A cerebral aneurysm isn’t something you hear about until it’s too late. For most people, it’s silent-no symptoms, no warning-until the vessel wall gives way and bleeding starts inside the skull. About cerebral aneurysm affects 1 in 30 adults, and while most never rupture, the ones that do kill nearly 4 out of 10 within the first day. That’s why knowing your risk and understanding your options isn’t just helpful-it’s life-saving.
What Makes a Cerebral Aneurysm Likely to Burst?
Not all brain aneurysms are created equal. Size matters, but it’s not the whole story. An aneurysm larger than 7 mm has over three times the risk of rupture compared to smaller ones. But even a 4 mm aneurysm in the right spot can be dangerous. The anterior communicating artery (AComm), for example, is a known troublemaker. Aneurysms here rupture at nearly 2.5 times the rate of those in other areas-even when they’re small.
Shape is another red flag. If the aneurysm looks like a lumpy balloon with daughter sacs sticking out, your risk jumps by almost 70%. Irregular shapes create chaotic blood flow, stressing the wall until it breaks. And location? Posterior circulation aneurysms (near the brainstem) are more likely to rupture than those in the front of the brain, even if they’re the same size.
Then there’s the body’s role. High blood pressure is the biggest modifiable risk. If your systolic pressure regularly hits 140 or higher, your rupture risk more than doubles. Smoking? It’s worse than you think. Current smokers have over three times the risk of rupture compared to non-smokers. And it’s not just about how many cigarettes-you’re looking at a 47% higher risk if you smoke 10 or more a day. Heavy drinking (more than 14 drinks a week) adds another 32% risk.
Age and gender play their parts too. Women are 1.6 times more likely to have aneurysms than men, and after age 65, rupture risk jumps 2.7 times. If you have a family history-two or more close relatives with aneurysms-your risk is four times higher. And if you’ve already had one rupture, your chance of another is over five times greater.
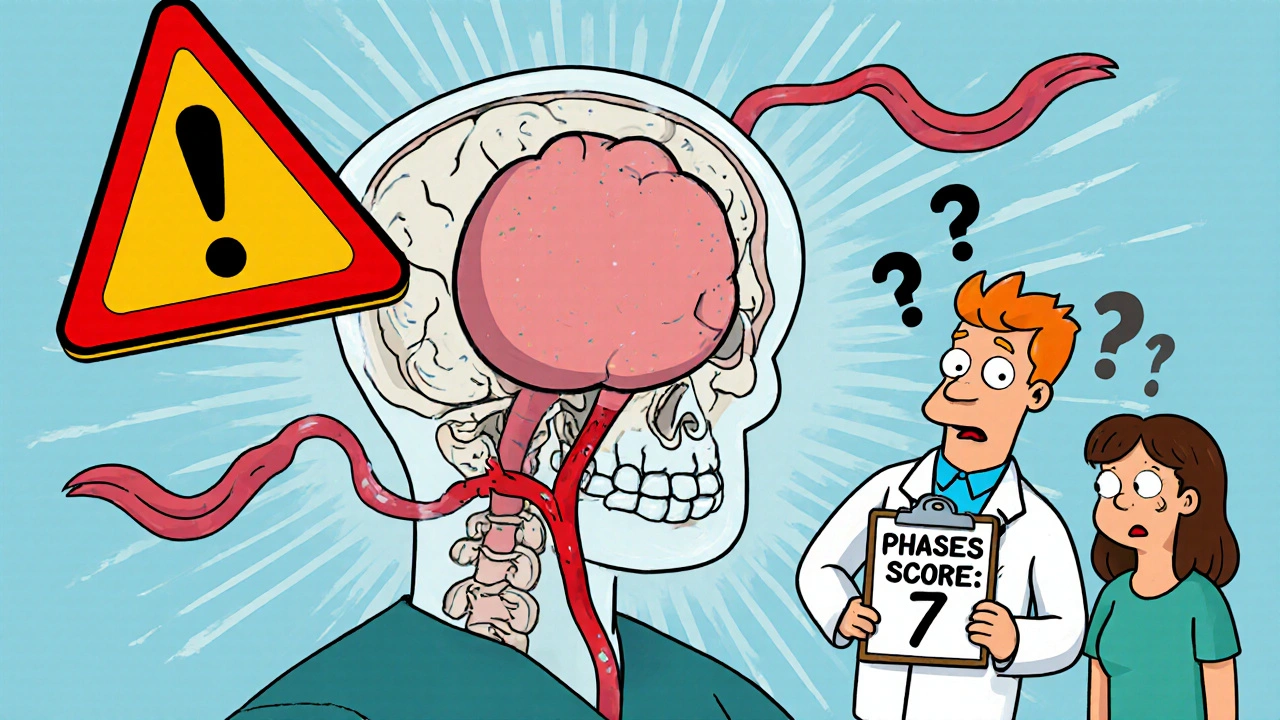
The PHASES Score: A Real-World Tool for Predicting Risk
Doctors don’t guess whether to treat or watch. They use tools. The PHASES score is the gold standard. It combines six factors: your population (where you live), blood pressure, age, aneurysm size, whether you’ve had a previous bleed, and the aneurysm’s location. Each factor adds points. A score of 0-3 means your 5-year rupture risk is only 3%. A score of 9-10? That’s a 45% chance you’ll bleed within five years.
