Rickets Risk Assessment Tool
Please answer the following questions to assess your child's risk for developing rickets.
Risk Assessment Result
Ever wondered why a lack of sunlight can make children’s bones bend and grow oddly? That’s not just a myth - it’s a real medical condition called rickets that sits at the crossroads of nutrition, hormones, and bone development. In the next few minutes, you’ll see how the endocrine system talks to your skeleton, why vitaminD is the star player, and what you can do to keep the conversation healthy.
Key Takeaways
- Rickets is a disease of bone softening caused mainly by vitaminD or calcium deficiency.
- The endocrine system, especially parathyroid hormone (PTH) and growth hormone, reacts to low mineral levels and can worsen or help resolve rickets.
- Sunlight, diet, and supplementation are the three pillars of prevention and treatment.
- Regular monitoring of serum 25‑hydroxyvitaminD, calcium, and alkaline phosphatase helps track recovery.
- Early intervention protects growth plates, reduces deformities, and supports lifelong bone health.
What Is Rickets?
Rickets is a pediatric disorder characterized by inadequate mineralization of the growing skeleton. It typically appears in children under five, manifesting as bowed legs, widened wrists, delayed dental eruption, and, in severe cases, seizures due to hypocalcemia. The root cause is usually insufficient vitaminD, which impairs calcium and phosphate absorption from the gut.
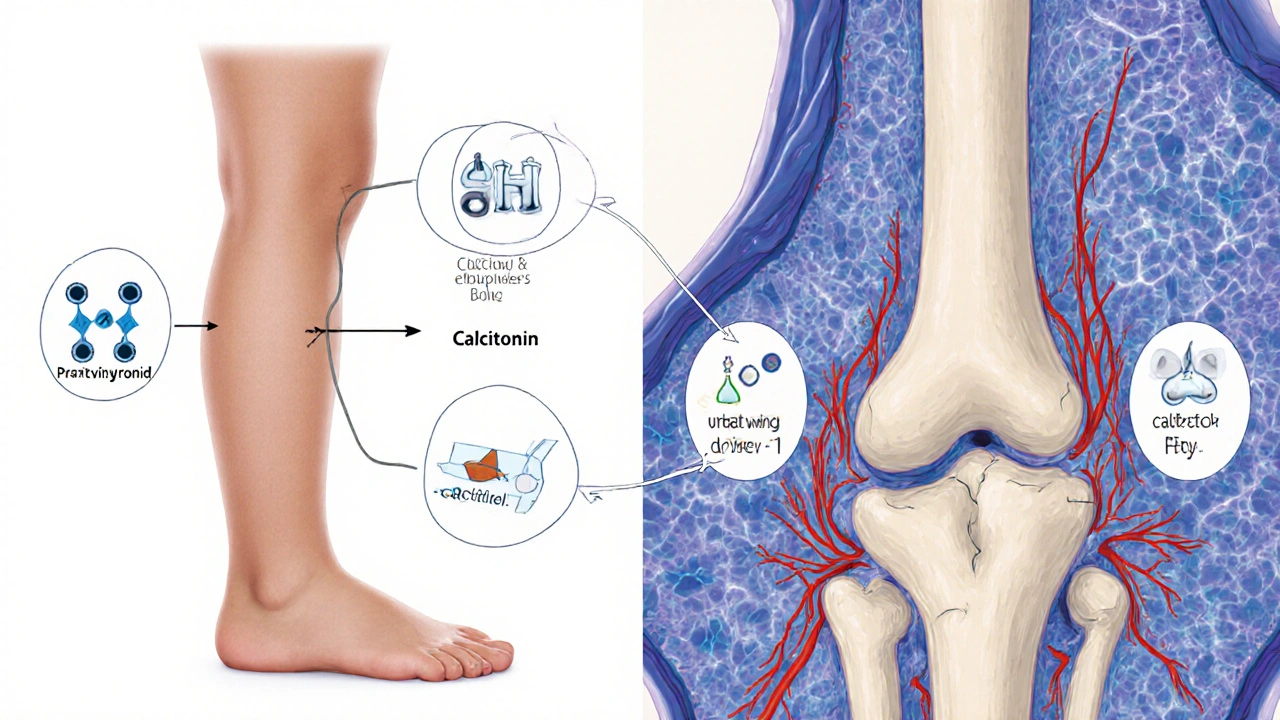
The Endocrine System’s Role in Bone Health
Bone is not a static structure; it’s a living tissue constantly shaped by hormones. The endocrine system releases several key messengers that regulate calcium balance, bone turnover, and growth. The most relevant players for rickets are:
- Parathyroid hormone (PTH): rises when blood calcium drops, stimulating kidneys to re‑absorb calcium and activating vitaminD.
