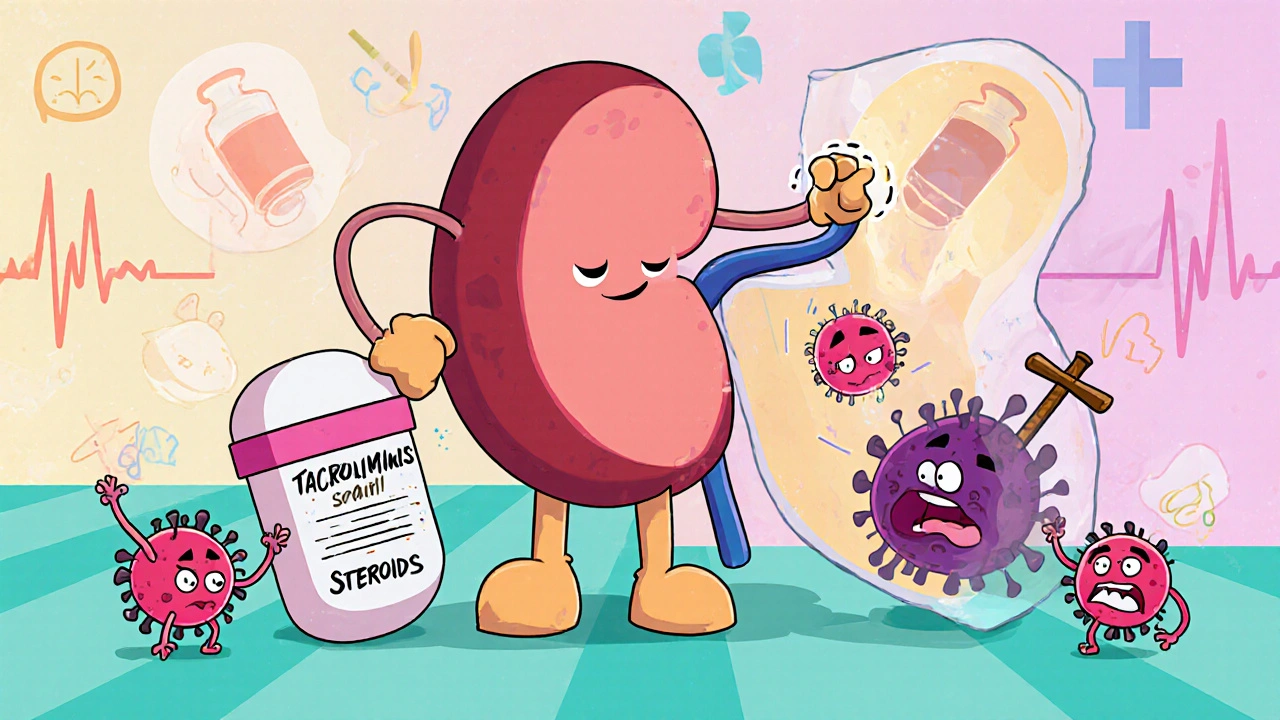
After a kidney transplant, your body doesn’t know the new organ is supposed to be there. It sees it as an invader and tries to attack it. That’s called rejection. To stop that, you need drugs that calm down your immune system. For over 25 years, the most common way to do this has been a three-drug combo: tacrolimus, mycophenolate, and steroids. This isn’t just a random mix - it’s a carefully balanced system designed to prevent rejection without completely shutting down your body’s defenses.
Why This Three-Drug Combo Became the Standard
Before the mid-1990s, most transplant patients took cyclosporine, another immunosuppressant. But it had big problems: high rates of rejection, kidney damage over time, and nasty side effects like shaky hands and excessive hair growth. When tacrolimus came along, it worked better. Then mycophenolate joined the team. Together, they cut rejection rates in half compared to older regimens. A major study in 1998 showed that patients on tacrolimus plus mycophenolate and steroids had only an 8.2% chance of biopsy-proven acute rejection in the first year. Those on tacrolimus and steroids alone? Over 21%. That’s a 61% drop in rejection risk. That’s why, today, around 90% of kidney transplant centers in the U.S. still use this triple therapy as their starting point.How Each Drug Works
These three drugs don’t work the same way. They hit different parts of your immune system, which is why they’re so powerful together.Tacrolimus is a calcineurin inhibitor. It stops T-cells - the main soldiers in your immune system - from getting activated. You take it twice a day, usually in the morning and evening. It hits your bloodstream fast, within an hour or two, but its effects last about 12 hours. That’s why timing matters. Too little, and rejection can happen. Too much, and you risk kidney damage, tremors, or even diabetes. Doctors aim to keep your blood level between 5 and 10 ng/mL during the first year. Monitoring isn’t just about checking a number once a week - it’s about understanding how your body absorbs it, how other meds interact with it, and how your diet affects it. Some people need higher doses. Others get side effects even at low levels. It’s personal.
