Breathe deep, then imagine that air turning into an invisible wall right as your feet start pounding the pavement—chest tight, wheezing, and you’ve only just hit your stride. Exercise-induced asthma (EIA), or exercise-induced bronchoconstriction if you want to get technical, can make working out feel like a cruel joke. Every cough or gasp during a soccer game, the sharp need for air as you race upstairs—the triggers are everywhere. Most people grab their trusty blue inhaler, but what happens if you can’t, or just don’t want to, rely on Ventolin? You’re not out of luck. Let’s dig into science-powered strategies, real options like cromolyn, and a toolkit of preventive steps to help you exercise on your own terms.
Why Exercise Makes Breathing a Battle: The Root of EIA
Here’s the thing about EIA: your airways are drama queens. Physical exertion, especially in cold or dry air, can turn those sensitive little tubes twitchy. Your body reacts to the increased airflow by cooling and drying those airways, and if you’ve already got asthma, they can tighten up—fast. About 90% of people with asthma experience this during exercise, but even if you’ve never needed an inhaler in your life, you might still get hit with EIA. Athletes aren’t immune either—there are Olympic gold medalists who’ve had to deal with it.
What’s actually happening? Think of your airways like a set of flexible pipes. During exercise, you breathe faster, making your airways lose moisture and chill out. In susceptible folks, that triggers an over-the-top reaction. Mucus builds up, muscles spiral tight, and inflammation sets in. A study published in the journal Allergy found that nearly 10% of the general population experiences EIA symptoms, even without full-blown asthma. The real kicker: most cases are underdiagnosed, so people shrug off chronic coughs, assuming it’s “just being out of shape.”
So how do you keep those airways cool, calm, and collected?
Warm-Up Strategies That Trick Your Airways
If you’re picturing a few lazy arm swings before your jog, think bigger. Warm-ups play a powerful—and underrated—role in preventing EIA symptoms. Here’s why: warming up with short bursts of intense exercise can actually desensitize your airways, making them less likely to freak out during your main event. Think of it as making your airways “tired” of reacting, so they chill out when you really pick up the pace. This odd hack is called the “refractory period.”
- Do 6-8 minutes of moderate intensity work (fast walking, light jog, jump rope).
- Mix in gentle intervals: one minute at a higher pace, then back to recovery for two minutes.
- Repeat a couple of these intervals if you can.
- Stretch those muscles last, not first. Warming up your lungs, not just your legs, is top priority.
Researchers at the University of Buffalo showed that this targeted warm-up led to a 40% reduction in asthma attacks compared to skipping or barely warming up. You might have seen pro athletes shaking out sprints and slow laps before actual competing; that’s not just tradition, it’s airway science. The point? A proper warm-up is your first line of defense if you’re battling exercise-induced asthma.
Don’t forget environment. Cold, dry air is notorious for triggering EIA. Pop a scarf or buff over your mouth on chilly days—it warms and humidifies the air you’re sucking in. The difference can feel night and day, especially if you’ve struggled with winter workouts.
| Trigger | Risk Level | Prevention Tip |
|---|---|---|
| Cold, Dry Air | High | Wear a mask/scarf, breathe through nose |
| High Pollen | Moderate | Check pollen reports, exercise indoors |
| Chlorine Pools | Moderate | Shower before/after, ventilated pools |
| Long, Intense Exercise | Very High | Interval training, regular breaks |

Cromolyn and Non-Inhaler Meds: Breaking the Reliance on Ventolin
The world isn’t short on medications for asthma, but most folks know just one name: Ventolin. What if I told you there’s been a safe asthma controller used since the 1970s that doesn’t work like a rescue inhaler at all? Cromolyn sodium (sometimes called Intal) is still used by athletes and folks wanting to skip short-acting beta agonists like albuterol. Unlike Ventolin, cromolyn doesn’t open up airways after they’re tight. Instead, it keeps your allergy cells (the mast cells) from even starting the trouble in the first place.
