RA Treatment Cost Calculator
Medication Selection
Cost Estimate
When you’re living with rheumatoid arthritis (RA), the goal isn’t just to manage pain-it’s to stop the damage before it steals your mobility. That’s where DMARDs and biologics come in. These aren’t just painkillers. They’re disease-modifying tools designed to slow or even halt the immune system’s attack on your joints. But mixing them isn’t simple. Getting the combination right can mean the difference between staying active and ending up in a wheelchair.
What Are DMARDs, Really?
Disease-modifying antirheumatic drugs (DMARDs) are the foundation of RA treatment. They’re not new. Methotrexate, the most common one, was originally developed in the 1950s as a cancer drug. Doctors noticed patients with arthritis had less swelling, and the rest is history. Today, methotrexate is taken weekly-usually as a pill or injection-and works by calming down overactive immune cells. It’s cheap, effective, and used in about 85% of new RA cases. Other traditional DMARDs include sulfasalazine, hydroxychloroquine, and leflunomide. These aren’t targeted. They’re like a broad net thrown over the immune system. That’s why side effects like nausea, fatigue, and liver stress happen. But for many, especially early in the disease, they work well enough. Studies show methotrexate alone puts about 20-30% of early RA patients into remission. That’s not perfect, but it’s better than nothing.Biologics: Precision Weapons Against RA
Biologics changed the game in the late 1990s. Unlike traditional DMARDs, they’re made from living cells and designed to hit one specific target in the immune system. Think of them as smart missiles instead of bombs. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) block tumor necrosis factor, a key inflammation driver. Rituximab wipes out B cells. Tocilizumab shuts down interleukin-6 signaling. Abatacept stops T cells from getting activated. Each one has a different job, and your doctor picks based on your symptoms, blood markers, and how you’ve responded to other drugs. They’re given as injections or IV infusions because they’re large proteins that would get broken down in the stomach if taken as pills. That means more visits to the clinic or learning to give yourself shots. Training takes a couple of sessions, but 85% of patients master it after just one or two tries.Why Methotrexate Is the Anchor
Here’s the key point most people miss: biologics work better when paired with methotrexate. It’s not optional-it’s standard. A 2015 study showed that when biologics are used alone, about 30-40% of patients hit a 50% improvement in symptoms (called ACR50). But when combined with methotrexate, that jumps to 50-60%. That’s a huge difference in real life: less swelling, less joint damage, fewer flares. Why? Methotrexate helps your body tolerate the biologic. It reduces the chance your immune system will see the biologic as a foreign invader and attack it, making it less effective. It also seems to boost the biologic’s ability to suppress inflammation. But not everyone can take methotrexate. About 20-30% of patients have nausea, liver issues, or just can’t handle it. In those cases, doctors may try other DMARD combinations or switch to a biologic alone. Some patients do well on biologic monotherapy, especially if they’ve had bad reactions to methotrexate in the past.Cost: The Hidden Battle
Methotrexate costs $20-$50 a month. A biologic? $1,500-$6,000. That’s not a typo. Even with insurance, co-pays can hit $500 a month. That’s why nearly 30% of RA patients skip doses or stop taking their meds because of cost. The Arthritis Foundation found that 28% of people on biologics didn’t take them as prescribed because of money. Biosimilars changed that. After 2016, copies of Humira and Enbrel hit the market. Amjevita, Cyltezo, and others are chemically nearly identical to the originals but cost 15-30% less. By 2023, biosimilars made up 28% of the U.S. biologic market. For many, this is the only way they can stay on treatment.
