Bringing someone with you to a medication appointment isn’t just a good idea-it’s a game-changer. Too many people leave these appointments confused, overwhelmed, or worse, with the wrong pills in their hands. You might think you remember everything the doctor says, but stress, fatigue, or side effects from your meds can make even simple instructions slip away. That’s where a caregiver or advocate comes in. They don’t need to be a doctor. They just need to be someone you trust who can listen, ask questions, and remember what you forget.
Why You Need Someone There
Medication errors are more common than most people realize. In the U.S. alone, they affect 1.5 million people every year. Many of these errors happen during appointments-when a new prescription is written, a dose is changed, or a drug interaction isn’t caught. The Joint Commission found that 78% of these mistakes occur during transitions of care, like when you switch doctors or start a new medication. That’s why having a second set of eyes and ears in the room matters so much. A 2023 study in Health Affairs showed that patients with trained advocates had 28% fewer medication errors. Even more telling: when someone helped review prescriptions, medication reconciliation errors dropped by 63% in a 12-month hospital study. This isn’t about being overly cautious. It’s about protecting yourself from a system that’s designed for speed, not clarity.Who Can Be Your Advocate
Your advocate doesn’t have to be a professional. In fact, most people use family members, partners, or close friends. But you can also hire a certified healthcare advocate if you need more support. These professionals are trained in medication safety, insurance navigation, and patient rights. As of January 2024, over 1,800 were certified in the U.S. through the Patient Advocate Certification Board. Family caregivers are the most common choice. But here’s the catch: untrained family advocates miss about 42% of critical medication details, according to a University of Pennsylvania study. That’s why preparation matters more than who shows up. Professional advocates cost between $75 and $200 an hour, but many Medicare Advantage plans now include free advocacy services. UnitedHealthcare, for example, offers it to 89% of their Medicare members. Check your plan-this might already be covered.How to Prepare Before the Appointment
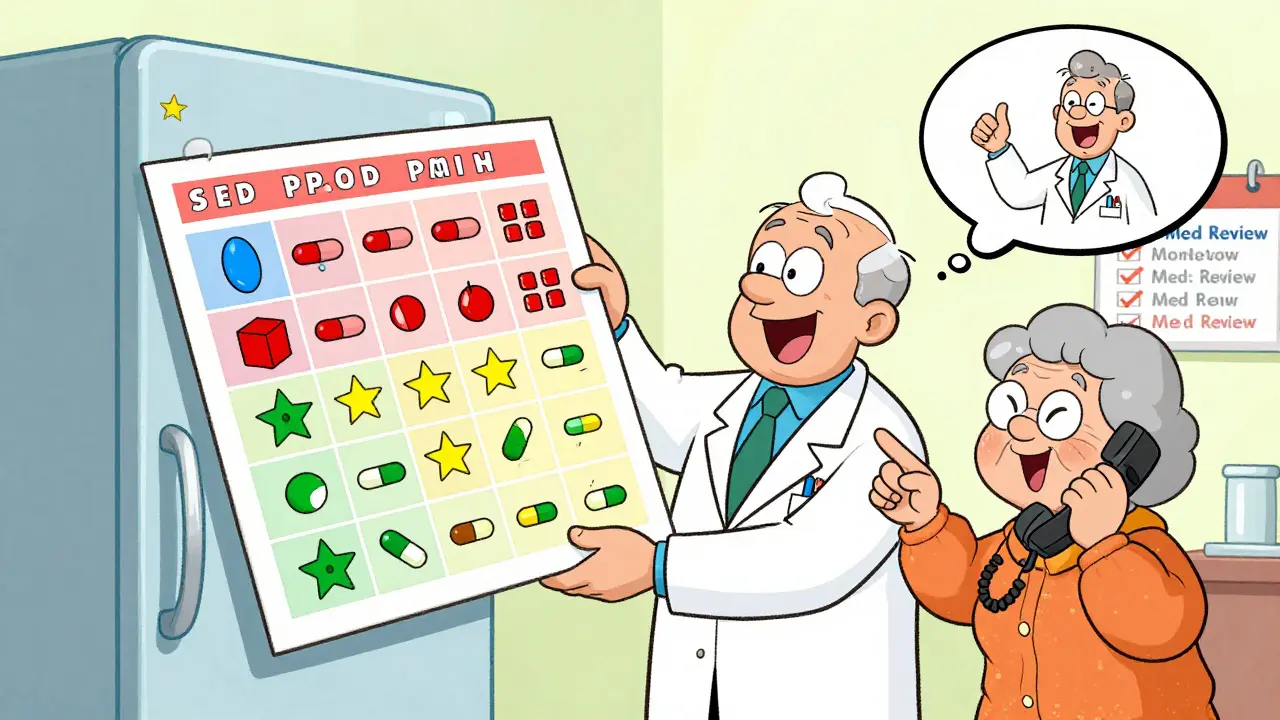
Preparation is the most powerful tool you have. Start three days before your appointment.- Gather every pill bottle. Don’t rely on a list. The FDA says 23% of medication errors come from inaccurate lists. Bring the actual bottles-even the empty ones. That way, your advocate can match the label to what the doctor says.
- Write down symptoms and side effects. Note when they happen: after taking a pill? Before dinner? At night? Use a simple notebook or a free app like Medisafe. The National Down Syndrome Society found that using a printed symptom tracker improved medication adherence by 34%.