- Growth hormone (GH) and its downstream factor Insulin‑like growth factor‑1 (IGF‑1): drive cartilage proliferation at growth plates, but need adequate mineral supply to harden the new bone.
- Calcitonin: released by thyroid C‑cells, it lowers blood calcium and slows bone resorption-counterbalancing PTH.
- Thyroid hormone: influences overall metabolism and indirectly affects bone turnover.
When vitaminD levels are low, PTH spikes (secondary hyperparathyroidism). This chronic elevation increases bone turnover without giving the skeleton enough calcium to rebuild, leading to the soft, pliable bones seen in rickets.
VitaminD: The Hormone That Behaves Like a Vitamin
VitaminD is unique because it works like a hormone. Sun‑exposed skin converts 7‑dehydrocholesterol into cholecalciferol (vitaminD3), which the liver then hydroxylates to 25‑hydroxyvitaminD, the main circulating form. Kidneys add a second hydroxyl group, making 1,25‑dihydroxyvitaminD (calcitriol), the active hormone that tells the intestines to absorb calcium and phosphate.
If any step in this chain falters-poor sun exposure, dark skin, liver or kidney disease-the downstream calcium uptake drops, PTH rises, and rickets can develop.
Calcium and Phosphate: The Building Blocks
While vitaminD opens the door for mineral absorption, the actual bricks are calcium and phosphate. Dietary sources include dairy, leafy greens, fortified cereals, and fish with edible bones. In rickets, serum calcium may be low‑normal, but phosphate is often markedly reduced because PTH pushes phosphate into the urine.
Maintaining a calcium‑phosphate product above 30 mg²/dL² is a useful clinical target for healing.
Nutrition, Sunlight, and Supplementation: The Three‑Pillar Strategy
Effective rickets management combines three practical steps:
- Sunlight exposure: Aim for 10‑15 minutes of midday sun on uncovered arms and legs, 2-3 times per week, for children with light skin. Darker‑skinned children may need longer or additional supplementation.
- Dietary intake: Encourage calcium‑rich foods-milk, yogurt, cheese, fortified soy or almond milks, sardines, and leafy greens like kale. Pair with a source of vitaminD such as oily fish or fortified eggs.
- Supplementation: When diet and sun are insufficient, give vitaminD3 drops at 400-1000 IU/day for infants, higher doses (2000-4000 IU/day) for confirmed deficiency, and calcium supplements if intake stays below 500 mg/day.
Regular labs should be checked after 4-6 weeks of therapy: serum 25‑hydroxyvitaminD >30ng/mL, calcium within age‑appropriate range, and alkaline phosphatase trending down.
Monitoring Hormonal Responses: When PTH Becomes a Problem
Secondary hyperparathyroidism can persist even after vitaminD levels improve, especially in chronic kidney disease. In such cases, a pediatric nephrologist may add active forms of vitaminD (calcitriol) or phosphate binders. The goal is to bring PTH back to the lower end of the reference range, letting bone formation catch up.
Complications if Left Untreated
Unaddressed rickets can lead to:
- Permanent deformities of the lower limbs, requiring orthopedic surgery.
- Growth retardation due to damaged growth plates.
- Hypocalcemic seizures, especially in infants.
- Reduced peak bone mass, increasing osteoporosis risk later in life.
Early endocrine intervention-normalizing PTH and vitaminD-greatly reduces these risks.
Quick Reference Table: Nutrients, Hormones, and Their Bone Impact
| Entity | Type | Primary Action on Bone | Typical Deficiency Effect |
|---|---|---|---|
| VitaminD | Hormone | Enhances intestinal calcium & phosphate absorption | Rickets, secondary hyperparathyroidism |
| Calcium | Mineral | Provides hydroxyapatite crystals for bone hardness | Bone demineralization, muscle cramps |
| Phosphate | Mineral | Combines with calcium to form hydroxyapatite | Weak bones, dental abnormalities |
| Parathyroid Hormone (PTH) | Hormone | Raises blood calcium, increases bone resorption | High PTH → bone loss, low phosphate |
| Growth Hormone (GH) | Hormone | Stimulates growth‑plate cartilage proliferation | Growth retardation if mineral supply is inadequate |
Practical Tips for Parents and Caregivers
- Check your child’s skin tone and local UV index. In winter or high‑latitude regions, supplement more aggressively.