Mycophenolate (often sold as mycophenolate mofetil or MMF) blocks a different pathway. It stops white blood cells from multiplying. You take it as two pills a day, usually 1 gram each. But here’s the catch: about one in three people can’t stick with the full dose. Why? Stomach problems. Diarrhea, nausea, vomiting - they’re common. Some get low white blood cell counts (leukopenia), which increases infection risk. If side effects hit, doctors often cut the dose to 500 mg twice a day. A few patients stop it altogether. That’s not ideal - studies show that staying on mycophenolate longer is linked to better long-term kidney survival. It’s not just a blocker; it’s a protector for your new organ.
Steroids (usually prednisone or methylprednisolone) are the heavy hitters. They’re given as a big IV dose right in the operating room - often 1,000 mg - to instantly suppress the immune system right after transplant. Then comes the taper. By week three or four, you’re down to 15 mg a day. By three months, most people are on 10 mg. Steroids are fast, effective, and cheap. But they’re also the reason so many transplant patients gain weight, get acne, or grow facial hair. They raise blood sugar, weaken bones, and can trigger mood swings. That’s why doctors are trying to get people off them as soon as possible.
Side Effects You Can’t Ignore
No one talks enough about how these drugs change your life. You’re not just taking pills - you’re managing a new reality.Post-transplant diabetes is real. About 1 in 5 people on this combo develop it. It’s not always because you ate too much sugar. Tacrolimus directly interferes with insulin production. Some people need insulin. Others control it with diet and metformin. Either way, it’s another chronic condition to manage.
Diarrhea from mycophenolate isn’t just annoying - it’s dangerous. If you’re losing fluids and nutrients, your body can’t heal. Some patients end up in the hospital. Doctors now recommend taking mycophenolate at least two hours apart from tacrolimus to reduce stomach upset. Also, avoid proton pump inhibitors like omeprazole. They make mycophenolate less effective. That’s something your pharmacist should catch - but if they don’t, you need to speak up.
Steroids cause more than weight gain. They thin your skin. You bruise easily. Your bones lose density. Many patients end up on calcium and vitamin D supplements, and sometimes even bone-strengthening drugs. And then there’s the emotional toll. Mood swings, anxiety, insomnia - steroids can make you feel like you’re losing control of your own mind.
Can You Skip the Steroids?
Yes. And more people are.In 2005, a major study showed that patients who got a special induction drug called daclizumab (now discontinued, but replaced by similar agents like basiliximab) plus tacrolimus and mycophenolate had the same rejection rates as those on the full steroid combo. About 89% of those patients stayed steroid-free after six months. No moon face. No belly fat. No brittle bones.
Today, steroid-free regimens are common, especially for low-risk patients - younger, healthy, with a well-matched donor. But it’s not for everyone. High-risk patients - those with prior transplants, high antibody levels, or deceased donor kidneys - still benefit from a short steroid burst. The key is personalization. Your doctor doesn’t just look at your age or kidney function. They look at your genetics, your immune profile, even your gut bacteria.
Monitoring Is Everything
You can’t just take these pills and hope for the best. You need to be tracked closely.Trough levels - the lowest concentration of drug in your blood before your next dose - used to be the gold standard. Now, experts are moving to AUC monitoring: measuring how much drug your body is exposed to over 12 hours. It’s more accurate. It catches people who absorb drugs too fast or too slow. Some centers are starting to use it routinely. It’s not everywhere yet, but it’s the future.
And it’s not just about the drugs. You need regular blood tests for kidney function, blood sugar, white blood cell count, and viral infections like CMV. A single missed appointment can mean the difference between a thriving transplant and a failing one.

What’s Next for Immunosuppression?
The goal isn’t just to keep your kidney alive - it’s to keep you healthy while doing it.Researchers are looking at biomarkers - proteins or genes in your blood - that can tell if rejection is starting before it shows up on a biopsy. Imagine a simple blood test that says, “Your immune system is getting restless,” instead of waiting for your kidney to get damaged.