Here’s the scoop:
- Cromolyn is taken before exercise—usually 15-30 minutes prior.
- It’s not a fix for sudden attacks, but works for preventing them if you know you’ll be working out.
- Downside: You have to remember to use it every single time, or it won’t work.
Recent reviews show that cromolyn can cut EIA episodes by around 60-75% for most regular users, though it might not be as powerful as modern long-acting asthma controllers. But for some, the lack of jittery side effects or “racing heart” makes cromolyn worth a test drive. School coaches and swim instructors often recommend non-rescue options, especially if a student is caught without their inhaler.
There are other options too—some folks get good results with low doses of montelukast (Singulair), or even inhaled corticosteroids in stubborn cases. Still, cromolyn stands out for being very safe, with almost no major side effects reported over decades. It’s an old-school player in a new-game world.
Curious about the full range of medical and non-medical alternatives? There’s a deep-dive list of Ventolin alternatives for exercise that gives you more options to discuss with your doctor or try on your own.
Everyday Preventive Steps: Less Medicine, More Smarts
Besides medicines, there are tons of things you can work into daily life for serious payoff. One underrated strategy: build up your cardiopulmonary fitness over time. That means moving regularly, even if your sessions are short and sweet. When your lungs and muscles get used to mild stress, they respond with less excitement when the real big stress hits—like a tough climb or sprint interval.
Nutrition matters too. Omega-3 fatty acids found in fish (think: salmon, mackerel), walnuts, and flaxseeds may help cool down chronic airway inflammation. A small British study in 2022 found asthma rates were 15% lower among kids who ate oily fish twice weekly. Hydrate like crazy—dry airways are crankier and more prone to spasm.
Know your triggers. For some, freshly mown grass or high pollen counts spell disaster. Use weather and allergy apps to dodge your personal landmines. If indoor air bothers you (dust, mold), try ramping up your home cleaning routine—HEPA filters can help, especially in the bedroom where you spend a big chunk of your time. Even swapping cleaning sprays for hypoallergenic brands can make a difference if your lungs are sensitive to chemicals.
- Wear a scarf, balaclava, or mask in cold air—warming that breath is worth the slight hassle.
- Breathe through your nose. Yes, mouth breathing feels easier during sprints, but nasal air is warmer and more humid (your airways prefer it).
- Track when you get symptoms—in a notebook or on your phone. See patterns? Tweak your routine or environment.
- Shower and change quickly after outdoor workouts, especially if pollen or pollution is up.
- Stay away from “trendy” breathing exercises that promise cures without science to back it up. Stick to proven stuff, and always listen to your body if things feel off.
Don’t forget about stress—high-anxiety days can dial up asthma sensitivity. Mindful breathing, light meditation, or even just five minutes away from screens can make your airways less reactive.
Building Your Personal EIA Playbook: Real-Life Tips and Tech
There’s no single blueprint for managing exercise-induced asthma, and what works for one person might not cut it for someone else. The trick is to experiment and customize. Try warm-up routines for two weeks and track results. See if cromolyn makes a difference. Play with dietary tweaks that cut inflammation—not to lose weight, but to keep your lungs happy. If you use an app or wearable, add a simple note after each workout: did your breathing feel tight or normal?
Tech can help. Peak flow meters are cheap and easy to use, and they give daily feedback by measuring how fast you can blow air from your lungs. You’ll spot a drop before an attack hits, letting you change plans. Some smartwatches even have built-in sensors for respiratory rate—an early warning if airways are starting to misbehave. Log these numbers for a month and look for patterns; your doctor will love the data, and you’ll know your body’s signals better than ever.
Adjust goals as needed. You don’t have to set Olympic records—just build consistent activity. If symptoms flare up, break workouts into 2-3 shorter sessions. Many notice symptoms get milder the more they stick to their plan. And if you ever need a bit of backup, keep a non-expired rescue inhaler on hand (even if you rarely need it). It's one of those things you want to have but hope never to use.