- Check your insurance coverage. Eighteen percent of prescriptions get delayed because of coverage surprises. Call your insurer 48 hours before your visit. Ask: Is this drug covered? Do I need prior authorization? Is there a cheaper generic?
- Write your questions. Use the Ask Me 3 framework: What is my main problem? What do I need to do? Why is it important? Write them down. Don’t rely on memory.
What to Do During the Appointment
Once you’re in the room, your advocate’s job is to speak up-calmly, clearly, and confidently.- Confirm the medication list. Ask the doctor: “Can we go through each medication one by one? I want to make sure we’re not missing anything or adding something that doesn’t belong.”
- Check doses and instructions. Ask: “Is this pill safe to crush or split?” “Do I take it with food or on an empty stomach?” “What time of day is best?” A Johns Hopkins study found that 12.3% of prescriptions have incorrect dosage instructions.
- Use the SBAR method. It’s a simple communication tool used by nurses and doctors: Situation (I’m here because my mom’s been dizzy after taking her new blood pressure pill), Background (She’s on five meds, including warfarin), Assessment (I think the dizziness might be from the interaction), Recommendation (Can we check for interactions or adjust the dose?). This increases understanding by 52%.
- Ask about alternatives. “Is there a less expensive option?” “Are there non-drug ways to manage this?” Many patients don’t ask because they feel rushed. Your advocate can slow things down.
What to Do After the Appointment
The appointment doesn’t end when you walk out. In fact, the most critical work happens after.- Review everything right away. Sit down with your advocate within 24 hours. Go over the notes. Did the doctor change anything? Did they say something that didn’t make sense? Write it down.
- Create a visual medication schedule. Take photos of each pill. Put them in a calendar with times and notes. GoodRx’s study showed this reduces identification errors by 67%. A photo of a blue oval pill is easier to recognize than “metoprolol 25 mg.”
- Call the pharmacy. Don’t wait until you get there. Call ahead and confirm the prescription was filled correctly. Ask the pharmacist: “Is this the same as what the doctor ordered?” Pharmacists are trained to catch errors-and they catch 45% of them before they reach you.
- Set up a ‘medication buddy’ system. If you live alone, ask someone to check in weekly. A simple text: “Did you take your pills today?” increases adherence by 41%.

What to Do If the Provider Says No
Sometimes, staff will say, “We can’t talk to you-that’s HIPAA.” That’s wrong. HIPAA allows patients to designate anyone they want to be involved in their care. All you need is a signed form, which most clinics provide. If you’re turned away:- Ask to speak with the office manager or patient services representative.