Pharmacogenomics is another big area. Some people have gene variants that make them break down tacrolimus faster. Others process mycophenolate slowly. In the next five years, we’ll likely see dosing based on your DNA, not just your weight or blood level.
And yes, steroid use will keep dropping. New drugs like belatacept - which works differently than calcineurin inhibitors - are already being used in some places. They avoid kidney toxicity and diabetes risk. But they’re expensive and require weekly IV infusions. Not ideal for everyone.
Still, the core of this regimen - tacrolimus, mycophenolate, and steroids - remains the backbone. Even as we move toward more personalized medicine, these three drugs will be the reference point. Because despite all the advances, no other combo has matched their balance of power and predictability.
What This Means for You
If you’re on this regimen, you’re not just a patient. You’re part of a system that’s saved hundreds of thousands of lives. But it’s not perfect. It’s heavy. It’s demanding. You’ll need to be your own advocate.Ask questions. Track your symptoms. Tell your team if you’re having trouble with side effects. Don’t stop a drug because you’re tired of the diarrhea - talk to your doctor. There might be a lower dose, a different brand, or a timing trick that helps.
And remember: this isn’t about living with drugs. It’s about living with a second chance. The fact that you’re reading this means your transplant is working. That’s huge. Keep going.
Can I stop taking my immunosuppressants if my kidney is working fine?
No. Stopping immunosuppressants, even if your kidney feels fine, almost always leads to rejection within days or weeks. The immune system doesn’t “forget” it’s supposed to attack the transplant. There are rare experimental cases where patients have been weaned off drugs under strict monitoring, but this is only done in research settings with advanced biomarkers. For everyone else, lifelong immunosuppression is necessary.
Why do I need to take tacrolimus and mycophenolate at different times?
Taking them together can increase stomach upset and reduce how well mycophenolate is absorbed. Spacing them out by 2 to 4 hours helps your body handle both drugs better. It’s a small change, but many patients report less nausea and diarrhea when they follow this timing.
Does mycophenolate cause cancer?
All immunosuppressants slightly raise cancer risk because they slow down your immune system’s ability to spot abnormal cells. Mycophenolate carries a small increased risk of skin cancer and lymphoma. That’s why regular skin checks and avoiding sun exposure are critical. The benefit of preventing rejection far outweighs this risk for most patients, but it’s something you need to monitor.
Can I drink alcohol while on these drugs?
Moderate alcohol is usually okay - one drink a day for women, two for men - but it’s risky. Alcohol can damage your liver, which is already working hard to process these drugs. It can also raise blood pressure and blood sugar, which are already concerns with tacrolimus and steroids. Many transplant centers recommend avoiding alcohol entirely, especially in the first year.
What happens if I miss a dose?
Missing one dose occasionally won’t cause immediate rejection, but it increases your risk. If you miss a tacrolimus dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Then skip it. Never double up. For mycophenolate, try to stay as close to your schedule as possible. Missing doses regularly is one of the top reasons for late rejection. Set phone alarms. Use pill organizers. Talk to your pharmacist about blister packs.
Are there natural supplements I can take to reduce side effects?
Absolutely not without talking to your transplant team first. Many supplements - like St. John’s wort, echinacea, grapefruit juice, and high-dose vitamin C - interfere with how your body processes tacrolimus and mycophenolate. Grapefruit juice can make tacrolimus levels spike dangerously. St. John’s wort can drop them to ineffective levels. Even fish oil and garlic can affect bleeding risk. What’s natural isn’t always safe.
 Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
 Lower GI Bleeding: Diverticula, Angiodysplasia, and How to Diagnose It
Lower GI Bleeding: Diverticula, Angiodysplasia, and How to Diagnose It
 Rickets and the Endocrine System: How They’re Linked
Rickets and the Endocrine System: How They’re Linked
 How to Prevent Wrong-Patient Errors at the Pharmacy Counter
How to Prevent Wrong-Patient Errors at the Pharmacy Counter
 Buy Generic Prilosec (Omeprazole) Online in Australia: Cheap, Safe Options for 2025
Buy Generic Prilosec (Omeprazole) Online in Australia: Cheap, Safe Options for 2025
Douglas Fisher
November 27, 2025 AT 08:47Just wanted to say thank you for writing this. I’ve been on this combo for 7 years now, and no one ever explains how it actually works-just ‘take your pills.’ The breakdown of each drug’s role? Perfect. I finally understand why my doc keeps nagging me about timing. Also, the part about mycophenolate and PPIs? My pharmacist missed that. I’m switching to famotidine tomorrow.