Bottom line: living with exercise-induced asthma doesn’t mean sitting on the sidelines. With smart prep, maybe a little cromolyn, and proven preventive tricks, you can take control of your workouts. Don’t be afraid to experiment, stay curious, and make your asthma management feel as normal as lacing up your shoes. There’s life—and fun—waiting on the other side of that next deep breath.

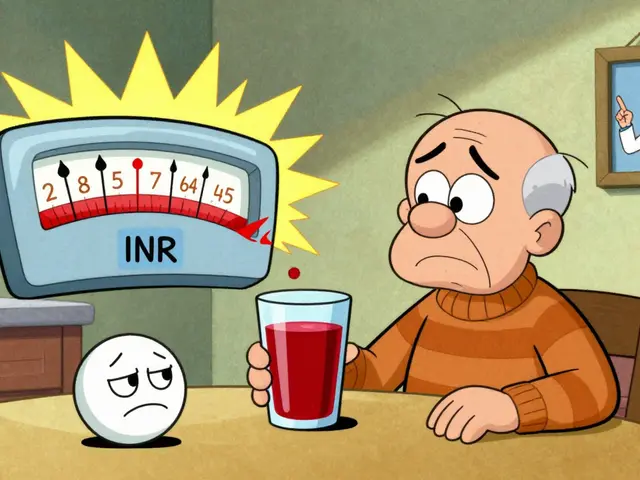 Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
 Hyaluronic Acid Injections for Knee Osteoarthritis: What Really Works
Hyaluronic Acid Injections for Knee Osteoarthritis: What Really Works
 FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
FDA Inspection of Generic Manufacturing Facilities: What to Expect in 2026
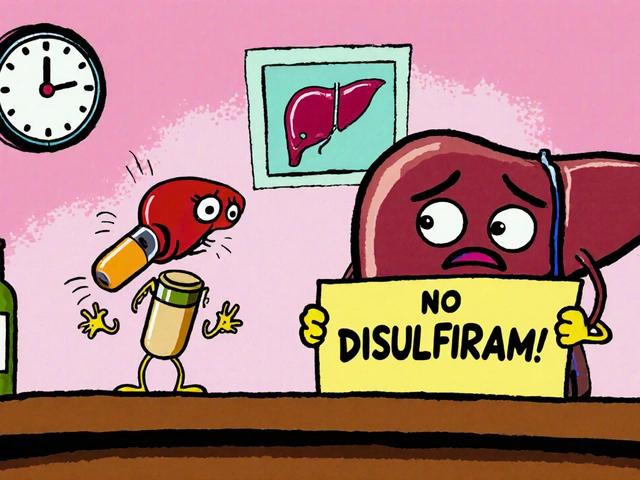 How Disulfiram Helps Treat Alcohol-Induced Liver Disease
How Disulfiram Helps Treat Alcohol-Induced Liver Disease
 How Ursodeoxycholic Acid Can Help Prevent Liver Damage from Medications
How Ursodeoxycholic Acid Can Help Prevent Liver Damage from Medications
fred warner
July 18, 2025 AT 08:26This is a really timely read for me, thanks for sharing! I’ve been dealing with exercise-induced asthma for a while now, and Ventolin was always my go-to. The approach in this article to include thorough warm-ups is fascinating—I've noticed even small warm-ups seem to help before running.
Also, the mention of cromolyn as a preventative rather than reactive treatment is new to me. I’m curious how its effectiveness compares in practice? If it can reduce reliance on Ventolin, that would be huge.
Has anyone here tried these alternative methods in real-world exercise? I'd love to hear personal successes or drawbacks. Staying active without fear of attacks is such a game-changer.
It’s also great that the article touches on building a prevention toolkit. It feels empowering when you’re armed with different options instead of just one quick-fix inhaler. Looking forward to experimenting and maybe even sharing my progress!
