Hemophilia & Alcohol Risk Calculator
Risk Assessment Result
Hemophilia is a hereditary bleeding disorder caused by missing or low levels of clotting factors. People with this condition experience prolonged bleeding after injuries, surgery, or even routine activities. Alcohol is a depressant that the body metabolises primarily in the liver, and its impact on the blood‑clotting system is a common worry for patients and caregivers. This article pulls together the science, the practical risks, and clear guidance so you can make informed choices about drinking while living with hemophilia.
Key Takeaways
- Alcohol interferes with liver function, clotting factor production, and platelet activity, all of which matter for hemophilia.
- Heavy or binge drinking can worsen bleeding episodes and reduce the effectiveness of factor replacement therapy.
- Light, occasional drinking may be safe for many, but it requires monitoring of liver health and treatment timing.
- Stay hydrated, avoid trauma, and keep your haemophilia care team in the loop about any alcohol use.
- Know the signs of dangerous bleeding and when to seek emergency help.
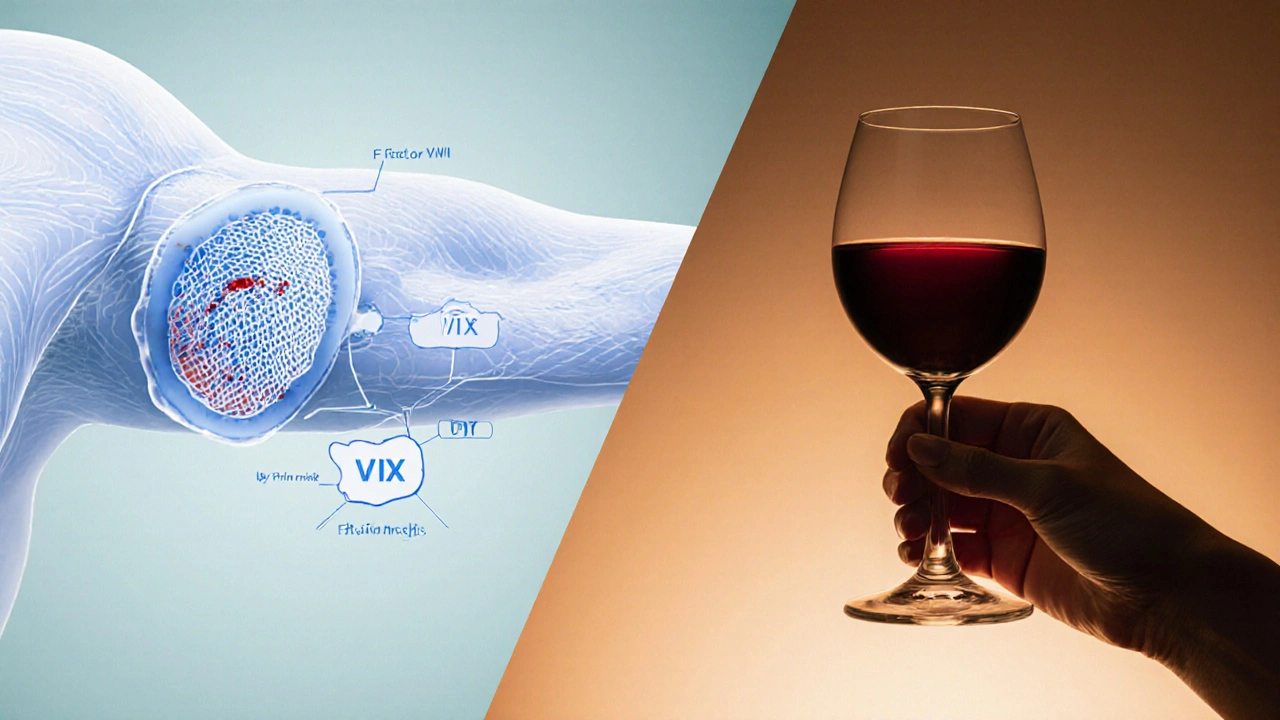
Understanding Hemophilia
Hemophilia comes in two main types: Hemophilia A - a deficiency of factor VIII - and Hemophilia B - a deficiency of factor IX. Severity is classified by the amount of functional clotting factor in the blood:
Patients manage the condition with factor replacement therapy, where missing clotting factors are infused on demand or as a prophylactic schedule. Advances such as extended‑half‑life products and gene therapy are changing the landscape, but the fundamental challenge remains: keeping the clotting cascade functional enough to stop bleeding.