- Track daily calcium intake with a simple food diary; aim for 500-800mg for toddlers, 1300mg for pre‑teens.
- Schedule a blood test if you notice delayed walking, knobby knees, or persistent irritability.
- Ask your pediatrician about measuring serum alkaline phosphatase-a quick marker of bone turnover.
- Remember that fortified plant milks are a reliable calcium source for lactose‑intolerant families.
Frequently Asked Questions
Can adults get rickets?
True rickets primarily affects growing bones, so it is rare in fully mature adults. However, severe vitaminD deficiency in adults can cause osteomalacia, a similar softening of bone that leads to muscle weakness and fractures.
Why is sunlight better than supplements?
Sunlight triggers the body’s natural synthesis of vitaminD3, which is more efficiently regulated than oral doses. The skin‑derived vitaminD also produces a steady, low‑level supply that reduces the risk of overdose.
How long does it take for bone deformities to reverse?
With adequate vitaminD and calcium, biochemical markers improve in 4-6weeks. Visible correction of mild bowing may take 6-12months, depending on age and severity. Severe deformities often need orthopedic intervention.
Is genetic rickets different from nutrient‑deficiency rickets?
Yes. Genetic forms, such as X‑linked hypophosphatemic rickets, involve mutations that affect phosphate handling regardless of vitaminD status. Treatment focuses on phosphate supplements and active vitaminD analogs, not just sun or diet.
What lab values confirm rickets?
Typical findings are serum 25‑hydroxyvitaminD < 20ng/mL, calcium low‑normal, phosphate low, elevated alkaline phosphatase, and secondary‑elevated PTH. Radiographs show widened growth plates and cupping of metaphyses.
Understanding the hormonal dance behind rickets turns a scary diagnosis into a manageable condition. By keeping vitaminD levels up, feeding the bones the calcium and phosphate they crave, and watching the endocrine feedback loops, you give your child a solid foundation for a healthy, active life.

 Online Pharmacy roidsource.net Review: Safe Steroid Buying Guide
Online Pharmacy roidsource.net Review: Safe Steroid Buying Guide
 Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
Weekend Weight Gain: How to Stop Calorie Creep and Prevent Regain
 Exploring 7 Effective Alternatives to Atarax for Anxiety Relief and Allergy Management
Exploring 7 Effective Alternatives to Atarax for Anxiety Relief and Allergy Management
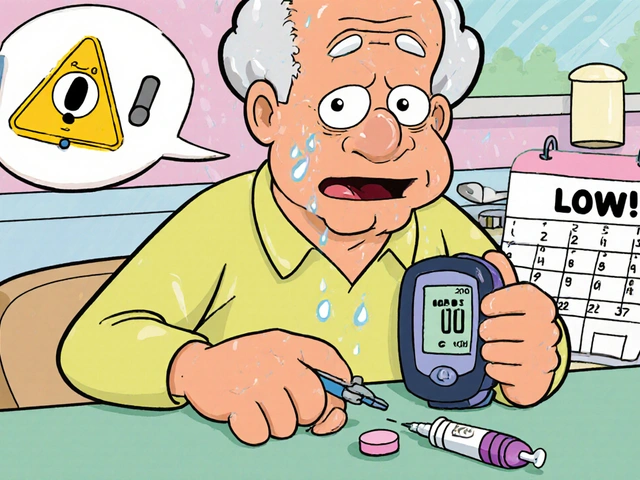 Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
 Celebrex: What You Need to Know About This Arthritis & Pain Relief Medication
Celebrex: What You Need to Know About This Arthritis & Pain Relief Medication
Christina Burkhardt
October 4, 2025 AT 02:25Great overview of how the endocrine system ties into rickets. It's crucial for parents to understand the role of vitamin D, calcium, and PTH when they see those bone changes. Keeping track of sunlight exposure and dietary sources can make a huge difference for kids.
liam martin
October 4, 2025 AT 04:38One could argue that the shadows of deficiency stretch far beyond the obvious bone pain, whispering of a deeper malaise. Yet we stand, watching the sun rise and set, hoping the light will heal what the plates cannot. It's a quiet drama playing out on the tiny frames of our future.
Ria Ayu
October 4, 2025 AT 06:51Thinking about the hormonal dance reminds me of a gentle river that must flow just right. When vitamin D is low, the river slows, and the banks-our bones-start to erode. A friendly reminder: a little daily sunshine and fortified foods go a long way.
maya steele
October 4, 2025 AT 09:05From a clinical perspective, the interplay between parathyroid hormone and vitamin D is a cornerstone of pediatric bone health.