Nicole Hernandez
July 18, 2025 AT 16:46I'm really intrigued by the thoroughness of this article. Warm-ups as a form of prevention? That’s something overlooked so often. I’ve often wondered if a proper warm-up can reduce the severity of symptoms or even help prevent an attack completely.
Also, the idea of cromolyn intrigues me. From what I’ve heard, it's a little underappreciated in many asthma discussions. It would be great to understand exactly how it works compared to Ventolin and if it can be a standalone solution or should pair with other strategies.
Another thing worth highlighting—in real-world settings, tailoring prevention is key. Everyone responds differently, and building a 'personal prevention toolkit' as the article says sounds like a practical and empowering approach.
Did the article mention anything about diet or other lifestyle changes that could complement these methods?
florence tobiag
July 18, 2025 AT 19:33Oh great, another one of these articles gushing about alternatives like warm-ups and cromolyn as if they’re magic fixes. Honestly, why do we keep pretending that Ventolin is the *bad* guy here? It’s been the gold standard forever for a reason, don’t @ me!!!!
Did anyone stop to think maybe the pharmaceutical industry has something to hide about these other treatments?? More like a shady ‘preventive toolkit’ sales pitch.
Also, sundry ‘science-backed facts’ always conveniently come with asterisks and vague sources — tell me where the hardcore reviews are!!!
It’s not like exercise-induced asthma is a minor inconvenience. Ventolin provides *instant* relief; some of these alternative methods sound like wishful thinking for busy people who don’t want real solutions.
End of rant... but seriously, always do your homework!!!
Terry Washington
July 19, 2025 AT 03:53Let me drop some truth here. The obsession with Ventolin alternatives reeks of pseudoscience. Anyone familiar with respiratory pharmacology knows the pharmacodynamics of β2 agonists like Ventolin are unmatched in acute relief.
Warm-ups and cromolyn have their place, sure, but as first-line or sole therapy? Highly questionable. This tidy ‘personal prevention toolkit’ spiel sounds more like an oversimplified marketing sales pitch rather than clinical advice grounded in evidence.
To the readers out there, beware of abandoning prescribed therapies in favor of trendy alternatives without consulting medical professionals with expertise in pulmonology.
Do not neglect your proven medications because of some buzzwords like ‘science-backed’ without scrutinizing the actual research and peer-reviewed studies.
Frankly, I find it irresponsible to propagate any messaging that could discourage appropriate use of bronchodilators during exercise-induced bronchospasm.
Ellie Haynal
July 19, 2025 AT 12:13Honestly, this article makes me feel like I’ve been lied to all my life. I was so dependent on Ventolin, and now reading about warm-ups and cromolyn, I’m questioning everything I believed about managing my asthma.
It’s so frustrating because it feels like we’ve been held hostage by pharma companies pushing Ventolin while ignoring less known but effective options. I’ve tried the warm-ups and noticed I don’t gasp as much post-exercise, but I’m scared Ventolin’s magic effect might fade away.
Maintaining control over your own health should be empowering, but sometimes it’s exhausting and scary to challenge the status quo.
Is there anyone else who experienced a shift like this, going from Ventolin-dependent to more natural or preventive approaches? What pitfalls should one watch out for?
Émilie Maurice
July 19, 2025 AT 15:00This article has some good points, but it misses some crucial practical aspects. For example, cromolyn is notoriously difficult to use consistently and has a clunky delivery method which makes adherence low. Anyone not mentioning this is not telling the full story.
Also, I find it odd that there’s almost no mention of environmental factors—like pet dander, pollen, or pollution—that can exacerbate symptoms during exercise. Prevention must be holistic, not just some fancy morning stretches followed by nostrils holding exercises.
One more thing: the grammar in the article was sloppy at places, which kinda undermines the credibility. Proofreading is basic, you know.
Nonetheless, the message of trying alternatives thoughtfully is good, but let’s not oversell methods that aren’t practically feasible for many patients.