How Alcohol Affects the Body’s Clotting System
The liver produces most clotting factors, including factor VIII and IX. Regular alcohol consumption can lead to fatty liver, inflammation, and eventually cirrhosis, all of which diminish the liver’s ability to synthesize these proteins. In addition, alcohol impairs platelet function, making platelets less sticky and reducing their ability to form the initial plug at a wound site.
Alcohol also influences the balance of fibrinolysis - the process that breaks down clots. Acute intoxication raises tissue‑type plasminogen activator (tPA) levels, which can accelerate clot breakdown. Chronic heavy drinking may also affect the levels of anticoagulant proteins like protein C and S, further tilting the balance toward bleeding.
Specific Risks for People with Hemophilia
When you combine a clotting‑deficient condition with a substance that weakens the clotting system, the risk isn’t just additive - it can be synergistic. The most important concerns are:
- Increased bleeding frequency: Even modest alcohol‑induced platelet dysfunction can turn a minor nosebleed into a prolonged episode.
- Reduced effectiveness of factor replacement: Some oral medications and alcohol metabolites can speed up the clearance of infused clotting factors, meaning you might need higher or more frequent doses.
- Liver disease: Chronic alcohol abuse can cause liver damage that further drops endogenous clotting factor production, compounding the inherited deficiency.
- Medication interactions: Many hemophilia patients also take pain relievers (e.g., ibuprofen) or antifibrinolytics. Mixing these with alcohol raises the odds of gastrointestinal ulcers and internal bleeding.
Because the impact varies with the amount and pattern of drinking, it’s crucial to differentiate between occasional low‑volume consumption and binge drinking.

Safe Drinking Guidelines for Hemophilia Patients
There is no one‑size‑fits‑all rule, but experts agree on a few practical limits.
- Define “light” drinking: Up to one standard drink per day for women and up to two for men - a standard drink in Australia equals 10g of ethanol (≈285ml of full‑strength beer, 100ml of wine, or 30ml of spirits).
- Avoid binge patterns: Consuming more than four drinks in a single occasion sharply raises bleeding risk.
- Stay hydrated: Alcohol is a diuretic; dehydration can thicken blood and aggravate joint bleeding.
- Schedule factor infusions around drinking: If you plan a night out, arrange prophylactic factor coverage before alcohol intake and be prepared to add a dose the next day if you notice increased bruising.
- Monitor liver health: Regular liver function tests (ALT, AST, GGT) should be part of your routine if you drink regularly.
Remember, the most important keyword Hemophilia and Alcohol appears only here for emphasis - you don’t need to binge to enjoy social moments, but you do need a plan.
Managing Alcohol When You’re on Factor Replacement Therapy
Timing matters. Your haemophilia nurse can help set a schedule that aligns with your usual drinking occasions. Here’s a simple workflow:
- Identify your typical drinking day(s) and the expected number of drinks.
- Check the half‑life of your prescribed factor product (e.g., standard factor VIII ~12hours, extended‑half‑life ~18‑24hours).
- Plan a prophylactic infusion 30‑60minutes before your first drink.
- Keep a log of any bleeding events, bruises, or joint pain for the next 48hours.
- If you notice increased symptoms, contact your care team for a possible supplemental dose.
Some patients find it helpful to keep a small “bleed‑kit” on hand - a spare factor vial, ice pack, and a quick‑reference card with emergency numbers.
Lifestyle Strategies Beyond Alcohol
If you’re looking to reduce alcohol without feeling deprived, consider these alternatives:
- Mocktails: Use sparkling water, fresh fruit, and a splash of non‑alcoholic bitters for flavor without ethanol.
- Social activities: Focus on games, sports, or creative workshops where the spotlight isn’t on drinking.
- Support groups: Communities such as the Australian Haemophilia Association often run “safe‑socialising” events.
- Professional help: If you struggle to cut back, a brief counselling session with a psychologist specializing in substance use can make a big difference.
All of these strategies aim to protect your joints, keep your liver healthy, and maintain the effectiveness of your haemophilia treatment plan.
