Kidney Transplant Immunosuppression: Drugs, Risks, and What You Need to Know
When your body gets a new kidney, it doesn’t see it as a gift—it sees it as an invader. That’s where kidney transplant immunosuppression, the medical process of suppressing the immune system to prevent organ rejection after transplantation. It’s not optional. Without it, your body will attack the new kidney, often within days. This isn’t just about taking pills. It’s a lifelong balance: too little drug, and your immune system destroys the transplant; too much, and you’re at risk for infections, cancer, or organ damage.
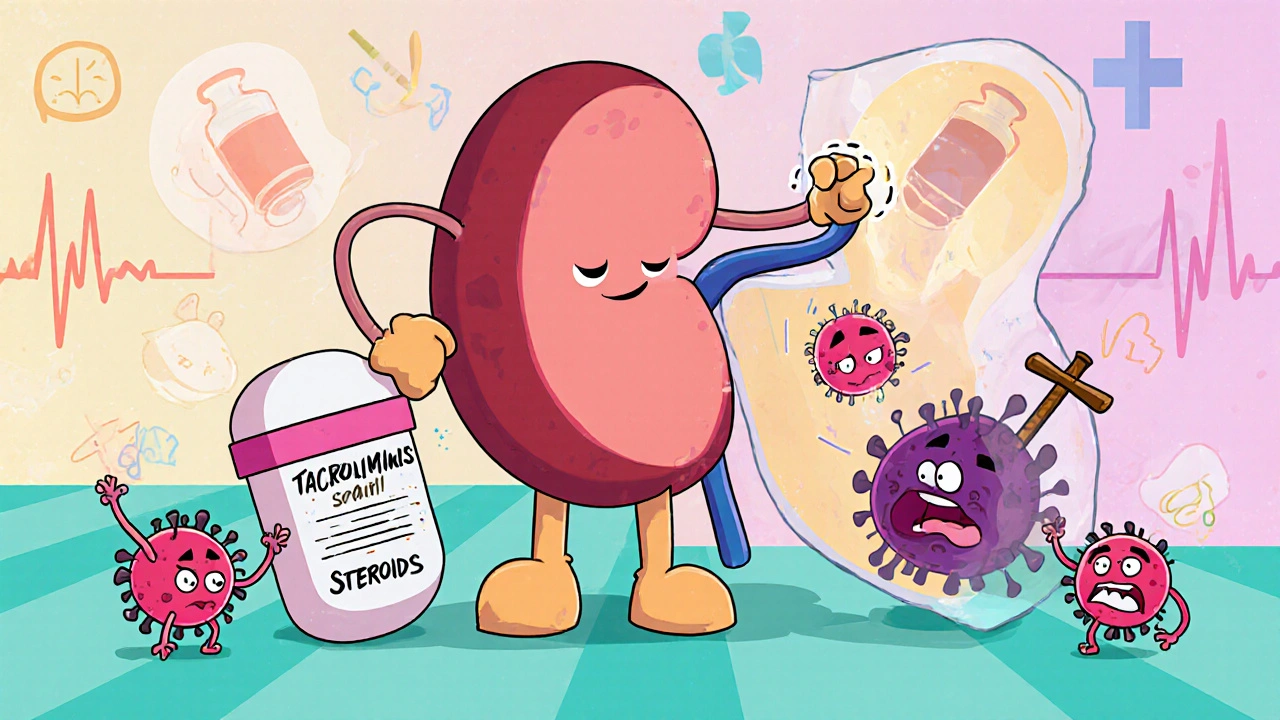
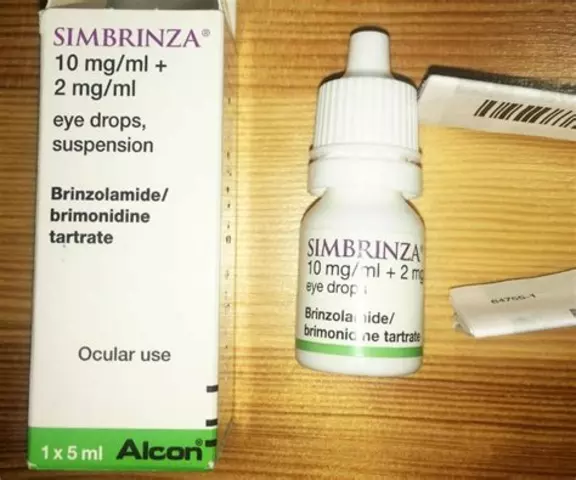
The main tools here are immunosuppressive drugs, medications designed to weaken the immune response to protect transplanted organs. Common ones include tacrolimus, cyclosporine, mycophenolate, and prednisone. Each works differently—some block T-cells, others stop cell division. Doctors often mix them to lower doses and reduce side effects. But there’s no one-size-fits-all. What works for one person might cause kidney damage or high blood pressure in another. That’s why regular blood tests and dose tweaks are part of the routine. And while these drugs save lives, they don’t come without trade-offs. You’ll need to avoid raw sprouts, undercooked meat, and crowded places during flu season. Even a simple cold can turn dangerous. Some patients develop diabetes, high cholesterol, or bone thinning over time. The goal isn’t to eliminate risk—it’s to manage it so your new kidney lasts as long as possible.
transplant rejection, the immune system’s attack on a transplanted organ, often occurring without obvious symptoms. It can happen anytime, even years after surgery. Many rejections are silent—detected only through blood work or biopsy. That’s why sticking to your medication schedule isn’t just important, it’s non-negotiable. Missing a dose, even once, can trigger a chain reaction your body can’t recover from. And while newer drugs and monitoring tools are making rejection less common, the threat never fully goes away. Then there’s anti-rejection medication, the broad term for drugs used to prevent the immune system from attacking a transplanted organ. These aren’t just pills you take forever—they’re the reason you’re alive today. But they’re also the reason you need to stay in close contact with your transplant team, get regular labs, and never ignore weird symptoms like fever, swelling, or sudden fatigue.
You’ll find posts here that cut through the noise. No fluff. Just real talk about how these drugs interact, what side effects actually matter, how to spot early signs of trouble, and what alternatives exist when one drug stops working. Whether you’re a patient, a caregiver, or just trying to understand what happens after a transplant, this collection gives you the facts you need to ask better questions and make smarter choices.