JAK Inhibitors: The Oral Alternative
JAK inhibitors like tofacitinib, baricitinib, and upadacitinib are a newer class. They’re not biologics. They’re small-molecule pills that block internal signaling pathways in immune cells. That means they’re taken orally-no shots, no infusions. They’re also faster-acting than biologics, often showing results in weeks, not months. The 2023 FDA approval of upadacitinib for early RA was a big deal. It was the first JAK inhibitor shown to be as effective as methotrexate alone. That opens the door for patients who can’t take methotrexate and don’t want injections. But there’s a catch. In 2021, the FDA added a black box warning to all JAK inhibitors after a study showed higher risks of serious infections, heart attacks, strokes, and cancer-especially in patients over 50 with existing risk factors. So doctors now weigh the benefits against these dangers. For a young patient with aggressive RA, the trade-off might be worth it. For an older patient with high blood pressure and a history of skin cancer? Maybe not.Real-World Choices: What Patients Actually Do
In clinical trials, everything looks neat: clear groups, controlled doses, perfect compliance. Real life? Messy. A 2022 Reddit thread with 147 RA patients showed 63% chose biologic + methotrexate combo despite side effects. Why? They said, “I can finally walk to the mailbox.” The other 37% went with methotrexate alone or switched to a biologic alone because nausea and fatigue from methotrexate were unbearable. In countries like India, where a biologic can cost 300-500% of a monthly household income, doctors rely on triple DMARD therapy-methotrexate, sulfasalazine, and hydroxychloroquine. Studies show this combo can match biologics in slowing joint damage over two years. And then there’s the data: 32.7% of RA patients on biologics in Switzerland were on them alone. The main reason? Methotrexate intolerance. Not because it didn’t work-because they couldn’t stand it.When to Switch or Add
Treatment isn’t static. It’s a step-by-step process called “treat-to-target.” You start with methotrexate. After 3-6 months, your doctor checks your disease activity. If you’re still in pain, swelling, or have rising blood markers, you don’t wait. You escalate. That means adding a biologic or switching to a JAK inhibitor. The 2021 ACR guidelines say: don’t wait a year. Don’t hope it gets better. Act. Early intervention saves joints. But here’s the twist: some studies, like CAMERA-II and CAMERA-III, show that triple DMARD therapy can match adalimumab in long-term outcomes. So if you’re hesitant about biologics or cost is a barrier, a strong combo of traditional DMARDs might be just as effective.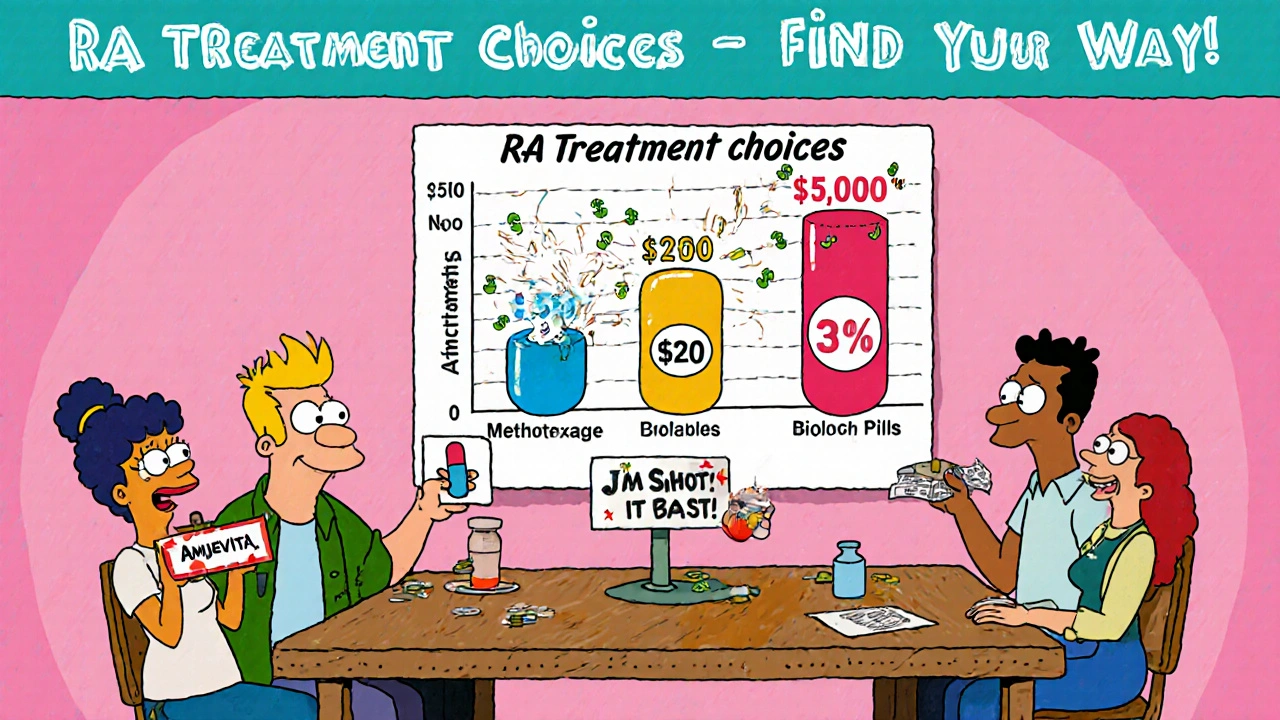
Monitoring and Safety
All these drugs suppress your immune system. That means infections are the biggest risk. TB screening is required before starting any TNF inhibitor. Blood tests every 1-3 months check liver function, blood counts, and kidney health. Biologics increase risk of serious respiratory infections. One in five patients on these drugs report needing antibiotics for pneumonia or bronchitis. Injection site reactions-redness, itching, swelling-are common with subcutaneous drugs but usually mild. JAK inhibitors come with their own warnings: higher risk of blood clots, especially in people over 50, and possible links to lymphoma. That’s why they’re not first-line for older patients with heart disease.What’s Next?