- Say: “I’ve been told I have the right under the Affordable Care Act to bring an advocate. Can you help me fill out the form?”
- If they still refuse, file a complaint with the clinic’s patient relations department. By 2023, 92% of large healthcare systems had formal policies requiring them to accommodate advocates.
Real Stories That Changed Things
One woman, ‘MedSafetyMom’ on Reddit, brought her daughter to a routine appointment. The doctor prescribed a new antibiotic. Her daughter noticed it was the same one that had caused a dangerous reaction with warfarin. They stopped it before the first dose. “I was too scared to ask,” she said. “She knew to look.” Another man, a retired pharmacist, created a color-coded chart with pictures of each pill for his mother. He called the pharmacy every time a new script came in. He reduced her medication errors by 76%. And then there’s the opposite: a patient in a Reddit thread had their advocate locked out of the room. No paperwork was accepted. They left with a new prescription that caused a 10-day gap in their treatment-and ended up in the ER.What’s Changing in 2026
The rules are shifting fast. The Centers for Medicare & Medicaid Services now require doctors to document advocate involvement in high-risk cases. If they don’t, they lose money. That means more clinics are training staff to welcome advocates. AI tools like MediCheck Pro are being used in clinics to flag dangerous drug interactions during appointments. And telehealth advocacy is growing-by 2026, two out of three medication consultations will include a virtual advocate joining by video. The bottom line? You’re not being difficult by bringing someone. You’re being smart. Medication safety isn’t about memorizing labels. It’s about having a team. And your advocate? They’re not a helper. They’re your partner in staying healthy.Can I bring someone to my medication appointment even if they’re not family?
Yes. You can bring anyone you trust-friends, neighbors, paid advocates, or community health workers. All you need is to give written permission to your provider. HIPAA doesn’t block this-it actually protects your right to choose who’s involved in your care.
What if I don’t have anyone to bring?
Many Medicare Advantage plans now offer free medication advocacy services. Check your plan’s benefits or call member services. Nonprofits like the Patient Advocate Foundation also offer free or low-cost support. Some pharmacies, like CVS and Walgreens, have patient navigators who can help you review your meds before your appointment.
Do I need to sign a form to bring an advocate?
Most clinics will ask for a simple authorization form, often called a “Designated Representative” form. It’s quick-usually just your name, the advocate’s name, and your signature. Some let you do it over the phone. If they don’t have one, ask to speak with patient services. You have a legal right under the Affordable Care Act to have someone with you.
Can my advocate talk to the pharmacist too?
Yes. Pharmacists are key players in medication safety. Your advocate can call the pharmacy to confirm the prescription, ask about side effects, or check for interactions. Many pharmacists welcome this. In fact, 45% of medication errors happen at the pharmacy-and advocates help catch them before you even leave.
What if I’m worried my advocate will make things awkward?
It’s normal to feel that way. But most providers appreciate advocates who are prepared and respectful. The key is to be collaborative, not confrontational. Say things like, “I just want to make sure I understood correctly,” or “Could you explain that again?” That’s not pushing back-it’s protecting your health.