Cynthia Boen
November 28, 2025 AT 08:41This is why medicine is broken. You’re telling people to take 5 pills a day, monitor their blood sugar, avoid grapefruit, space out meds, get biopsies, and still get diabetes and cancer risk? And you call this ‘second chance’? It’s a life sentence with extra steps.
Amanda Meyer
November 30, 2025 AT 06:45While I appreciate the clinical precision of this post, I must push back on the assumption that all patients have equal access to monitoring, pharmacogenomic testing, or even consistent pharmacy access. The ‘personalized medicine’ future you describe is still a luxury for the insured and the privileged. Many of us are just trying to keep our levels stable with a $200 co-pay and a 3-hour bus ride. The science is brilliant-but the system isn’t.
Jesús Vásquez pino
December 1, 2025 AT 14:37Hey, I’m a transplant recipient too. I got mine in 2020. I stopped steroids after 6 weeks-no issues. But I also had a living donor, zero antibodies, and a doc who actually listened. I get that this works for most-but if you’re on this combo and you’re miserable, ask for alternatives. Belatacept isn’t magic, but it’s less toxic. And yes, I know it’s IV. But I’d rather get a shot every 2 weeks than wake up with moon face again.
hannah mitchell
December 2, 2025 AT 11:19Thanks for posting this. I read it during my dialysis appointment. It made me feel less alone.
vikas kumar
December 3, 2025 AT 08:15As someone from India, I’ve seen how expensive this combo is here. Tacrolimus alone costs 3x what it does in the US. My cousin’s transplant was funded by community donations. But the real issue? No one tells you about the mental toll. You’re not just managing meds-you’re managing guilt. ‘Did I eat too much sugar? Did I miss a pill? Is my kidney failing?’ It never stops. Keep talking about this. We need more honesty.
Vanessa Carpenter
December 3, 2025 AT 19:02I’ve been on this regimen for 12 years. My kidney’s still working. I’ve gained weight, I have osteoporosis, and I take 11 pills a day. But I’m alive. And I get to see my granddaughter grow up. That’s worth the trade-offs. I don’t complain. I just take my pills. And I thank the scientists who made this possible.
Bea Rose
December 4, 2025 AT 09:53Post-transplant diabetes isn’t ‘real’-it’s just poor lifestyle choices masked as medical necessity. If you’re eating sugar and not exercising, don’t blame tacrolimus. Also, your ‘steroid-free’ stats are cherry-picked. Most of those patients had perfect donors and zero comorbidities. Real people aren’t that lucky.
Michael Collier
December 4, 2025 AT 17:02It is with profound respect for the scientific rigor and clinical insight presented herein that I offer the following observation: the pharmacokinetic variability of tacrolimus, particularly in relation to CYP3A4/5 polymorphisms, remains an underappreciated variable in routine clinical practice. The transition from trough-level monitoring to AUC-based dosing represents not merely an incremental improvement, but a paradigm shift toward precision immunosuppression. I urge all transplant centers to adopt therapeutic drug monitoring protocols aligned with the 2022 KDIGO guidelines.
Shannon Amos
December 5, 2025 AT 06:37So let me get this straight… you’re telling me I have to take 3 drugs, avoid grapefruit, space out pills, get biopsies, watch my sugar, and still get cancer? And the solution is… more drugs? I’m just here for the free t-shirt and the ‘you’re a warrior’ sticker.
Wendy Edwards
December 5, 2025 AT 14:51OMG I’ve been on this combo since 2019 and I thought I was the only one who got soooo tired of the diarrhea. I started taking my mycophenolate at 7am and tacrolimus at 11am and it’s like night and day. No more panic attacks before work because I had to be near a bathroom. Also, I stopped grapefruit juice and my levels stabilized. I’m alive because I listened to my body, not just the doctor. You’re not broken-you’re adapting. Keep going 💪
Damon Stangherlin
December 5, 2025 AT 16:08Just wanted to add something important: if you're on tacrolimus and you're taking any OTC pain meds, check with your pharmacist before taking NSAIDs like ibuprofen. They can raise your creatinine and mask early signs of rejection. I missed a dose once because I took Advil for a headache-my creatinine jumped 0.4 in 48 hours. Now I use acetaminophen and set 4 alarms a day. It's a pain, but your kidney doesn't care if you're tired. It just needs you to be consistent.