Quick Reference Table: Alcohol Levels vs. Expected Impact
| Level | Standard Drinks per Week | Potential Effects on Bleeding Risk | Recommended Action |
|---|---|---|---|
| None | 0 | No alcohol‑related impact | Maintain current prophylaxis schedule |
| Light | 1‑7 (≤1 per day) | Minimal; monitor liver enzymes | Optional prophylactic factor before drinking |
| Moderate | 8‑14 (2‑3 per day) | Increased platelet inhibition; possible factor clearance | Schedule factor dose + watch for bruising |
| Heavy/Binge | >14 or >4 in one session | Significant bleeding risk; liver strain | Avoid; seek medical advice if consumption occurs |
Frequently Asked Questions
Can a hemophilia patient drink wine at a family dinner?
Yes, a single glass (≈1 standard drink) is generally safe for most patients, provided they have stable liver function and are up‑to‑date on their factor prophylaxis. Keep a log of any bruising after the event and inform your haemophilia nurse.
Does alcohol make factor replacement less effective?
Alcohol can accelerate the clearance of some factor products, especially short‑acting ones. This means a dose might wear off a bit faster, so timing a prophylactic infusion just before drinking can offset the effect.
What are the warning signs that alcohol has caused a bleed?
Look for unexplained bruising, joint swelling, prolonged nosebleeds, gum bleeding, or dark urine. If any of these appear after drinking, treat it as a potential bleed and contact your treatment centre immediately.
Is it safe to mix alcohol with over‑the‑counter painkillers?
Mixing NSAIDs like ibuprofen with alcohol raises the risk of stomach ulcers and internal bleeding, especially in hemophilia. Opt for acetaminophen (paracetamol) at recommended doses, and always discuss pain‑management plans with your doctor.
How often should I get liver function tests if I drink occasionally?
For light, occasional drinkers, an annual check‑up is usually enough. If you exceed light limits or have a history of liver issues, aim for every six months.
Living with hemophilia doesn’t mean you have to give up all social pleasures, but it does require a thoughtful approach to alcohol. By staying informed, planning your factor infusions, and keeping an eye on liver health, you can enjoy gatherings while minimizing bleeding risks. When in doubt, reach out to your haemophilia treatment centre - they’re there to help you balance safety and quality of life.
 Hydration Plans to Protect Kidneys from Nephrotoxic Medications
Hydration Plans to Protect Kidneys from Nephrotoxic Medications
 Tamoxifen and SSRIs: What You Need to Know About Drug Interactions and Breast Cancer Outcomes
Tamoxifen and SSRIs: What You Need to Know About Drug Interactions and Breast Cancer Outcomes
 Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
Understanding the Link Between Heart Arrhythmias and Sudden Cardiac Arrest
 Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
Cranberry Products and Warfarin: What You Need to Know About Bleeding Risk
 Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
Why American Mistletoe is the Perfect Addition to Your Daily Supplement Routine
Chidi Anslem
October 2, 2025 AT 20:31Navigating the balance between social enjoyment and medical caution is a timeless challenge, especially for those living with hemophilia. Alcohol, as a social lubricant, can unintentionally tip that balance when liver function is already compromised. Understanding one's own severity and treatment schedule empowers informed decisions rather than reflexive avoidance. Staying hydrated and planning factor infusions around occasional drinks can reduce unexpected bleeding. Ultimately, a nuanced approach respects both health and quality of life.
Holly Hayes
October 5, 2025 AT 16:31If you're mild you can sip wine but dont be lazy about checking your liver.
Penn Shade
October 8, 2025 AT 12:31From a pharmacokinetic standpoint, ethanol can accelerate the clearance of short‑acting factor concentrates, effectively shortening their half‑life. This means that a dose administered before drinking may wear off sooner than anticipated, potentially leaving a gap in protection. Patients with severe hemophilia should therefore schedule infusions after the drinking episode, not before. Monitoring post‑drink factor levels with a simple point‑of‑care test can provide reassurance. Consultation with the hemophilia treatment centre remains the gold standard.
Jennifer Banash
October 11, 2025 AT 08:31Esteemed colleagues and fellow sufferers, permit me to underscore the gravitas of intermixing ethanol with haemophilic pathology.
The hepatic metabolism of alcohol, when perturbed, can precipitate a diminution of endogenous clotting factor synthesis, a circumstance most dire for those already deficient.
Moreover, the attendant vasodilatory effects exacerbate capillary fragility, heralding insidious bleeding episodes.
One must, therefore, exercise the utmost circumspection in the consumption of even modest libations.
The sanctity of one's health ought to supersede the fleeting allure of convivial revelry.
I implore each reader to engage in pre‑emptive dialogue with their haematology specialist prior to any indulgence.