 Blue Light and Eye Health: Screen Filters and Habits That Actually Work
Blue Light and Eye Health: Screen Filters and Habits That Actually Work
 Harness the Power of Nature: The Ins and Outs of Marijuana Dietary Supplements
Harness the Power of Nature: The Ins and Outs of Marijuana Dietary Supplements
 Hemophilia and Alcohol: Essential Facts and Safe Practices
Hemophilia and Alcohol: Essential Facts and Safe Practices
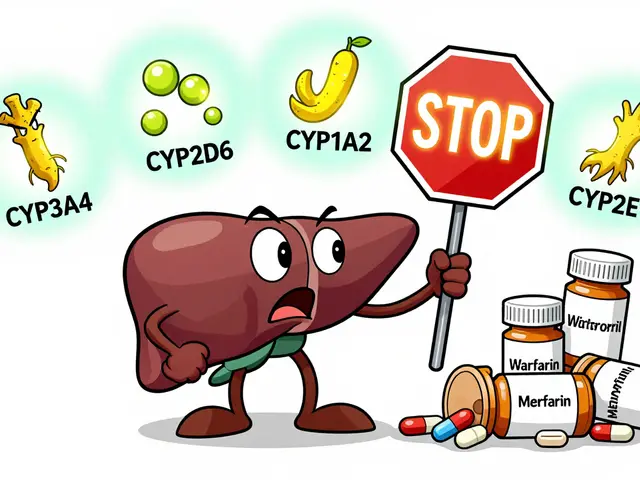 Goldenseal and Medications: What You Need to Know About Liver Enzyme Interactions
Goldenseal and Medications: What You Need to Know About Liver Enzyme Interactions
 Unlock Your Body's Natural Energy with Ribose: The Revolutionary Dietary Supplement
Unlock Your Body's Natural Energy with Ribose: The Revolutionary Dietary Supplement
Heather Wilson
January 9, 2026 AT 07:26This article is dangerously oversimplified. You act like bringing someone along is some magical shield against medical errors, but what about liability? If your 'advocate' mishears a dosage and you overdose, who's legally responsible? The doctor? The advocate? You? HIPAA doesn't protect you from your own incompetence.
And don't get me started on the 'free advocacy services' myth. Medicare Advantage plans don't offer this out of the goodness of their hearts-they do it to avoid paying for ER visits later. This isn't patient empowerment, it's cost-shifting.
Also, 45% of errors happen at the pharmacy? Then why not just hire a pharmacist as your advocate instead of dragging your cousin who doesn't know the difference between metoprolol and metformin?
Stop romanticizing chaos. This system is broken because people refuse to take personal responsibility.
Micheal Murdoch
January 9, 2026 AT 13:44I’ve been a caregiver for my mom for six years now, and this piece got me right in the chest. Not because it’s perfect-it’s not-but because it finally names what so many of us do in silence.
You don’t need to be a doctor. You don’t need to memorize every drug interaction. You just need to show up. Even if you’re nervous. Even if you’re shaking. Even if you’re 70 and your own memory’s failing.
I used to feel like a nuisance. Then one day, the nurse said, 'You’re the reason she’s still here.' That’s all you need to hear.
Bring the pill bottles. Write the questions. Ask for the form. Say 'I’m not sure I understood.' That’s not weakness. That’s wisdom.
And if someone tells you you’re not allowed? Smile. Say 'Okay, I’ll call your patient advocate office.' Then do it. They’ll back down.
You’re not asking for special treatment. You’re asking for basic human dignity. And that’s never too much to ask.
Jeffrey Hu
January 11, 2026 AT 12:54Let’s be real-most people who bring 'advocates' are just trying to offload their own anxiety onto someone else. And the article ignores the fact that 80% of these advocates are untrained relatives who misinterpret everything.
That '63% drop in errors' study? It was a 12-month hospital trial with trained professionals, not your cousin who watches medical dramas on Netflix.
Also, why is everyone acting like pharmacists are some kind of miracle workers? They’re overworked, underpaid, and often just reading a screen. If you think calling ahead stops errors, you’ve never waited 45 minutes for a simple script to be filled.
And the 'color-coded chart' thing? Cute. But if your parent can’t read, what then? Or if they’re blind? This article assumes everyone has access to tech, time, and family support. Reality check: most people don’t.
Stop pretending this is a fix. It’s a Band-Aid on a hemorrhage.
Matthew Maxwell
January 12, 2026 AT 06:40It’s pathetic how we’ve turned healthcare into a spectator sport. You can’t trust yourself to remember a pill schedule, so you bring a cheerleader? That’s not advocacy-that’s enablement.
And the 'Ask Me 3' framework? That’s for people who can’t read. Why not just teach patients to read medical labels? Why not teach them to ask questions themselves?