The future is moving toward more targeted drugs. New biologics are being tested against GM-CSF, a different inflammation signal. Deucravacitinib, a more selective JAK inhibitor, might offer the benefits of oral treatment without the same cancer risks. Ultrasound and MRI are now being used to measure remission-not just how you feel, but whether the inflammation inside your joints has truly quieted. The 2024 draft of the ACR guidelines now includes imaging remission as a goal. That means treatment will get even more personalized.Frequently Asked Questions
Can I take biologics without methotrexate?
Yes, but it’s less effective for most people. Methotrexate boosts the response to biologics, reducing the chance your body will neutralize them. However, if you can’t tolerate methotrexate due to nausea, liver issues, or side effects, your doctor may prescribe a biologic alone. Some patients do well on monotherapy, especially with newer biologics or JAK inhibitors.
Are biosimilars as good as the original biologics?
Yes. Biosimilars are not generics-they’re highly similar versions of the original biologic, with no clinically meaningful differences in safety or effectiveness. The FDA requires them to pass rigorous testing. Adalimumab biosimilars like Amjevita and Cyltezo have been used safely in millions of doses since 2016. They cut costs by 15-30% and are now standard in many insurance plans.
Why do some doctors avoid JAK inhibitors?
Because of safety warnings. The 2022 ORAL Surveillance trial showed higher rates of heart attacks, strokes, blood clots, and cancer in patients over 50 using JAK inhibitors, especially those with existing risk factors. The FDA now requires a black box warning. Doctors avoid them for older patients or those with heart disease, smoking history, or prior cancer. For younger, healthy patients with aggressive RA, they’re still a strong option.
How long does it take for biologics to work?
Most patients start feeling better in 4-8 weeks, but full effect can take 3-6 months. That’s why doctors don’t switch drugs too quickly. If you don’t see improvement after 12 weeks, your doctor may adjust your dose or switch to another biologic. Patience is key-but not endless. If nothing works after 6 months, it’s time to rethink the plan.
Can I stop taking these drugs if I feel better?
Not without talking to your doctor. Stopping DMARDs or biologics too soon can cause a flare-up, sometimes worse than before. Some patients in remission for over a year may try to taper under close supervision, but most need to stay on some form of medication long-term to prevent joint damage. RA doesn’t go away-it just goes quiet. Keep treating it.
 Online Pharmacy roidsource.net Review: Safe Steroid Buying Guide
Online Pharmacy roidsource.net Review: Safe Steroid Buying Guide
 Levaquin Antibiotic: Key Facts, Side Effects, and Safer Alternatives
Levaquin Antibiotic: Key Facts, Side Effects, and Safer Alternatives
 Insulin Therapy Side Effects: Managing Hypoglycemia and Weight Gain
Insulin Therapy Side Effects: Managing Hypoglycemia and Weight Gain
 Exploring the Top 8 Alternatives to Canadapharmacy.com in 2025: Navigating the Online Pharmacy Landscape
Exploring the Top 8 Alternatives to Canadapharmacy.com in 2025: Navigating the Online Pharmacy Landscape
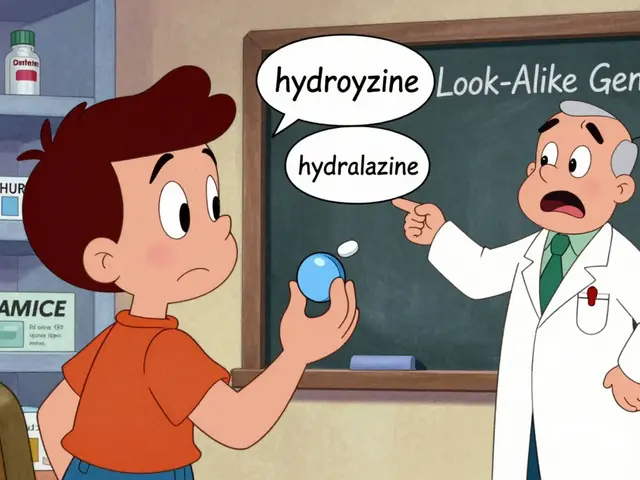 Pharmacy Errors with Generics: How to Prevent and Fix Common Mistakes
Pharmacy Errors with Generics: How to Prevent and Fix Common Mistakes
Jeremy Hernandez
November 17, 2025 AT 20:47Bro this whole post is just Big Pharma whispering in your ear. Methotrexate? It’s a chemo drug repackaged as a miracle cure. Biologics? They’re basically designer antibodies that cost more than your car. And don’t get me started on JAK inhibitors - they’re basically ticking time bombs wrapped in a pill. You think you’re saving your joints? You’re just trading one set of problems for a whole new one. I’ve seen people on these meds end up in the ER with pneumonia because their immune system was nuked. They call it treatment. I call it chemical surrender.
