Introduction: Tendonitis and Lyme Disease
In recent years, there has been a growing awareness of the connection between tendonitis and Lyme disease. As a blogger on health and wellness, I have come across numerous cases where patients suffering from tendonitis eventually discovered they were also battling Lyme disease. In this article, I will explore this connection, discuss the symptoms and causes of both conditions, and provide some helpful tips on prevention and treatment. By understanding the link between tendonitis and Lyme disease, you can better protect your own health and that of your loved ones.
Understanding Tendonitis: Causes and Symptoms
Tendonitis is a painful condition that affects the tendons, which are the fibrous tissues connecting muscles to bones. It is often caused by repetitive motion or overuse of a particular joint, leading to inflammation and irritation of the tendon. The most common areas affected by tendonitis include the shoulder, elbow, wrist, knee, and Achilles tendon. Some of the typical symptoms of tendonitis are pain, swelling, and stiffness around the affected joint, which often worsen with movement.
There are several factors that can contribute to the development of tendonitis, including age, occupation, and certain sports activities. As we age, our tendons become less flexible and more prone to injury. People who perform repetitive tasks in their jobs, such as typing or assembly line work, are also at a higher risk of developing tendonitis. Additionally, athletes who frequently engage in activities that put stress on specific tendons, like tennis or baseball players, are more likely to experience tendonitis.
Lyme Disease: An Overview
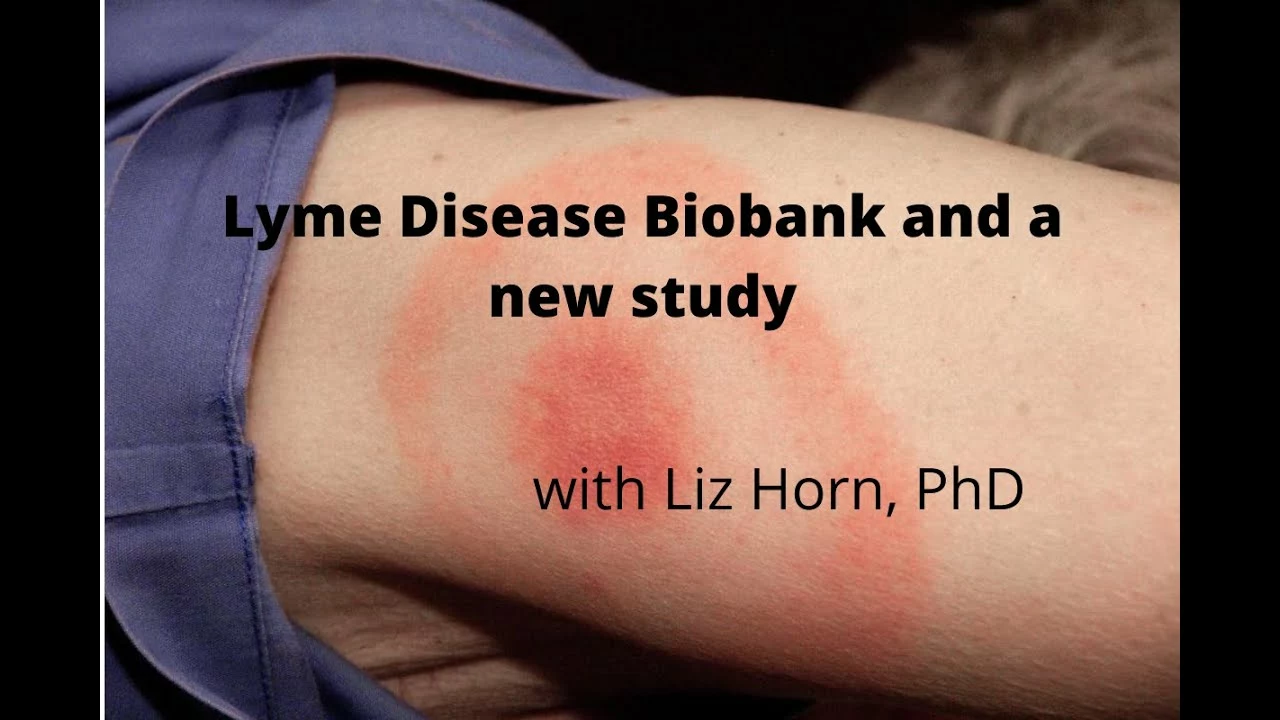
Lyme disease is an infectious disease caused by the bacterium Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks. The early symptoms of Lyme disease can include a rash, fever, headache, fatigue, and muscle or joint aches. If left untreated, the infection can spread to the joints, heart, and nervous system, potentially leading to more severe symptoms and long-term complications.
It is essential to recognize the signs of Lyme disease early and seek prompt medical treatment, as this can significantly reduce the risk of long-term complications. The most effective way to prevent Lyme disease is to avoid tick bites by taking preventive measures such as wearing protective clothing, using insect repellent, and checking your body for ticks after spending time outdoors.
The Connection Between Tendonitis and Lyme Disease
While tendonitis and Lyme disease might seem like unrelated conditions, there is a surprising connection between the two. In some cases, Lyme disease can cause inflammation in the tendons and joints, leading to symptoms that mimic those of tendonitis. This can make it challenging to diagnose Lyme disease, as patients may initially be treated for tendonitis rather than the underlying infection.
Moreover, people with Lyme disease may be more susceptible to developing tendonitis due to the overall weakening of their immune system. The inflammation caused by the Lyme infection can weaken the tendons and make them more prone to injury, especially if the person is already at risk due to factors like age, occupation, or sports activities.
