn.’ Died six months later. No one told him. No one warned him. And now? They want to talk about ‘guidelines’ like that’s some kind of apology. It’s not. It’s negligence dressed in white coats.
gerard najera
January 4, 2026 AT 19:35Genetics decide who lives. Enzymes decide how.
Stephen Gikuma
January 5, 2026 AT 12:43Big Pharma knew this all along. They pushed omeprazole because it’s cheap. They knew clopidogrel’s efficacy dropped. But they didn’t care-until the lawsuits started. Now they’re pushing ‘safer’ PPIs and expensive new drugs. Same game. Different labels. The system doesn’t fix problems-it monetizes them. And you? You’re just the cash register.
Bobby Collins
January 5, 2026 AT 13:09wait so are they saying the government is lying to us about heart meds?? like... is this why my cousin got a second stent?? i thought it was just bad luck 😔
Layla Anna
January 6, 2026 AT 04:30thank you for writing this so clearly 💛 i had no idea timing didn't matter... i was so proud of myself for taking my meds at different times 😅 but now i'm scared... my doc gave me omeprazole last week... should i call them or just wait? i don't want to panic but... i also don't want to die
Heather Josey
January 7, 2026 AT 03:39This is an excellent, evidence-based breakdown. Thank you for highlighting the critical distinction between PPIs and the importance of pharmacogenetics. For patients on clopidogrel, switching to pantoprazole is not just a suggestion-it’s a standard of care. If your provider hasn’t discussed this, please advocate for yourself. Your life depends on it. And if you’re unsure, ask for a referral to a clinical pharmacist. They’re trained for exactly this kind of interaction.
Donna Peplinskie
January 8, 2026 AT 19:06Thank you so much for sharing this-it’s so important, and I’m so glad you included the alternatives. I’ve been on clopidogrel since my stent, and my GI doc just gave me omeprazole without a word... I’m going to call my cardiologist first thing tomorrow. I also have family from Korea, so I’m definitely asking about the gene test. I feel like I’ve been sleeping through this, and now I’m awake. Thank you for waking me up 💛
Olukayode Oguntulu
January 9, 2026 AT 02:49One must acknowledge the epistemological rupture between clinical pharmacology and patient autonomy. The CYP2C19 axis represents a hegemonic reductionism-pharmaco-kinetic determinism masquerading as medical authority. One wonders: who benefits from this narrative? The pharmaceutical complex? The regulatory apparatus? Or the medical-industrial complex that thrives on iatrogenic sequelae? The data may be statistically significant, but the ontology remains unexamined. One must ask: is safety truly the goal-or merely compliance?
jaspreet sandhu
January 9, 2026 AT 12:34I read all this and I think most people are overcomplicating it. In India we give clopidogrel and omeprazole together all the time and patients don't die. Maybe it's different for rich countries with fancy labs and genetic tests. Here we have people who can't even afford aspirin, let alone gene testing. We use what works. If the patient is fine, why change? Maybe the problem is not the drug, but the fear of drugs. People think every pill is poison. I think we should stop being scared and just take what the doctor says. Simple.
Alex Warden
January 9, 2026 AT 15:20Look, I don't care what some lab says. I'm American. I take what I need. If I need acid relief and I need blood thinners, I'll take both. I don't need some PhD in a lab coat telling me my liver can't handle it. This is America. We don't get scared of pills. We take them and we live. The real threat is overregulation and fearmongering. Stop scaring people with science they don't understand.
LIZETH DE PACHECO
January 10, 2026 AT 08:04Thank you for this. I’ve been on clopidogrel for 3 years after my heart attack. My doctor gave me omeprazole last year and I never questioned it. I’m scheduling a call with my cardiologist this week to ask about pantoprazole and testing. I’m not scared-I’m just ready to do better. You made me feel like I can ask the right questions without sounding paranoid. That means a lot.
Kristen Russell
January 10, 2026 AT 20:37So… if I’m on clopidogrel, and I need a PPI, and I can’t get pantoprazole… what’s the worst that could happen? I die? Maybe. But I also might not. And if I do, at least I didn’t suffer from acid reflux. Life is a risk. Medicine is a gamble. I’d rather have a quiet stomach than a perfect platelet count. Let’s stop pretending this is black and white. It’s not. It’s gray. And gray is where real life lives.