Tarryne Rolle
November 19, 2025 AT 08:54It’s ironic, isn’t it? We’ve built a medical system that can engineer proteins to target specific cytokines, yet we still can’t afford to let people live without financial ruin. The real disease here isn’t RA - it’s capitalism disguised as healthcare. We treat symptoms with billion-dollar biologics while ignoring the root: stress, poverty, environmental toxins, and the systemic abandonment of preventive care. A pill can’t fix a society that treats human bodies like disposable machinery.
Kyle Swatt
November 21, 2025 AT 06:06Look i’ve been on methotrexate for 7 years and let me tell you something - it ain’t pretty but it’s the only thing keeping me from crawling on the floor like a wounded animal. Biologics? They’re magic if you got the cash. But here’s the raw truth nobody says: it’s not about the drug. It’s about the person behind the prescription. I’ve had doctors treat me like a spreadsheet. I’ve had insurance reps tell me to ‘just take less’ because my co-pay was too high. The science? Solid. The system? Broken. And yeah i know biosimilars exist but good luck getting your doc to switch you over without a 6-month paperwork gauntlet. This ain’t medicine. It’s a damn obstacle course with side effects.
Deb McLachlin
November 22, 2025 AT 21:43While the article presents a comprehensive overview of current therapeutic modalities for rheumatoid arthritis, it would benefit from a more explicit discussion regarding longitudinal outcomes of triple DMARD therapy versus biologic monotherapy in low-resource settings. The referenced Indian cohort data, while compelling, lacks detail on radiographic progression over time. Additionally, the omission of cost-effectiveness analyses beyond U.S. insurance structures limits generalizability. The inclusion of global health equity considerations would significantly enhance the utility of this resource for international clinicians and patients.
saurabh lamba
November 23, 2025 AT 16:38bro why u even tryin? i got RA too and i just drink turmeric milk and pray. biologics cost more than my whole month’s salary here. methotrexate gave me nausea so bad i threw up for a week. triple DMARD? yeah my doc gave me that but i skip half the pills. i still walk. i still cook. maybe the body knows better than the lab?
😅Kiran Mandavkar
November 24, 2025 AT 23:31Pathetic. You people are still debating whether methotrexate is ‘enough’? That’s a 1950s cancer drug you’re clinging to like a security blanket. Biologics are the future, and anyone who refuses them because of ‘side effects’ is just afraid of progress. And don’t even get me started on JAK inhibitors - if you’re over 50 and still on those, you’re not managing RA, you’re gambling with your life. This isn’t a hobby, it’s a war - and you’re showing up with a slingshot while the enemy has tanks. Wake up.
Eric Healy
November 25, 2025 AT 18:57yo i read this whole thing and like… why do they say ‘methotrexate is the anchor’ like its some holy grail? i tried it and my liver went haywire. my doc just shrugged and said ‘try again’ like im a lab rat. and biosimilars? sure they’re cheaper but they’re still 1500 a month. i work two jobs and still can’t afford the co-pay. and dont even get me started on the black box warning on jaks - like yeah thanks for telling me after i already started taking it. this system is rigged.
Shannon Hale
November 27, 2025 AT 09:02STOP. RIGHT. NOW. I’m 32, been on Humira since I was 24, and I just walked 5 miles yesterday for the first time in 8 years. You think this is just ‘meds’? This is my freedom. This is me being able to hold my niece without crying from pain. I’ve cried in pharmacy parking lots over the cost. I’ve begged insurance for 11 months just to get approved. But I didn’t give up. I didn’t ‘pray’ or ‘drink turmeric’. I fought. And if you’re sitting there saying ‘maybe the body knows better’ - go ahead. But don’t act like your pain is wisdom when mine is survival. This isn’t a debate. It’s a lifeline. And I’m not letting anyone tell me I’m wrong for grabbing it.