When serum 25‑hydroxyvitamin D dips below 20 ng/mL, PTH begins to rise in an effort to maintain calcium homeostasis.
This secondary hyperparathyroidism accelerates bone resorption, manifesting as metaphyseal cupping and rachitic rosary.
Therapeutic intervention should therefore aim first at repleting vitamin D, using age‑appropriate dosing of cholecalciferol.
Concurrently, calcium intake must be optimized-approximately 500 mg/day for infants and up to 1300 mg/day for early adolescents.
Monitoring alkaline phosphatase provides a rapid biochemical gauge of bone turnover; a falling trend indicates therapeutic response.
Radiographic evaluation, while not routinely required, can confirm resolution of widened growth plates after 3–6 months of treatment.
In cases of genetic rickets, such as X‑linked hypophosphatemic rickets, phosphate supplementation and active vitamin D analogues are indicated.
Nephrological comorbidities demand calcitriol or phosphate binders to curb persistent PTH elevation.
It is also prudent to assess for concurrent deficiencies, including magnesium, which can blunt the response to vitamin D therapy.
Family education should emphasize the importance of consistent sunlight exposure, especially during winter months at higher latitudes.
Fortified milks, cereals, and leafy greens serve as reliable dietary sources of calcium and vitamin D.
Regular follow‑up labs-vitamin D, calcium, phosphate, PTH, and alkaline phosphatase-should be obtained every 2–3 months until stability is achieved.
Once biochemical parameters normalize, the frequency of testing can be reduced to semi‑annual checks.
Finally, an interdisciplinary approach involving pediatricians, endocrinologists, and dietitians ensures comprehensive care and minimizes the risk of long‑term complications.
Sharon Lax
October 4, 2025 AT 11:18While the article is thorough, it leans heavily on textbook jargon without addressing real‑world compliance barriers. The clinical lexicon-"secondary hyperparathyroidism," "alkaline phosphatase trending down"-may alienate the very caregivers who need actionable steps.
Benjamin Cook
October 4, 2025 AT 13:31Absolutely love the practical tips!!! Remember to check the vitamin D dosage on the label-some brands are way off!!! Also, a quick reminder: kids love cheese sticks, so sprinkle that calcium!!
karthik rao
October 4, 2025 AT 15:45Interesting take, but the article glosses over the socioeconomic dimensions of rickets. Access to fortified foods and safe sunlight exposure is uneven across communities. 🌍📊 Moreover, the recommendation for routine blood tests may be impractical for families without insurance. 📈💡 It would be more balanced to discuss low‑cost alternatives, such as community health screenings.
Ashika Amirta varsha Balasubramanian
October 4, 2025 AT 17:58Indeed, equity matters. In many regions, fortified staples like millets and soy milk can bridge the gap where dairy is scarce. Encouraging cultural dietary patterns while ensuring adequate calcium and vitamin D is both respectful and effective.
April Yslava
October 4, 2025 AT 20:11The government isn’t telling us the truth about why kids get rickets-look at the chemical additives in our food supply. It’s a hidden agenda to keep us dependent on pharma. Wake up and demand natural sunlight, not synthetic supplements.
Daryl Foran
October 4, 2025 AT 22:25Statistically, the prevalence of rickets correlates more strongly with latitude and skin pigmentation than any alleged conspiracy. The data shows a clear pattern that aligns with established physiology.
Paul Griffin
October 5, 2025 AT 00:38Thank you for the balanced guidelines. A systematic approach to assessment, supplementation, and follow‑up can empower clinicians and families alike.
Michael Tekely
October 5, 2025 AT 02:51Just a heads up-if you’re tracking calcium, watch out for hidden sources in processed snacks. Also, keep an eye on vitamin D levels during the winter months when UVB is low.
Oscar Taveras
October 5, 2025 AT 05:05Optimism is key! 🌞 With the right vitamin D and calcium, kids can bounce back stronger than ever. Keep the spirit high and the supplements consistent! 😊
Lindsey Crowe
October 5, 2025 AT 07:18Sure, because everyone loves reading dense medical jargon on a weekend.
Rama Hoetzlein
October 5, 2025 AT 09:31Wow, you really think a simple vitamin drop fixes everything? 🙄 The industry profits from these oversimplifications. 🏦💊
Lorena Garcia
October 5, 2025 AT 11:45I’m curious-has anyone tried tracking sunlight exposure with a smartphone app? It might help families quantify their outdoor time more accurately.
Dietra Jones
October 5, 2025 AT 13:58Thats a gud tip, but i cant remmeber wht i ate yesturday lol