Here’s what that means in practice. A 62-year-old woman with a 6 mm irregular aneurysm in the AComm, who smokes and has high blood pressure, might score a 7. That’s a 15-20% rupture risk in five years. For her, intervention makes sense. But a 45-year-old man with a 3 mm smooth aneurysm in the front of the brain, no smoking, normal BP, and no family history? He might score a 2. His risk is under 5% over five years. Watching with yearly MRIs is the safer path.
The PHASES score isn’t perfect-but it’s the best we have. Each point increase raises the risk by 32%. That’s why doctors don’t just look at size. They look at the whole picture.
Treatment Options: Clipping, Coiling, and Flow Diversion
If your aneurysm needs treatment, you have three main choices: surgical clipping, endovascular coiling, or flow diversion. Each has trade-offs.
Surgical clipping is the oldest method. A neurosurgeon opens the skull, finds the aneurysm, and places a tiny titanium clip across its neck. It’s a direct fix. Success rates are high-95% of aneurysms are completely sealed off. Long-term, 88-92% stay closed forever. But it’s invasive. Recovery takes weeks. Complication rates? Around 4.7% risk of permanent disability and 1.5% risk of death.
Endovascular coiling is less invasive. A catheter is threaded from the groin up to the brain. Platinum coils are packed into the aneurysm, triggering a blood clot that seals it off. Success at six months? 78-85%. Mortality is lower-1.1%-and most patients go home in a day or two. But there’s a catch: 15-16% of coiled aneurysms need retreatment within 10 years because the clot doesn’t hold. Clipping has only a 6% retreatment rate.
Flow diversion is the newest option. It’s not about filling the aneurysm-it’s about redirecting blood away from it. A mesh stent (like the Pipeline Embolization Device) is placed across the artery. Blood flows through the stent, not into the aneurysm. Over months, the aneurysm slowly shrinks and scars over. It’s ideal for large, wide-necked, or complex aneurysms. One-year occlusion rates hit 85.5% with newer platinum-coated devices. But it requires long-term anti-clotting drugs (aspirin and clopidogrel), and there’s a small risk of delayed stroke. Morbidity is slightly higher at 5.2%, but mortality is the lowest of the three-just 0.8%.

Who Gets Which Treatment?
There’s no one-size-fits-all. Your age, health, aneurysm shape, and location guide the decision.
- If you’re under 60 and healthy, clipping is often preferred for its long-term durability.
- If you’re over 70, or have heart or lung problems, coiling is usually safer. Surgery carries a 35% higher complication rate in older patients.
- Wide-necked aneurysms (over 4 mm at the base) are hard to coil. Flow diverters work best here.
- Posterior circulation aneurysms (brainstem area) have 22% higher complication rates with clipping. Coiling or flow diversion are better choices.
- Bifurcation aneurysms-like those at the top of the basilar artery-are now treated with the WEB device. It’s designed to sit right in the middle, with 71% complete closure at one year.
For someone with multiple aneurysms, doctors often treat the highest-risk one first. If you’ve had a prior rupture, treating all visible aneurysms is standard-even the small ones.
What If You Choose to Watch and Wait?
Many small aneurysms never rupture. The UCAS Japan study found that aneurysms under 5 mm in the front of the brain have only a 0.2% chance of bleeding in five years. Even those in the back of the brain (which are riskier) only have a 0.7% risk if they’re under 5 mm.
Conservative management means strict control of blood pressure (under 130/80), quitting smoking (which cuts rupture risk by 54% in two years), and cutting back on alcohol. Annual MRA scans track growth. If the aneurysm grows even 1 mm, treatment is usually recommended.
Don’t underestimate the power of lifestyle. One study showed that quitting smoking had a bigger impact on reducing rupture risk than any surgical technique. Blood pressure control alone reduces rupture risk by over 50%.

What’s Next in Research?
Science is moving fast. The HUNT study identified 17 genetic markers linked to aneurysm formation and rupture. In the future, a simple blood test might tell you if you’re genetically at risk-even before an aneurysm forms.
Machine learning is also changing the game. New models now analyze 42 different features-shape, flow patterns, wall thickness-from a single MRI scan. These models are outperforming PHASES in predicting rupture risk within six months. Some are already being tested in hospitals in Europe and the U.S.