Stephen Gachie
October 14, 2025 AT 04:31Philosophically, the act of drinking can be viewed as a ritual of surrender to temporality, yet the physiology of hemophilia demands steadfast vigilance. Proper grammar in medical documentation mirrors the precision required in timing factor replacement. When alcohol enters the equation, the metabolic interplay becomes a paradoxical dance of risk and reward. Hence, a measured approach-light consumption, scheduled infusions, and liver monitoring-offers a rational compromise.
Sara Spitzer
October 17, 2025 AT 00:31Let me be clear: the literature overwhelmingly supports caution for heavy drinkers with hemophilia, but the data on light occasional use is sparse. I skimmed the recent guidelines and they barely touch on moderate intake, which feels like a half‑hearted concession. In practice, clinicians often rely on anecdotal experience, a lazy shortcut that can mislead patients. Still, if you keep your liver enzymes in check and avoid traumatic contexts, a single glass may not be catastrophic.
Jennifer Pavlik
October 19, 2025 AT 20:31Remember to tell your care team about any drinks you have, even if it’s just one glass, so they can help you stay safe.
Jacob Miller
October 22, 2025 AT 16:31While I respect personal choice, overlooking the bleed risk after a night out can be reckless, especially when you’re on a tight prophylactic schedule. It’s not about policing behavior, but about pointing out a blind spot that many ignore. A gentle reminder: schedule factor doses after drinking, not before, to keep the safety net intact.
Anshul Gandhi
October 25, 2025 AT 12:31The intersection of hemophilia management and alcohol consumption is often shrouded in misinformation propagated by both anecdotal forums and selective scientific reporting. First, ethanol induces hepatic cytochrome P450 enzymes which can alter the metabolism of recombinant clotting factors, potentially reducing their efficacy. Second, alcohol-mediated platelet inhibition compounds the intrinsic clotting deficiency inherent in hemophilia, creating a double jeopardy scenario. Third, chronic heavy drinking can lead to fibrosis and cirrhosis, further compromising the liver’s ability to produce residual factor VIII or IX. Fourth, binge episodes are notorious for causing sudden spikes in blood pressure, which may precipitate joint bleeds in vulnerable patients. Fifth, the timing of factor replacement relative to alcohol intake is critical; infusing too early may result in premature clearance, while infusing too late leaves a therapeutic gap. Sixth, several observational studies have hinted at a modest increase in spontaneous bleeds among moderate drinkers, though confounding variables limit definitive conclusions. Seventh, the psychological aspect cannot be ignored; the social pressure to drink can lead individuals to conceal their consumption from healthcare providers. Eighth, concealment obstructs accurate monitoring of liver enzymes and clotting factor levels, thus impairing personalized treatment plans. Ninth, the safest recommendation remains individualized: patients should undergo baseline liver function tests before any regular alcohol use. Tenth, those with a history of liver disease should limit intake to no more than one standard drink per month, if at all. Eleventh, education on recognizing early signs of bleeding-such as unexplained bruising or joint swelling-remains paramount for all patients, regardless of drinking habits. Twelfth, emergency protocols should be reviewed with the care team, ensuring rapid access to factor concentrates should an alcohol‑related bleed occur. Thirteenth, peer support groups can provide valuable shared experiences, but the advice given must always be vetted against clinical guidelines. Finally, open communication with your haemophilia treatment centre before planning any social events involving alcohol is the cornerstone of risk mitigation.
Emily Wang
October 28, 2025 AT 07:31Your thorough breakdown is a beacon for anyone tangled in the haze of mixed messages. I’m especially grateful for the reminder about emergency protocols; many overlook that until it’s too late. Let’s all commit to sharing this knowledge with our circles, because awareness saves lives. Keep the momentum going, and stay safe.
Hayden Kuhtze
October 31, 2025 AT 03:31Ah, the lofty philosophy of sipping wine while your blood refuses to clot-truly a pastime for the avant‑garde. One might suggest a monocle and a poetry book, but alas, the liver insists on being the buzzkill. Nonetheless, your balanced musings are a charming distraction from the grim reality.
Craig Hoffman
November 2, 2025 AT 23:31Just to add – if you do decide to have that glass, make sure you’ve got your factor on hand and keep an eye on any weird bruises you might notice later.
Terry Duke
November 5, 2025 AT 19:31What an inspiring cascade of insights, and it’s wonderful to see everyone building on each other’s knowledge, because together we create a safety net that’s stronger than any single recommendation, so keep sharing, keep caring, and remember that informed choices lead to brighter, bleed‑free gatherings!