Every time we outsource responsibility, we make the system worse. The doctor doesn’t have time to explain because now they’re explaining to two people, one of whom is emotionally overwhelmed.
And don’t even get me started on the 'virtual advocate' trend. Next thing you know, we’ll have AI bots whispering in patients’ ears during surgery.
This isn’t progress. It’s surrender.
Pooja Kumari
January 13, 2026 AT 03:29Oh my god, I cried reading this. I’ve been doing this for my dad since he had his stroke, and no one ever says it out loud: it’s lonely. You’re the one who remembers the names of the pills, who calls the pharmacy at 8 p.m., who stares at the pill organizer and wonders if you messed up the colors.
And then you get blamed for being 'too involved' when you ask why the doctor changed his blood thinner.
My husband says I’m obsessive. But what’s more obsessive? Caring too much or letting someone you love die because no one was paying attention?
I don’t care if it’s 'too much.' I care that he’s alive. And if that makes me a 'toxic' advocate, then fine. I’ll wear that badge with pride.
Thank you for writing this. I didn’t know I was doing something right until now.
Jacob Paterson
January 15, 2026 AT 03:19Oh wow. Another feel-good piece for people who think healthcare is a group project. Let me guess-you also believe in 'vibes' as medical diagnostics?
You want to bring your 'advocate'? Great. Now the doctor has to explain things twice, once to the patient who’s too tired to understand, and once to the emotionally volatile cousin who thinks 'statins' are a type of dance.
And let’s not forget the 'MedSafetyMom' story. Yeah, her daughter caught a bad interaction. But what if she’d been wrong? What if she’d caused a delay that led to sepsis? No one talks about that.
This isn’t empowerment. It’s a lawsuit waiting to happen. And the system is already drowning in liability. Don’t make it worse by turning every appointment into a courtroom drama.
Kiruthiga Udayakumar
January 16, 2026 AT 01:08As an Indian woman who took care of my grandmother through three hospital stays, I want to say: this is beautiful. But also, so very American.
In India, we don’t 'bring advocates.' We bring the whole family. Three aunts, two cousins, the neighbor who works at the pharmacy, the uncle who used to be a nurse in Kuwait-everyone shows up. We argue over pills. We cry. We laugh. We eat samosas in the waiting room.
You think this is about paperwork? No. It’s about love. It’s about community. You don’t need a form. You need people who care.
And yes, we miss things. But we never give up. Not because we’re trained. Because we’re family.
Maybe the real solution isn’t certification. Maybe it’s remembering that we’re not alone.
tali murah
January 17, 2026 AT 19:46Let’s be honest: this entire article is performative allyship wrapped in a PowerPoint deck.
Yes, bring your advocate. Yes, write your questions. Yes, call the pharmacy. But let’s talk about the real elephant in the room: why are we even in this mess?
Because the U.S. healthcare system is a predatory, profit-driven nightmare. You don’t need an advocate-you need a revolution.
And while you’re sitting there color-coding pill bottles, the insurance company is raising premiums, the hospital is billing you $200 for a Band-Aid, and the doctor is seeing 30 patients an hour because they’re drowning in admin.
So yes, bring your cousin. Write your list. Take your photos.
But don’t mistake survival for justice.
Diana Stoyanova
January 19, 2026 AT 17:13Y’all, I’m not a doctor, I’m not a nurse, I’m not even a certified advocate-I’m just a 32-year-old who lost her dad because no one checked his meds.
He was on five pills. The doctor added a sixth. No one asked if he was taking anything else. No one asked if he’d had a reaction before. He died of internal bleeding. It was preventable.
So yeah, I bring my notebook. I bring my phone to record. I bring my anxiety. I bring my rage.
And if you think that’s too much? Good. You should be uncomfortable. Because if you’re not, you’re not trying hard enough.
Don’t wait until it’s too late. Bring someone. Even if it’s your dog. (My dog listens better than my brother anyway.)