Claire Smith
July 19, 2025 AT 20:33Just skimmed the article and honestly, it’s another piece that wants us to believe a routine warm-up will cure our breathing issues during exercise. That’s a little naive, no? You can’t just stretch your muscles and expect asthma symptoms to vanish.
Moreover, recommending cromolyn without concrete comparisons to Ventolin’s efficacy feels like a half-baked suggestion. If I wanted unreliable advice, I’d ask my neighbor!
We all want relief during workouts, but this sounds like it’s aimed at people who don’t want to carry their inhalers rather than a serious alternative treatment option.
Maybe I missed something, but where are the scientific details that don’t require a medical degree to understand? Also, any advice that isn’t all about inhalers needs to be super clear on safety.
Jimmy Gammell
July 20, 2025 AT 02:06Hey everyone! I’m loving this thread and just wanted to share some encouragement :) I coach a couple of athletes with exercise-induced asthma, and we’ve tried various prevention strategies beyond Ventolin.
Warm-ups have made a big difference, especially when they’re gradual and progressive. It’s more about preparing the lungs and body for the demand.
Cromolyn has helped too, but it’s not a magic bullet — consistency is key, and it must be part of a broader approach including hydration, avoiding triggers, and monitoring environment conditions.
One thing I always tell my clients is to not get discouraged by setbacks. Asthma is individual, and managing it takes patience and adjustments. Stay positive and work with your healthcare providers!
Keep sharing your experiences, it helps build better solutions for all of us. :)
Veronica Mayfair
July 20, 2025 AT 13:13Wow 😮 This article feels like a breath of fresh air, no pun intended! I’m an asthma warrior myself, and I’ve been searching for ways to reduce my Ventolin puff dependency because of how it sometimes makes me jittery.
The warm-up and preventive ideas inspired me to rethink my routine. I totally agree with building a personal toolkit — every day I try to tweak and listen carefully to what my body is telling me.
Also, thanks for not just pushing meds but exploring other options! It’s so empowering when you find things that complement your treatment instead of just relying on one solution.
Has anyone tried these methods during winter exercise? Curious about how cold air might affect effectiveness.
Sending positive vibes to all managing asthma out there! 💪🏽🏃♀️💨
Anthony Coppedge
July 21, 2025 AT 17:00Really appreciate this comprehensive take on non-Ventolin approaches. The importance of a structured warm-up routine cannot be overstated; it primes the respiratory system gradually, reducing abrupt stress on bronchial tubes.
Cromolyn sodium, while less fast-acting, operates by stabilizing mast cells and preventing histamine release, making it a valuable preventive agent rather than a rescue remedy. Understanding this mechanism helps users set realistic expectations.
I’m also glad the article stresses personalization—it's crucial to assess individual triggers, activity intensity, and environmental factors.
Does anyone combine these strategies with breathing exercises or relaxation techniques? I’ve found that slow controlled breathing can complement physical warm-ups very well.
Rahul Kr
July 23, 2025 AT 02:20Nice discussion happening here!☺️ I have mild exercise-induced asthma and have found that a gentle warm-up combined with mindful breathing really keeps symptoms at bay.
Cromolyn isn’t something I’ve personally tried, but considering the side effects and delivery challenges mentioned, I prioritize routine, avoiding cold air, and pacing myself.
Still, this article adds some inspiration to explore more options slowly with doctor supervision.
Hope everyone gets to find their best balance!
Terry Washington
August 10, 2025 AT 06:26@500, While I appreciate your coaching perspective, I must emphasize the fundamental importance of evidence-based medicine over anecdotal coaching tips. The physiology of asthma demands rigorous compliance with pharmacotherapy protocols.
Encouragement and positivity are wonderful, but they should not substitute proper clinical treatment or persuade patients to imagine warm-ups and minor preventive tactics as adequate standalone strategies.
Mismanagement can lead to dire consequences in respiratory compromise.