Diagnosing Lyme Disease in Tendonitis Patients
If you are experiencing tendonitis symptoms and suspect that Lyme disease might be the underlying cause, it is crucial to discuss your concerns with a healthcare professional. They may recommend blood tests to check for the presence of Lyme disease antibodies, as well as other diagnostic tests to rule out other potential causes of your symptoms.
Keep in mind that diagnosing Lyme disease can be challenging, as the symptoms can be similar to those of other conditions, and the tests are not always conclusive. Therefore, it is essential to work closely with your healthcare provider and provide them with as much information as possible about your symptoms and medical history.
Treatment Options for Tendonitis and Lyme Disease
The treatment for tendonitis usually involves a combination of rest, ice, compression, and elevation (RICE) to reduce inflammation and promote healing. Over-the-counter pain relievers and anti-inflammatory medications may also be recommended to help alleviate pain and swelling. In more severe cases, physical therapy or even surgery may be required to repair the damaged tendon.
If Lyme disease is found to be the underlying cause of your tendonitis, your healthcare provider will likely prescribe a course of antibiotics to treat the infection. This can help reduce the inflammation in your tendons and joints, allowing your body to heal more effectively. It is crucial to complete the full course of antibiotics and follow any additional treatment recommendations provided by your healthcare provider to ensure the best possible outcome.
Preventing Tendonitis and Lyme Disease
Prevention is always better than cure, and there are several steps you can take to protect yourself from both tendonitis and Lyme disease. To prevent tendonitis, it is essential to practice good ergonomics at work and maintain a healthy level of physical activity. This can help to strengthen your tendons and reduce the risk of injury. Additionally, be mindful of your body's limits and avoid overworking your joints and tendons.
To protect yourself from Lyme disease, take precautions to avoid tick bites while spending time outdoors. This includes wearing long sleeves and pants, using insect repellent, and thoroughly checking your body for ticks after returning indoors. If you find a tick, remove it promptly and safely, and keep an eye out for any symptoms of Lyme disease. Early detection and treatment can significantly reduce the risk of long-term complications.
Final Thoughts
The connection between tendonitis and Lyme disease is an important topic to be aware of, as it can help you recognize the signs of Lyme disease early and seek appropriate treatment. By understanding the symptoms and causes of both conditions, you can take steps to protect your health and minimize your risk of complications. If you suspect that you may have Lyme disease or are experiencing tendonitis symptoms, it is crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
 Why Acetaminophen Helps with Social Pain: Surprising Research Insights
Why Acetaminophen Helps with Social Pain: Surprising Research Insights
 Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
 Potential Benefits of Ibuprofen for Managing Shingles Pain
Potential Benefits of Ibuprofen for Managing Shingles Pain
 The Role of Special Olympics in the Lives of People with Intellectual Disabilities
The Role of Special Olympics in the Lives of People with Intellectual Disabilities
 Terramycin vs Alternative Antibiotics: Tetracycline Comparison Guide
Terramycin vs Alternative Antibiotics: Tetracycline Comparison Guide
Joanne Myers
April 30, 2023 AT 01:56Thank you for illuminating the often‑overlooked intersection between musculoskeletal inflammation and vector‑borne infection; your thorough review underscores the importance of a multidisciplinary diagnostic approach.
rahul s
April 30, 2023 AT 02:36Honestly, most people think tendon pain is just a ‘cheesy gym‑wound’, but ignoring the tick‑born bacteria is a rookie move – get your labs sorted before you blame the dumbbell.
Julie Sook-Man Chan
April 30, 2023 AT 04:00I appreciate the balanced perspective; it’s easy to miss Lyme when treating chronic joint pain, so keeping a broad differential is key.
Amanda Mooney
April 30, 2023 AT 06:46What a comprehensive guide!
First, recognizing that repetitive strain can mask an infectious etiology reminds clinicians to stay vigilant.
Second, the emphasis on early serologic testing can prevent months of unnecessary physiotherapy.
Third, integrating ergonomic education with tick‑avoidance strategies offers a holistic prevention model.
Moreover, the step‑by‑step treatment algorithm – RICE for inflammation, followed by targeted antibiotics if Borrelia is confirmed – provides a clear pathway for patient management.
Additionally, the reminder to complete the full antibiotic course cannot be overstated; premature cessation often leads to relapse.
Fourth, patients should be educated on the signs of both conditions to facilitate self‑monitoring.
Fifth, primary care providers ought to maintain a low threshold for ordering Lyme panels when tendon pain persists.
Sixth, physiotherapists can incorporate anti‑inflammatory modalities while awaiting diagnostic confirmation.
Seventh, interdisciplinary communication between primary care, rheumatology, and infectious disease specialists aligns with best practice standards.
Eighth, insurance coverage considerations should be addressed early to avoid treatment delays.
Ninth, follow‑up appointments must be scheduled to assess response to both antibiotic and rehabilitative therapy.
Tenth, lifestyle modifications such as balanced activity levels and proper footwear can reduce recurrence.
Eleventh, public health messaging on tick avoidance complements clinical efforts.
Twelfth, research into the exact mechanisms linking Borrelia infection with tendon matrix degradation is needed.
Thirteenth, clinicians should remain aware of regional variations in tick prevalence when evaluating patients.
Fourteenth, shared decision‑making ensures patients understand the benefits and risks of prolonged antibiotic use.
Finally, this article equips both patient and provider with actionable knowledge to navigate a complex clinical picture.
Mandie Scrivens
April 30, 2023 AT 09:33Great info, but if you’re not into labs, just check for ticks.
Natasha Beynon
April 30, 2023 AT 12:20Your points on ergonomics and tick awareness are spot‑on; encouraging folks to adopt both habits will undoubtedly reduce the dual burden of tendonitis and Lyme disease.