We’re not asking for miracles. We’re asking for a chance to live.
Jenci Spradlin
January 21, 2026 AT 14:11lol i just brought my bf to my last appt and he kept saying 'but what about the side effects?' like he was in a medical drama. i had to shush him.
but honestly? he caught that the doc wrote '20mg' but the script said '10mg'. so i guess he helped.
also i forgot to bring the bottles. my bad. but i did take pics of the pills on my phone. that helped.
pharmacist was chill. said 'good job bringing someone.'
so yeah. do it. even if you're bad at it. better than nothing.
Elisha Muwanga
January 22, 2026 AT 20:13This is exactly what’s wrong with America. We’ve turned healthcare into a spectator event where everyone needs a personal hype team just to take a pill.
In my country, people don’t bring advocates. They take responsibility. They read the labels. They ask the doctor. They don’t outsource their health to someone else because they're too lazy to learn.
And now we’re paying for it-literally. Insurance premiums are rising because people treat medicine like a group project.
Stop treating patients like children. Teach them. Don’t hand them a crutch and call it 'empowerment.' It’s infantilization.
Alicia Hasö
January 24, 2026 AT 13:13I’ve been a nurse for 22 years. I’ve seen everything.
And I can tell you this: the patients who bring someone? They live longer. They get fewer ER visits. They don’t end up in nursing homes because they misunderstood their meds.
It’s not about being 'difficult.' It’s about being alive.
I used to roll my eyes when a patient showed up with a binder full of notes. Now I hand them a pen and say, 'What else do you need to know?'
Doctors are rushed. Systems are broken. But love? That’s not broken. That’s the one thing that still works.
Bring your person. Bring your questions. Bring your fear.
And if someone tells you you’re being too much?
Smile. Say, 'Good. I’m glad you noticed.'
You’re not a burden. You’re a lifeline.
Drew Pearlman
January 24, 2026 AT 15:46I know it sounds corny, but I really believe this: healthcare isn’t about the pills. It’s about the people.
My wife had cancer. She couldn’t remember her own name on bad days. So I went with her. I took notes. I asked questions. I cried in the parking lot.
And you know what? The doctor told me once, 'You’re the reason she’s still here.'
That’s not a statistic. That’s a life.
Don’t wait for permission. Don’t wait for a form. Don’t wait until you're 'ready.'
Just show up.
Even if you’re scared.
Even if you’re tired.
Even if you think you’re not enough.
You are.
RAJAT KD
January 25, 2026 AT 16:37Simple truth: if you don’t understand your meds, you’re not alone. But you’re not helpless either.
Bring someone. Write it down. Call the pharmacy.
Done.
No form needed. No certification. No drama.
Just care.
That’s all it takes.
Chris Kauwe
January 25, 2026 AT 23:14Let’s deconstruct the epistemological framework of medical advocacy as presented in this performative discourse. The ontological assumption here is that patient agency is inherently fragmented and requires external epistemic scaffolding-a neoliberal biopolitical strategy that pathologizes cognitive load and commodifies relational care.
The 'advocate' functions as a prosthetic for systemic failure, redistributing epistemic labor from the institution to the familial unit while absolving the healthcare complex of structural accountability.
Moreover, the 'color-coded chart' is a symptom of semiotic overload-a visual hermeneutic band-aid on a hemorrhaging system that prioritizes aesthetic compliance over structural reform.
Until we dismantle the profit-driven architecture of pharmaceutical capitalism, all advocacy is merely aesthetic resistance wrapped in a GoodRx coupon.
Meghan Hammack
January 27, 2026 AT 01:52Author here. Thank you for all of this. I wrote this because I saw my mom almost die from a mix-up. I didn’t know how to help. I wish I’d known then what I know now.
To the ones who say this is too much? I get it. It feels heavy.
But here’s the thing: you don’t have to be perfect. You just have to show up.
And if you’re scared? Me too.
Let’s do this together.