There’s also work on drugs that reduce inflammation in the aneurysm wall. If you have high CRP or IL-6 levels (markers of inflammation), future treatments might target those pathways directly-instead of just blocking blood flow.
Key Takeaways
- Most cerebral aneurysms never rupture-but knowing your risk saves lives.
- Size, shape, location, and lifestyle all matter. A 7 mm aneurysm with irregular shape in the AComm is far more dangerous than a 7 mm smooth one in the front.
- The PHASES score is your best tool for deciding whether to treat or monitor.
- Clipping offers long-term certainty. Coiling offers faster recovery. Flow diversion is best for complex cases.
- Quitting smoking and controlling blood pressure are the most effective ways to lower your risk-no surgery needed.
- Small, stable aneurysms in low-risk locations can be safely watched with yearly scans.
Frequently Asked Questions
Can a cerebral aneurysm heal on its own?
No. Once a cerebral aneurysm forms, it doesn’t disappear or heal on its own. The weakened wall remains vulnerable. In rare cases, a clot may partially fill the aneurysm and reduce blood flow, making it less likely to rupture-but the structure is still there. Without treatment, the risk remains. That’s why monitoring and intervention are critical.
Are there warning signs before a cerebral aneurysm ruptures?
Usually, no. Most ruptures happen without warning. But in about 10-20% of cases, a small leak called a "sentinel bleed" occurs days or weeks before a major rupture. This can cause a sudden, severe headache-often described as "the worst headache of my life." Other signs include blurred vision, neck stiffness, or nausea. If you have one of these headaches, get checked immediately. It could be your only warning.
Is it safe to fly or exercise with an unruptured aneurysm?
Yes, for most people. Moderate exercise like walking, swimming, or cycling is safe and even beneficial-it helps control blood pressure. Avoid heavy weightlifting, intense straining, or activities that spike blood pressure suddenly. Flying is also safe. There’s no evidence that cabin pressure increases rupture risk. Always talk to your doctor about your specific aneurysm size and location before starting a new routine.
How often should I get scanned if my aneurysm is being watched?
Annual MRA (magnetic resonance angiography) scans are standard for unruptured aneurysms under 7 mm with low PHASES scores. If your aneurysm is larger, irregular, or growing, scans may be done every 6 months. If it’s stable for two or three years, some doctors extend the interval to every 18-24 months. Never skip a scan-even if you feel fine. Growth often happens without symptoms.
Can stress or emotional trauma trigger a rupture?
Extreme emotional stress or sudden physical strain (like intense anger, heavy lifting, or sexual activity) can cause a brief but sharp rise in blood pressure. In someone with a high-risk aneurysm, this spike might be the trigger for rupture. It’s not the stress itself-it’s the blood pressure surge. That’s why managing stress and avoiding sudden exertion matters, especially if you have a known aneurysm with a PHASES score over 6.
What’s the long-term outlook after successful treatment?
Successful treatment cuts your 10-year re-rupture risk from 68% to just 2.3%. Most people return to normal life within months. Quality of life is generally better after coiling or flow diversion than after clipping, especially in the first year. Long-term, both approaches offer excellent survival rates. The key is follow-up imaging to catch any recurrence early. With proper care, many live decades without issue.
 Comparing Diabetes Medications: Rybelsus Versus Ozempic Explained by Expert Betul
Comparing Diabetes Medications: Rybelsus Versus Ozempic Explained by Expert Betul
 Transplant Immunosuppression: How Tacrolimus, Mycophenolate, and Steroids Work Together After Kidney Transplant
Transplant Immunosuppression: How Tacrolimus, Mycophenolate, and Steroids Work Together After Kidney Transplant
 How Disulfiram Helps Treat Alcohol-Induced Liver Disease
How Disulfiram Helps Treat Alcohol-Induced Liver Disease
 How to Audit Your Medication Bag Before Leaving the Pharmacy: A Simple 7-Step Safety Check
How to Audit Your Medication Bag Before Leaving the Pharmacy: A Simple 7-Step Safety Check
 Compare Bentyl (Dicyclomine) with Alternatives for IBS and Spasms
Compare Bentyl (Dicyclomine) with Alternatives for IBS and Spasms
Aidan McCord-Amasis
November 16, 2025 AT 00:16Ogonna Igbo
November 16, 2025 AT 02:40BABA SABKA
November 16, 2025 AT 21:37Chris Bryan
November 17, 2025 AT 11:49Jonathan Dobey
November 17, 2025 AT 19:55ASHISH TURAN
November 19, 2025 AT 13:52Ryan Airey
November 20, 2025 AT 06:05Hollis Hollywood
November 20, 2025 AT 08:34Adam Dille
November 21, 2025 AT 05:16Katie Baker
November 21, 2025 AT 16:48John Foster
November 22, 2025 AT 18:54Edward Ward
November 23, 2025 AT 06:34Andrew Eppich
November 24, 2025 AT 05:41